
Dr. Scott Commins describes alpha-gal allergy, which scientists believe is triggered by a tick bite and can cause a reaction to red meat. Dr. Commins talks about the symptoms of a reaction, how one can be tested for the allergy, and changes in diet recommended for patients who have alpha-gal. Dr. Scott Commins is an Associate Professor of Medicine in the Division of Rheumatology, Allergy, and Immunology and UNC Thurston Arthritis Research Center.
– Dr. Scott Commins
Ron Falk, MD: Hello, and welcome to the Chair’s Corner from the Department of Medicine at the University of North Carolina. Today’s episode is part of our series focused on food allergy, and we will be discussing an interesting allergy called alpha-gal.
We welcome Dr. Scott Commins who is an Associate Professor of Medicine in the Division of Rheumatology, Allergy, and Immunology and UNC Thurston Arthritis Research Center. Dr. Commins is an allergist and immunologist and he sees patients in the UNC Allergy and Immunology Clinic. Dr. Scott Commins is one of the world’s leading experts in this field of alpha-gal, and has helped many patients who have this condition, and is actively investigating the cause of this allergy in his laboratory. Welcome, Dr. Commins.
Scott Commins, MD, PhD: I’m excited to be here. Thank you for the invitation.
Alpha-Gal And Its Discovery
Falk: What on earth is this word alpha-gal, and what does that describe?
Commins: Alpha-gal is a carbohydrate or sugar that has two galactose sugars linked in an alpha-1-3 linkage.
Falk: Okay, you lost me. Say that to me in lay-speak, please.
Commins: So, there are two galactose sugars that are in line with each other in a certain configuration in space that chemists call an “alpha configuration” and the technical name is this galactose-alpha-1,3-galactose. We call that “alpha-gal” for short.
Falk: On the surface of so many proteins, probably all proteins, there are carbohydrate moieties of one kind or another and galactose is one of those.
Commins: Correct.
Falk: Sialic acid would be another, but there are several sugars that coat proteins, and what you’re describing then is a sugar—a galactose—that is present on some proteins.
Commins: Absolutely. One of the fascinating things about this alpha-gal sugar is that as humans, we don’t have alpha-gal, and many sugars are ubiquitous. However, alpha-gal is different in the sense that non-primate mammals—cows, sheep, pigs, cats, dogs—all have alpha-gal. As humans, we actually don’t have that sugar, but we make an immune response to it.
Falk: That would be one of the potential reasons why we as humans, if we eat foods that are derived from the species you just described, we could potentially develop a reaction to it. And like in so many allergies and autoimmune diseases, when most people can eat these kinds of animal products, some individuals become reactive to it. Is that right?
Commins: That is correct, and that is what the focus of my research and clinic is largely centered upon.
Falk: Why some people suddenly react to meat.
Commins: Exactly.
Falk: Tell us a little about the history of how alpha-gal allergy was discovered, and what was your role in that discovery process?
Commins: I think it’s a fascinating history, and it actually starts in the oncology, or cancer world. In fact, there is some indication that when Martha Stewart went to prison, it involved alpha-gal. Her role in this essentially is that a company creating a cancer drug produced it in a mouse cell line. These mouse cells, as we discussed earlier, that would be one of the species that makes alpha-gal. These mouse cells decorated this cancer drug with their alpha-gal sugar. So, when this therapeutic was given to people who were allergic to alpha-gal, they reacted, and they reacted in a very serious way—life-threatening, anaphylactic-type reactions. The company began to find that this was happening throughout the southeast, but not in California or New York. In fact, UNC was one of the early sites that identified that their patients who were receiving this medication were reacting on the order of one in five or one in four on first infusion of this medication.
Falk: One in five, or one in four patients.
Commins: Correct. Nearly a quarter of them were reacting the first time getting this medication. Reacting meaning getting hives, itching, loss of blood pressure, true kind of anaphylaxis. The company began to know that this was happening in a certain geographic region but not in others. The story goes that perhaps they weren’t as forthcoming with some of this data, but eventually they did have to tell the FDA. Allegedly, Martha’s stock broker found out that the company was moving towards telling the FDA and her stock was sold at the appropriate time. That’s the cancer side of alpha-gal. Essentially the way the story goes is these patients were reacting because they had developed an allergic response to alpha-gal.
