Education
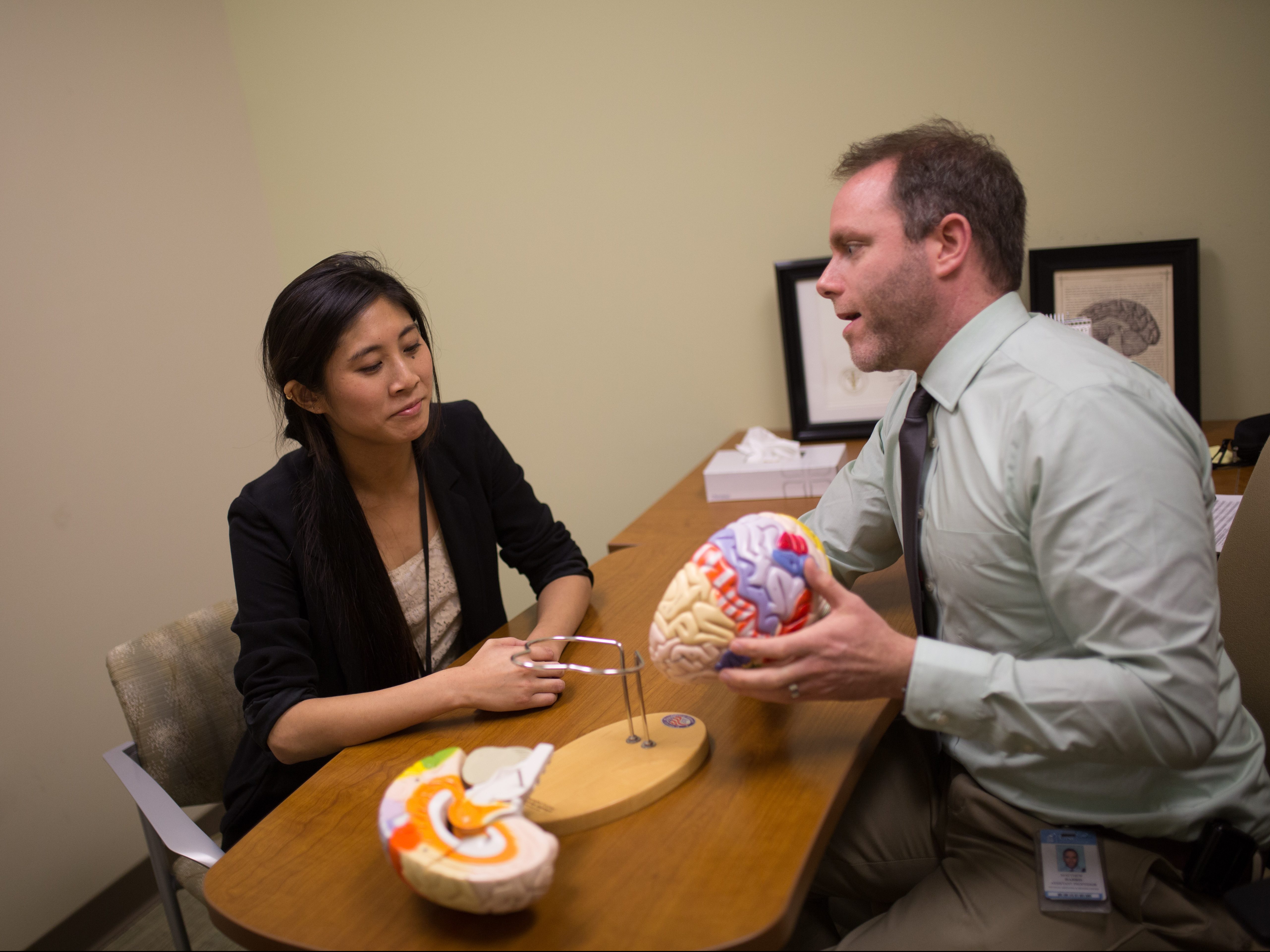
UNC PM&R is dedicated to educating tomorrow’s health care professionals and academic researchers. Our residency program provides a vigorous educational experience coupled with strong support for resident wellness, in state-of-the-art facilities. Along with our residency program, we also offer rotations for medical student education and shadowing experiences. Our T32 Fellowship program provides support for two to three years of pre- or post-doctoral research training leading to impactful Complementary and Integrative Healthcare (CIH) research careers.
