The experimental treatment uses a genetically modified virus to deliver a missing gene into the cerebrospinal fluid of children with giant axonal neuropathy (GAN).
Article by/Media contact: Tom Hughes, 984-974-1151, Tom.Hughes@unchealth.unc.edu
Thursday, June 25, 2015
University of North Carolina (UNC) School of Medicine researchers have developed an innovative, experimental gene transfer-based treatment for children with giant axonal neuropathy (GAN).
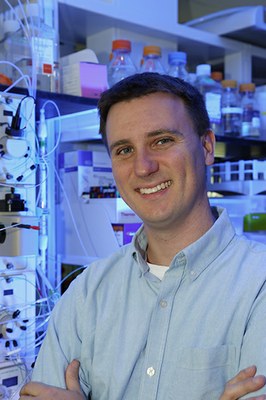
Researchers led by Steven J. Gray, PhD, assistant professor in the Department of Ophthalmology and a researcher in UNC’ s Gene Therapy Center and Carolina Institute for Developmental Disabilities, developed the experimental treatment in studies conducted at UNC. Gray’s work in this area was funded almost entirely by Hannah’s Hope Fund, a charity founded by the parents of Hannah Sames, an 11-year-old girl with giant axonal neuropathy (GAN), to support the development of a treatment and cure. This extremely rare genetic disorder causes children to gradually lose the ability to balance themselves, move their muscles and to feel certain sensations. Most children born with GAN do not survive beyond their early 20s because of progressive impairment of their ability to breath.
The treatment approach developed at UNC uses a genetically modified virus called AAV to deliver a missing gene, the gigaxonin gene (scAAV9/JeT-GAN), into the cerebrospinal fluid of children with GAN. The therapeutic viral vector to be used in each of these injections is prepared at the UNC Vector Core Human Applications Laboratory.
A clinical trial of this approach is now underway at the National Institute of Neurological Disorders and Stroke (NINDS) of the National Institutes of Health (NIH) in Bethesda, Maryland. The first patient was enrolled in May. This is the first gene delivery approach directly into the spinal fluid in order to treat an inherited neurological disorder, and is expected to pave the way to developing treatments for many other related diseases.
Gray chose to focus his career on this rare genetic condition after meeting Hannah, who is the same age as his own daughter, Aubrey.
“This has been a coordinated and committed effort between Hannah’s Hope and UNC to drive a treatment forward for GAN. Hannah’s Hope is a truly amazing community that provides a constant source of inspiration. Our goal has always been to bring hope to the families affected by this devastating disease, and we are proud to be taking the first step to making a GAN treatment a reality,” said Dr. Gray. “We are greatly appreciative of NIH/NINDS for partnering with us on this life-saving mission. This trial is the first in history to deliver gene therapy through the spinal fluid to test the potential to achieve broad treatment of the spinal cord and brain (central nervous system or CNS). It is a momentous step forward, and we’re already seeing clear application of this approach to treat other diseases studied in my lab.”
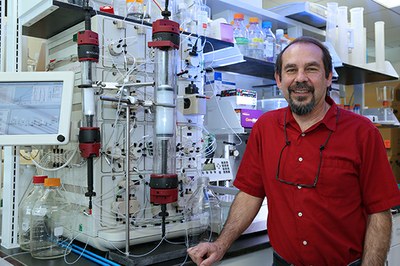
Gray serves as an associate investigator on the trial as does R. Jude Samulski, PhD, director of the UNC Gene Therapy Center.
“After 30 years of focusing on optimizing successful gene delivery, it is very rewarding to finally see these approaches being tested for some of the unmet clinical needs caused by these terminal genetic disorders,” Samulski said. “This specific study represents a culmination of years of basic research from the UNC Gene Therapy Center and that primarily of Steve Gray’s team coupled with clinical expertise at the NIH. More importantly, this journey for me has personally been a truly rewarding one that started seven years ago with a parent knocking on the office door asking if we could ‘help save her child’, to last week’s gene therapy administration; a remarkable and humbling journey that I’m privileged to be a part of.”
(The above excerpted from Thomas Hughes’ article on School of Medicine News, of same title, published June 25, 2015.) Read the full School of Medicine News article by Thomas Hughes here.