That was work done in Dr. Platts-Mills’s lab in the University of Virginia, where I was training as an allergy and immunology fellow. When I joined the lab, they had just published this work, but what we were seeing in the clinic, was patients who were telling us, “Hey doc, I think I’m allergic to beef (or pork, or lamb) but it doesn’t happen every time, and it happens in a delayed way.” This sort of flew in the face of conventional food allergy at that point. But because we had this knowledge of the distribution of alpha-gal being in these lower mammals, and we had a test because Dr. Platts-Mills had just published this work with the cancer therapeutic, we thought, “Maybe we should run their serum sample for this alpha-gal allergy.” Sure enough, that opened the Pandora’s box. In 2009, we then published 24 cases who had reported they had delayed allergic responses to beef, pork or lamb.
Falk: Prior to that, somebody who thought they were having an allergic response to a slice of beef, would have thought they were…nutty.
Commins: Absolutely. It’s an excellent point, because prior to that, allergic reactions to beef were almost case-reportable in every instance. There’s actually a publication of 12 patients who had a beef allergy from the early 1980’s, and there really just wasn’t much else in the literature related to red meat and allergic responses to it.
Falk: How does the story of tick bite then get mixed with what you found from these patients?
Commins: At the time, we were fascinated by the idea that there was a delayed allergic response, but we had no understanding or indication why—these were adults, safely having eaten beef for forty or fifty years and all of a sudden developing the allergic response. We started thinking about what was it about perhaps about the geography of the southeast, or what was it about these patients who might have a common history, to give us a clue. We tried lots of different things, but ultimately it came down to two observations.
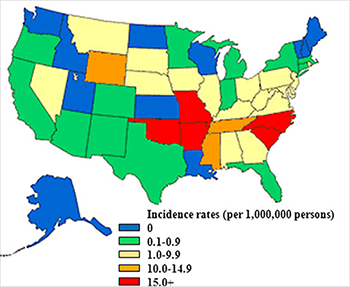
One was a map—a map of Rocky Mountain Spotted Fever, if you look at the incidence on the CDC maps. The incidence of that really played quite well, almost overlaid—with the map of our allergic responses to beef in an alpha-gal allergy type of way. Secondly, one of the technicians in our lab at the time had been hiking and he got several tick bites and developed a new onset allergy to beef.
Falk: What a chance moment in time—sorry for the guy.
Commins: Indeed. It does show you that serendipity, it favors the prepared mind. So here we were investigating this and absolutely stumbled upon the idea that tick bites perhaps could be doing this. We essentially called back our patients we had been enrolling in our meat allergy study, and this was largely my role—and began asking them questions related to their tick bite history, exposure, settings where they were, and began to piece the puzzle together.

Falk: How do you know it’s a tick bite? What’s the evidence?
Commins: We’re actively working on this. If you go in the woods, how do you know that it’s a tick bite and not a mosquito or poison ivy? Ultimately, we’re working on a mouse model where we can inject tick extract into a certain type of mouse. These mice produce the same allergic response to alpha-gal that our patients do. That so far has been the best indication.
Delayed Allergic Reaction
Falk: Why does a person with alpha-gal allergy experience a reaction several hours after eating red meat, instead of like a peanut allergy which can happen immediately?
Commins: There’s two main answers to that—the first of which is that alpha-gal is a sugar. You mentioned peanut. So much of what we know about allergy in general centers on proteins. Part of this, we believe that the response to the sugar is in some ways a weaker response than we might see for proteins. Secondly, the most severe reactions that we have heard about happen with fattier forms of meat. The digestion of fat is very different from the way that sugars or proteins are absorbed. The digestion of fat is a process that takes three to hours to deliver fat to the bloodstream.
Falk: You think that may participate in some of the delayed reaction?
Commins: We think, particularly, that the absorption of fat and the time that it takes for that to occur begins to explain the delay. We’ve done some challenges where we bring our patient volunteers in and feed them sausage. When we do that, we can find that the appearance of alpha-gal in the bloodstream is actually delayed three or four hours. So there’s something about the processing of meat, and we think fat makes a good candidate that begins to explain the delay.
