Clinical Training

Clinical training takes place at UNC Medical Center, UNC Pulmonary Clinics at Eastowne and Panther Creek, and UNC Hillsborough Hospital. We take pride that UNC is a public, academic institution operated by and for the people of North Carolina. We support the system’s mission to provide high quality patient care, educate health care professionals, advance research and provide community service.
People from all 100 North Carolina counties and throughout the Southeast are patients at our hospital facility. Additionally, we care for people at UNC outpatient practices and clinics. Training within this large and dynamic health care system provides our fellows with robust clinical exposure to a diverse patient population, a wide range of common and uncommon pulmonary diseases, and breadth of critical illness.
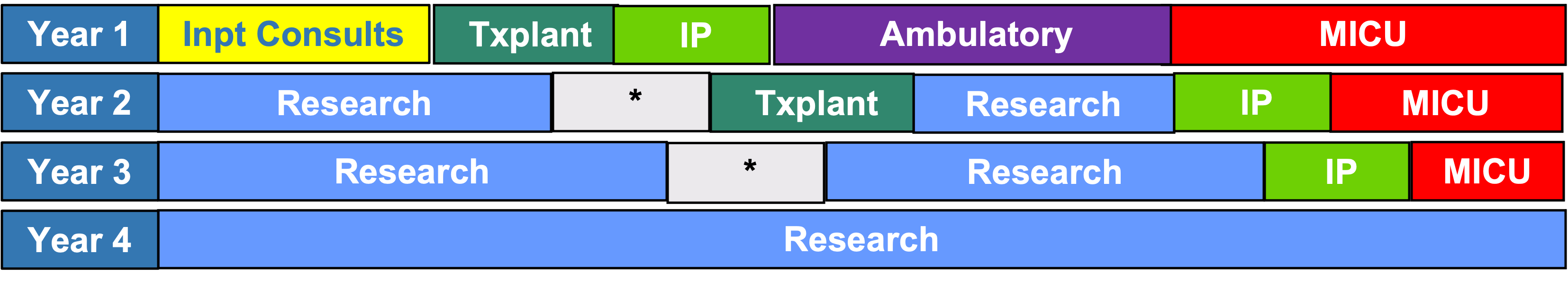
The first year of fellowship is dedicated to clinical training. During the latter years of fellowship, 75% of the time is dedicated to a research training program tailored to the specific career interests of the individual fellow, and 25% of the time for continued clinical training during which time clinical skills are advanced, solidified, and fine-tuned.
Clinical training during the first year of fellowship is divided among rotations in: Ambulatory Pulmonary, Inpatient Pulmonary Consults, Pulmonary Transplant, Interventional Pulmonary and the Medical Intensive Care Unit. During years two and three, fellows rotate through the MICU, complete their non-MIC critical care electives and spend more time on the Interventional Pulmonary Service advancing their procedure skills. Additional electives can be arranged on an individual basis based upon fellow interests.
 Ambulatory Pulmonary Medicine
Ambulatory Pulmonary Medicine
Fellows participate in various pulmonary subspecialty clinics during their ambulatory rotations including Multi-disciplinary Thoracic Oncology Program (MTOP), Interstitial Lung Disease, Cystic Fibrosis, Bronchiectasis, COPD, Asthma, Sleep Medicine, Vasculitis and Pulmonary Hypertension.
The fellow gains experience in outpatient procedures such as bronchoscopy, advanced bronchoscopy (EBUS, navigational), pleural procedures, right heart catheterization and cardiopulmonary exercise testing.
Medical Intensive Care Unit
 UNC Hospital has a 30 bed Medical Intensive Care Unit (MICU) that is staffed by dedicated critical care pharmacists, nurses, respiratory therapists, nutritionists and internal medicine residents and interns. Fellows are an integral part of the MICU team during their training. During fellowship they will learn to lead a multidisciplinary team in the management of critically ill patients admitted to a quaternary medical ICU.
UNC Hospital has a 30 bed Medical Intensive Care Unit (MICU) that is staffed by dedicated critical care pharmacists, nurses, respiratory therapists, nutritionists and internal medicine residents and interns. Fellows are an integral part of the MICU team during their training. During fellowship they will learn to lead a multidisciplinary team in the management of critically ill patients admitted to a quaternary medical ICU.
The first-year fellow guides the resident team in the evaluation and management a wide spectrum of diseases including hemorrhagic shock from gastrointestinal bleeding, septic shock, cardiogenic shock from massive pulmonary emboli, respiratory failure, liver failure, renal failure, metabolic emergencies, drug overdose and others. Management of respiratory failure and the mechanical ventilator is a primary focus of MICU rotation. The first-year fellows perform all bronchoscopies in ICU patients, learn airway management/intubation, and assist the housestaff with the placement of central lines, arterial lines, paracenteses, and thoracenteses. With the Interventional Pulmonary team, they may perform percutaneous tracheostomy and chest tube placement. Skills in critical care ultrasound and physiology are acquired during this rotation.
Second and third year fellows continue to develop their skills and act as the “pre- Attending” physician on their service, directing teaching rounds with the housestaff and supervising patient care.