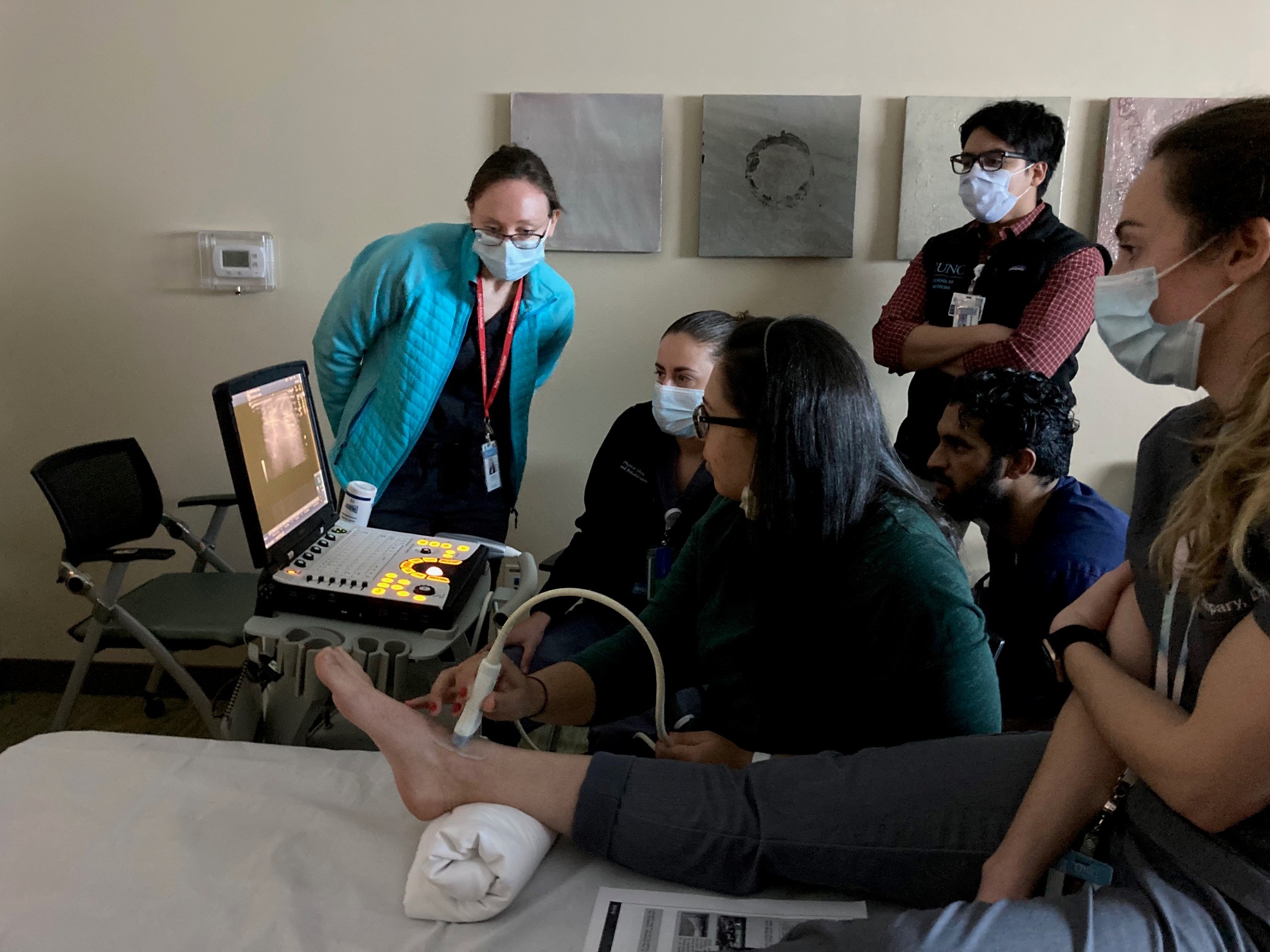
Residency Program

The UNC Physical Medicine and Rehabilitation ACGME-accredited residency training program aims to help medical graduates develop into outstanding practicing physiatrists.