About IBD
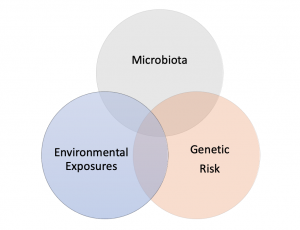
Inflammatory bowel disease or “IBD” encompasses two major conditions: ulcerative colitis and Crohn’s disease. Both lead to chronic inflammation of the mucosal lining of the intestine, though each has specific characteristics. Currently we don’t know what causes the inflammation, but one hypothesis postulates that several factors are involved in causing IBD. These factors include a specific genetic background, the environment including nutrition, and the intestinal microbiota (see Figure below). According to this theory intestinal inflammation develops in genetically susceptible individuals after an initial environmental or infectious trigger. Once inflammation starts it’s amplified by the intestinal microbiome.
What is Ulcerative Colitis?
The term “-itis” refers to inflammation, thus ulcerative colitis is inflammation of the colon. Unlike Crohn’s disease, ulcerative colitis or “UC” affects only the colon (the large bowel) and causes inflammation and ulceration of the lining of the colon. Different amounts of the colon may be affected but the inflammation is always continuous and always involves the rectum. The inflammation can include the rectum alone (“proctitis”), extend from the rectum up to the left colon (“left-sided colitis”), or involve the entire colon (“pancolitis”).
Symptoms of ulcerative colitis often include diarrhea, blood in the stool, and abdominal or rectal pain. Patients often have “urgency” meaning they have to get to a bathroom right away. They may also feel like they haven’t completely emptied their bowels. Although diarrhea is the most common symptom of ulcerative colitis, some patients may actually experience constipation. Other symptoms include fever, weight loss, or low blood counts (anemia). Inflammation can also affect other parts of the body and cause rashes, joint pains, or eye changes.
What is Crohn’s Disease?
Crohn’s disease can affect anywhere along the gastrointestinal tract from the mouth to the anus. Unlike ulcerative colitis the inflammation is not always continuous and there can be areas of normal bowel in between areas of inflamed bowel. Crohn’s disease can cause inflammation of just the intestinal lining or can cause deeper inflammation. Deep inflammation can affect the full thickness of the bowel wall and can lead to complications of Crohn’s disease. These complications include stricture (or narrowing) of the bowel, abscess (or infection), and fistulae which are abnormal connections between two parts of the body. Fistula can occur between two parts of the intestine, between the intestine and the skin, or between the intestine and other nearby organs like the bladder or vagina.
Symptoms of Crohn’s disease can be more variable than ulcerative colitis and depend on what part of the bowel is affected. If the colon is involved then symptoms can be very similar to ulcerative colitis with diarrhea and passage of blood or mucus. If the small intestine is involved then symptoms may include diarrhea and vitamin or nutrient deficiencies due to decreased absorption in the inflamed intestine. If there is a narrowing or blockage in the bowel then patients may have crampy abdominal pain, nausea, vomiting, weight loss, or decreased bowel movements. If Crohn’s disease affects the skin near the anus then patients can have drainage, pain, or swelling of the perianal area. Like ulcerative colitis, Crohn’s disease can cause inflammation of other parts of the body. The most common are inflammation of the joints (arthritis) or skin. Inflammation can also affect the eyes. Rare sites of inflammation include the liver and bile ducts, pericardium (sac surrounding the heart), pancreas, and blood (leading to blood clots).
What is Indeterminate Colitis (also known as IBD-Unclassified [IBD-U])?
Sometimes your doctor may use the term “indeterminate colitis” or IBD-U. This means that we’re not quite sure if the inflammation of the colon is from Crohn’s disease or ulcerative colitis. About 5%-10% of patients with IBD carry the diagnosis of indeterminate colitis or IBD-U. It doesn’t make a big difference because treatments for both are similar and with time things may become clearer.
Diagnosis
IBD is diagnosed by a combination of patient history, imaging, blood work, stool analyses and endoscopic evaluation (usually colonoscopy and/or upper endoscopy) If a patient has symptoms suggesting IBD a diagnostic work-up is initiated. Your doctor may order blood work to look for signs of inflammation or specific deficiencies (such as iron deficiency) and also exclude an intestinal infection with stool cultures. Different types of imaging like a CT or MRI can also identify inflammation in the intestine. Generally, an upper endoscopy or colonoscopy can be done to look directly at the bowel and take biopsies of the affected tissue. Sometimes a small pill camera is used to look at the small bowel that is beyond the reach of our endoscopes. Putting together all of the testing can help your doctor make a diagnosis of inflammatory bowel disease.
Treatment
Many treatments for Crohn’s disease and ulcerative colitis overlap. Below are some of the common medications used to treat inflammatory bowel disease. These medications may be used alone or in combination. Your doctor may choose which medication(s) to use based on type of disease, severity, and other medical conditions you may have. Goals of treatment are to decrease inflammation and improve symptoms and quality of life. For more information on specific medications please see the Crohn’s and Colitis Foundation IBD Medication Guide.
Medications
- Aminosalicylates (e.g. mesalamine, balsalazide, sulfasalazine): these are oral and topical medications used to treat mild-to-moderate ulcerative colitis. They have anti-inflammatory properties to reduce tissue inflammation. They are well-tolerated and have very few side effects. Your doctor should monitor blood work annually on these medications.
- Corticosteroids: oral, topical, and intravenous formulations are available. Steroids generally treat inflammation quickly and are used to achieve remission at initial diagnosis or during a disease flare. Steroids are not used for long-term maintenance of remission due to side effects including sleep disturbance, weight gain, poor blood sugar control, altered bone health, and increased risk of infections.
- Immunomodulators (azathioprine, 6-mercaptopurine, methotrexate): these are oral and subcutaneous medications used to treat moderate-to-severe ulcerative colitis and Crohn’s disease. These medications block the body’s immune response in order to decrease inflammation. Often, they are used in combination with biologic medications and can also help prevent your body from becoming immune to these types of medications. These medications can cause bone marrow suppression and elevated liver enzymes, so blood work is monitored every three months on these medications. Some of these medications have been associated with malignancy including lymphoma and non-melanoma skin cancers. The overall risk of malignancy is quite low. We recommend regular sunscreen use and annual skin exams with a dermatologist while on these medications.
- Biologic Medications (e.g. infliximab, adalimumab, certolizumab, golimumab, vedolizumab, ustekinumab): these are subcutaneous and intravenous medications used to treat moderate-to-severe ulcerative colitis and Crohn’s disease. These target specific receptors to suppress the immune system and decrease inflammation in the gut. Some work systemically (throughout the body) and some are gut-specific. These medications are generally well-tolerated but do carry some risks similar to immunomodulators.
- Small Molecule Inhibitors (e.g. tofacitinib): these are a type of oral medication approved for moderate-to-severe ulcerative colitis which has been unresponsive to other therapies. These oral medications are also currently evaluated for patients with Crohn’s disease. These drugs target specific molecules inside a cell to turn off inflammatory cascades.
Surgery
Some forms of IBD may require surgery due to stricture or narrowing, infection, fistula formation, or severe inflammation unresponsive to medications. The UNC Multidisciplinary Center is designed to facilitate a team approach to your care before, during, and after surgery.
IBD and Pregnancy
Most IBD medications are safe to continue throughout pregnancy and breastfeeding. The American Gastroenterological Association has information and guidelines for treatment of IBD during pregnancy at the IBD Parenthood Project. Our providers are here to help if you are pregnant or thinking about becoming pregnant.