Falk: It’s a need for the digestion of the meat that then participates in triggering this process.
Commins: We think that’s true, and it’s supported by the idea that when these cancer patients were getting their medication…
Falk: They were getting it by vein.
Commins: That’s right, and the reactions happened right away.
Falk: This whole concept of a delayed reaction implies, as you have nicely described, a delay or some sort of alteration in digestion. In your mind’s eye, this is associated with fat absorption. How does that actually work? Walk me through—food goes into your mouth, down the esophagus, into the stomach—lots of acid in the stomach, food starts to digest, goes into the small intestine, gets modified, large intestine, and then out. Where’s the problem? Where’s the digestion that is slowed up? It must be in a cellular mechanism.
Commins: You’re correct that the cellular mechanism is important here. When it comes to fat absorption, fat essentially has to be broken down and digested—we think of it as a trimer—three fat molecules are hooked together generally. Those three molecules have to be separated—this is where the word “triglyceride” comes from…You have to then break these three fat molecules apart so that they become singular. Then they are essentially reshaped into a sphere. This sphere then gets pulled across the intestine, for lack of a better way to think about it. Then it enters the lymphatics—these are our immune response, our lymphatics move our immune cells around to our lymph nodes. Fat, as it gets absorbed through the digestive process, actually ends up in the lymphatics that encirculate our intestines. Fat then moves through the lymphatics and ultimately empties into the thoracic duct, which is a lymphatic opening in our neck. This whole process takes three-ish hours, and it really fits with the reactions when they’re delayed.
Falk: That’s one explanation, you can imagine there could be other reasons for a delay as well—that’s a conjecture.
Symptoms of a Reaction

Falk: What is the reaction that patients get three or four hours later? What does it feel like?
Commins: Their reactions often start with itching, particularly the palms and soles. We have patients tell us repeatedly that their hands begin to itch and turn red. Then they often get systemic hives all over their skin. Then the process seems to snowball. It starts with skin and itching and hives and redness, perhaps swelling, then often tell us that they feel light-headed so we think their blood sugar is dropping. Often there is a gastrointestinal component to this as well—so really severe abdominal cramping, diarrhea, nausea, vomiting—all the hallmarks of an anaphylactic allergy reaction that you might see in a child who has a milk, egg or peanut allergy.
Falk: Unhappily then, you can imagine someone who has a burger or steak for dinner, would think everything is fine, would go to bed, and what would wake them up?

Commins: Typically the itching. You have described a very prototypical allergic reaction for the alpha-gal allergy, which is certainly very different from the typical allergic response. This idea that patients experience allergic reactions after midnight is really in keeping with the alpha-gal allergy and unlike most other food allergies.
Falk: People are then woken up, out of sleep, itching away… What are they supposed to do?
Commins: We tell folks to take Benadryl if you have it. If you had an EpiPen or epinephrine auto-injector, then that would be a good time to use it, but most people don’t have an auto-injector at home. We ask them to take antihistamine such as Benadryl because most folks will have something along those lines, and then begin to activate the emergency response cascade: whether that’s calling 9-1-1 or if you’re close enough and you can get to the emergency department quickly.
Falk: So, this really is a “Let’s go to the emergency room” kind of moment.
Commins: It is, in large time because we have no idea at that moment, when you wake up with hives and itching, “Is this going to progress and become a life-threatening response, or is this going to evolve and I’m going to get a little bit of GI upset but otherwise be fine?”
Falk: For the first time this happened to a patient, it would be really a scary phenomenon. You would have no clue what was amiss, because more than likely you’d think, “I ate something and it doesn’t agree with me and now I’m not feeling well.”
Commins: Absolutely. I have countless patients who have recalled passing out in the bathroom at midnight, 1 AM, at their initial allergic reaction.
Tick Bites and Alpha-Gal
Falk: Let’s come back to the tick for a moment. Tick bites are common for anyone who likes to be outside, if you like to garden or hike. In the southeastern portion of the United States your chances of getting a tick bite are pretty large. Let’s now say someone has gotten a tick bite and they’ve listened to this podcast, they’re not going to start worrying that that tick is going to induce an alpha-gal allergy. How long after being bitten by a tick do you think would it take for somebody to figure out they may be having a problem?