Non-Medical Critical Care
During the 2nd and 3rd years of fellowship, the fellow participates in two week rotations for the total of 12 weeks on the surgical services caring for critically ill surgery patients at UNC Hospitals. These rotations permit the fellow to gain experience with critically ill patients in the surgery/trauma ICU, cardiothoracic ICU, neurosurgery ICU, burn ICU unit, and cardiac intensive care unit.
Interventional Pulmonary
During all three years of fellowship there is opportunity to rotate on the Interventional Pulmonary service. This incorporates inpatient consults, procedures and outpatient clinic with associated procedures. Fellows’ procedure experience will occur in a graduated fashion with junior fellows focusing on the basics of flexible bronchoscopy, thoracentesis, ultrasound-guided pigtail chest tubes and senior fellows gaining experience with more advanced diagnostic bronchoscopy and pleural procedures.
Lung Transplant
The lung transplant program at UNC is one of the oldest in the US and performs an average of 15 transplants yearly. The pulmonary fellow is a valuable member of the multidisciplinary team during their transplant rotations. This incorporates inpatient transplant consults, outpatient transplant referral and post-transplant clinic, and procedures such as bronchoscopy. Fellows are exposed to a broad range of patients and diseases, in a multi-disciplinary setting, and thus are exposed to the many facets of pulmonary, cardiothoracic surgical, infectious disease and transplant critical care experience in patients who have “end stage” lung disease and all its associated complexities.
Bronchoscopy
Fiberoptic bronchoscopy is the dominant procedure of the pulmonologist. Skills in bronchoscopy are obtained at orientation and on each rotation during the first year of training. Training begins with a bronchoscopy course during orientation bootcamp, and with simulation in the Procedural Simulation Laboratory. The Fellow becomes skilled in airway inspection, bronchoalveolar lavage, endobronchial biopsy, transbronchial biopsies and transthoracic needle biopsy using endobronchial ultrasound (EBUS). Fellows also have the opportunity to acquire skills in electromagnetic navigation bronchoscopy. Bronchoscopies are performed in our state-of-the art bronchoscopy suite, the OR, and in the intensive care units of UNC Hospitals. Each fellow in our program progresses through competency-based training in bronchoscopy graduating with ample experience and skills.
Continuity Clinic
The outpatient Pulmonary Specialties Clinic at UNC is located at the Eastowne Medical Office Building, about 3 miles from the main UNC campus. Additional outpatient clinics are also located at Panther Creek (general pulmonary) and the Main Hospital (Transplant, Interventional Pulmonology, and Thoracic Oncology).
Eastowne MOB is the main site for outpatient care for UNC’s Department of Medicine. In 2021, construction was completed on this six-story building that houses clinics for nearly all internal medicine subspecialties. In addition, there is an onsite retail pharmacy, imaging center, laboratory, infusion center, ample meeting space, and the Clinical Research Unit. Five dedicated PFT labs are available for same-day pulmonary function testing, including spirometry, lung volumes, six-minute walk tests and methacholine challenges. At Eastowne, patients are seen in a number of pulmonary specialty clinics staffed by expert providers in COPD, non-CF bronchiectasis, interstitial lung disease, sarcoidosis, cystic fibrosis, alpha-1-antitrypsin disease, asthma, pulmonary hypertension, and general pulmonology.
A major focus of the Department of Medicine currently is the development of multidisciplinary subspecialty clinics to enhance care delivery to patients with specific diseases. For example, under development is a joint Pulmonary/Rheumatology Interstitial Lung Disease clinic, ensuring patients have access to all necessary providers in one physical location. Other multidisciplinary clinics that currently exist or are in development at Eastowne include:
- Vasculitis
- Cystic Fibrosis (pulmonary, endocrine, and psychiatry)
- Pulmonary Hypertension (pulmonary and cardiology)
- Severe asthma (pulmonary and allergy/immunology)
- Sickle Cell (pulmonary and hematology)
Fellows maintain a continuity clinic at Eastowne throughout all three years of fellowship training; continuity clinic occurs weekly during the first year of fellowship and may move to biweekly in years 2/3 depending on research focus. In continuity clinic each week, fellows evaluate new referrals, often from other pulmonologists, and maintain their own panel of follow-up patients with a wide variety of respiratory diseases. During clinic days, fellows will interact with and learn from dedicated precepting pulmonary faculty, specialty nurses, respiratory therapists and a clinical pharmacist. After three years of training in this longitudinal pulmonary clinic, fellows are well-prepared to practice outpatient pulmonology in an academic or clinical setting. Trainees with a particular interest in an area of excellence (cystic fibrosis, pulmonary hypertension, etc.) can choose to have a longitudinal experience in these dedicated subspecialty clinics in their second or third year of fellowship.
Clinical Conferences
To complement the hands-on training, a number of didactic and interactive conferences are available. Clinical conferences are attended by fellows during their research and clinical years. Clinical conferences include the following:
- Clinical Case Conference
- Core curriculum conference
- Critical Care Boot Camp
- Interstitial Lung Disease Conference/Journal Club
- Interventional Pulmonary Conference/Journal Club
- Journal club
- Lung transplant conference
- Multidisciplinary Thoracic Oncology Program conference
- Radiology Conferences
- Research Conference
In addition, multiple other conferences are available in the School of Medicine and Department of Medicine in particular fields or in general internal medicine.