Commins: We think it takes on the order of four to six weeks. Some of that is, as you know, the immune response takes time, but then you have to eat the right meal in a time period after you’ve developed that immune response. In general, this is on a month-ish side.
Falk: A month or six weeks and of course that person has no clue that they’ve been bitten by a tick. Would you like if they had kept the tick if they could have?
Commins: It’s a great thought and we are hopeful that we’re going to be able to have some research goals around the actual tick. At the moment, I don’t have a particular thing to do with the tick, but we are in discussions, so stay tuned.
Falk: Stay tuned – for tick harvesting.
Testing for Alpha-Gal
Falk: Now—the patient comes to the emergency room, or they’re worried about this process, what kind of test do you do? How do you prove that the person has an alpha-gal allergy?
Commins: Right, so in allergy land the proof is two-fold. One is clinical history – so does their story fit? Secondly, it’s a positive blood test. That same blood test that we talked about earlier related to the cancer drug, and defining those patients who are allergic to alpha-gal, that’s actually the same test that we use for our patients who’ve developed the alpha-gal meat allergy.
Falk: So the reason then why someone would want to get tested, is that it would confirm whether or not they had this allergy. How good is the test?
Commins: The test is quite sensitive.
Falk: That means it picks up a positive reaction in lots of folks. The question then, is if it’s positive, does that mean you have the allergy? How specific is it?
Commins: It is not very specific. The answer is nuanced because this is different for us in Chapel Hill than it would be in Denver, Colorado in large part because the geography matters when it comes to tick bites. Our data indicate that the test is not as specific as we want to be and we are working to try to create a better test. It’s an excellent screening test.
Falk: A positive test should make one think that one could have an alpha-gal allergy, but it doesn’t prove it, because there are individuals who are positive in this test who can eat all the meat they want and have no problems.
Commins: That’s absolutely true. This is a nuance that we have in allergy land in general – so if we took a hundred kids and tested them all for peanut allergy, ten would be positive. Of those ten, one would truly be allergic to peanuts. We have a similar phenomenon when it comes to the alpha-gal test. In some ways, I think it’s a marker for tick bites, and perhaps other bites as well, but only a small fraction of people who test positive truly develop allergic responses after eating mammalian meat.
Falk: It is then really the symptoms—the story—that a person tells you about the allergy symptoms that are more indicative of the allergy than is the test.
Commins: Correct, and because of that, we don’t advocate getting tested just because you’ve had a tick bite.
Falk: Now for those of us who like red meat, especially the males in my family, the idea of no longer being able to eat red meat would be devastating. Can you get desensitized?
Commins: At the moment, no. We’re working on that. The good news, however, is that in many cases, we don’t find this is a life-long immune response. It may go away. It appears in many patients to be transient. They may have 18-24 months without red meat, and then we begin to follow their blood test level—which is another reason to have the blood test done—it typically trends down over time. When appropriate, we begin to reintroduce red meat.
Diet Changes and Considerations
Falk: How do you then counsel somebody who has this allergy? What do you tell them to avoid?
Commins: Initially, we ask people to strictly avoid red meat—beef, pork, lamb, this would include venison, bison, buffalo—anything essentially that has hooves and walks on four legs, we ask them to avoid. They can certainly eat chicken, turkey and fish, but we often leave dairy in their diet if they can tolerate it. Ice cream, however, comes up again and again as something that contains a fair amount of milk fat and as we talked about earlier, I worry a lot about the fat content of things. Ice cream is one that after red meat, we typically find, if people are still having reactions, it typically involves dairy and we ask them to remove ice cream from their diet.
Falk: Oh my goodness. You can’t eat red meat, you can’t eat ice cream, and you’re stuck on vegetables forever—is that what you’re gently trying to suggest?
Commins: Well, hopefully it’s not a forever thing.
Falk: But it could be.
Commins: It could be.
Falk: How do you tell patients, then, who go out to eat, how do they know that they’re not going to have some red meat product slipped in, even in a sauce?
Commins: I’m glad you asked that, because initially we would tell people to have some card that explained alpha-gal allergy, and I think that was really unfair to waiters and waitresses, because no one really knows much about alpha-gal in the restaurant community, so we have changed our advice. We ask patients to lead with, “I’m allergic to beef, pork, lamb.” Chefs and wait staff understand that. Typically, people do find in their local community places where they will be able to prepare their foods either separately or without beef or pork fat. In the south, we love vegetables that contain a ham hock or are supplemented with lard, and we have to be careful about those dishes as well.
Falk: There are a number of pharmaceutical agents or bio-derived devices, heart valves for example—heparin, the drug that is used in patients who have blood clots, for example. Heparin is derived from the animals you’re describing. Heart valves are, to a certain extent, are pork-derived valves. What about those people?
Commins: That’s a great question, and not one that we were necessarily thinking about in 2009 when we thought this was simply a food allergy. We have been aware of and seen patients who have had anaphylaxis to heparin, particularly heparin that is used to dissolve clots, or to anticoagulate someone, thin their blood during an operation—a little different from the heparin that you might get just to prevent your DVT or blood clot from being immobile. This is massive doses of heparin given intraoperatively, and we have seen folks that have had allergic responses, they are alpha-gal allergic and have anaphylaxis from heparin. We have published a series of three cases of patients who developed anaphylaxis after having a pig valve put in their heart.
Clearing up Misconceptions About Alpha-Gal
Falk: There are abundant comments on the Internet about meat allergy. There are all sorts of funny and perhaps misleading comments: “It’s only one kind of tick…It’s only the lone star tick…There are some sources of red meat that are safer than others…It’s always an anaphylactic reaction.” Help us dispel some of what is out there.
Commins: We are probably guilty of advancing this idea that lone star ticks were the only cause.
Falk: Are you the culprit?
Commins: I probably share some blame in this. So, initially that was because we were describing this in the southeast, and it really fit with the distribution of the lone star tick. I do maintain that in the south and in the east—Long Island, for instance as well—I think most of these allergic responses are due to the lone star tick. That doesn’t account for problems people are having in Australia, people we know about in southern Sweden, in Europe where they have this same allergy but they don’t have the lone star tick. So, one of the myths as you described, is that lone star ticks are the only cause, and that’s clearly not true.
Secondly, we do hear from some folks that they can eat certain kinds of beef, so cows that are grass fed or free range or organic. At the end of the day, a cow is a cow, and they all make alpha-gal. Perhaps there are some cuts of meat, that as they are leaner, they may create less of a risk for a reaction, but at the end of the day, I’m convinced that if you eat enough of an organic, grass-fed, free-range cow, and you have the alpha-gal allergy, you’re going to have a reaction.
Falk: Those reactions can be severe enough that it wouldn’t be worth that experiment.
Commins: Not in my mind.
Future of Alpha-Gal Research
Falk: What kind of research are you doing right now? Where is this research going?
Commins: We have several projects, but I think the one that is most important at the moment is to define what it is about the tick that creates a risk or causes this allergy. There’s two main reasons for that. One is because it’s immunologically fascinating, and it’s a paradigm-changing type of thing. We, in the allergy field have seen a massive rise in allergic eczema, asthma, eosinophilic esophagitis—allergic disease is on the rise, and this is another one of those types of entities. We really need to understand what it is about the tick that creates this risk.
I think the second part of this—you alluded to desensitization earlier—we treat people who are allergic to bee venom or wasp venom with allergy shots to prevent future reactions, so if we can define what it is from the tick that causes this, then I believe we can develop allergy shots that use the protein or salivary component from the tick.
Falk: To desensitize a person.
Commins: Correct.
Falk: Thank you, Dr. Commins for all of this wonderful information.
Commins: My pleasure.
Falk: Thanks so much to our listeners for tuning in. Next week, we’ll talk some more about alpha-gal with Dr. Commins and with one of his patients and we will get to hear about this individual’s experience with having alpha-gal. If you enjoy this series, you can subscribe to the Chair’s Corner on iTunes or like the UNC Department of Medicine on FaceBook. Thanks so much.