Diagnostic Procedures
What will the physician do to determine the type and extent of a patient’s disease?
He will inform you, the patient, that “diagnostic procedures” are now necessary, that you should undergo certain types of examinations. As a first step, he will conduct a physical examination of your entire body, particularly the abdomen and also the rectum. He will gather information by palpating the outer surface of the body, by listening with the stethoscope and by tapping over hollow organs. This will help discover whether the skin, mucous membranes, eyes or joints show signs of disease. When examining the abdomen, it may be possible to determine the exact site of pain and the physician will be able to learn much about the condition of the liver and the activity of the bowel. In examining the anus, he will be able to recognize inflammation and, by gently examining the rectum with his finger, possibly find traces of blood.
The physician will then obtain blood and urine samples in order to perform certain laboratory tests, including erythrocyte sedimentation rate (time required for settling of suspended red blood cells), the number of white and red blood cells and platelets (the “blood count”), the protein content of the blood (protein electrophoresis and C-reactive protein [CRP]) and other special laboratory tests such as iron, electrolytes, vitamins (particularly vitamin B12), folic acid and trace elements, such as zinc. Together, these tests help determine whether general signs of inflammation, absorption disorders (reduced or inadequate uptake of nutrients from the bowel) or bleeding are present. The urine tests help evaluate the kidneys and urinary tract
If the results of these tests confirm the suspicion of an inflammatory bowel disease, further examinations will be necessary to determine the type of the individual patient’s disease as well as its location and extent in the gastrointestinal tract. An important fact is that the diagnosis of an inflammatory bowel disease can only be made if all test and test results of endoscopy, of the evaluation of biopsies, of imaging studies and of the laboratory and microbiolgical tests are pointing all in this direction. The diagnosis based on a singular test, e.g. blood test is not possible.
In determining the extent of the digestive tract affected by any IBD, it is crucial to determine the exact site(s) of inflammation. A number of methods are available, including endoscopy and radiography.
Endoscopy
Endoscopy uses an optical instrument to directly see the inner surface of hollow organs. Entering through the mouth, it is possible to examine the esophagus, stomach and duodenum. Entering through the anus, the physician can check the rectum, the entire length of the colon and usually the last few centimeters of the small bowel, also known as the terminal ileum. The endoscope is a flexible, tube-like instrument with a diameter of 9–12 mm. These high-precision instruments contain an optical system integrated into their tip connected to the outer end by a fiber-optic cable consisting of thousands of fine glass fibers. This fiber-optic cable transmits light into the organ being examined and conveys the image onto a television monitor. The endoscope has a separate channel through which a thin instrument can be introduced. This instrument, known as a biopsy forceps, can be used to obtain tissue samples for examination.

 Endoscopy permits the examiner to look directly at the mucous membrane of the digestive tract. Normal tissue can usually be easily distinguished from inflamed areas. In addition, tissue samples can be taken from affected areas and examined using microscopic methods, also known as histological examination. This direct examination under the microscope of samples of mucous membrane permits determination of whether inflammation is present, how severe it is, and what type of inflammation it is. Thus, it can establish the diagno sis of IBD and usually (≥ 90%) can differentiate between ulcerative colitis and Crohn’s disease.
Endoscopy permits the examiner to look directly at the mucous membrane of the digestive tract. Normal tissue can usually be easily distinguished from inflamed areas. In addition, tissue samples can be taken from affected areas and examined using microscopic methods, also known as histological examination. This direct examination under the microscope of samples of mucous membrane permits determination of whether inflammation is present, how severe it is, and what type of inflammation it is. Thus, it can establish the diagno sis of IBD and usually (≥ 90%) can differentiate between ulcerative colitis and Crohn’s disease.
Endoscopic examination of the stomach is also known as gastroscopy. For gastroscopy, the optical instrument is introduced through the mouth and advanced through the esophagus into the stomach and duodenum. This examination must be done in a fasting state in order that the food content of the stomach will not interfere with inspection of the mucous membrane. The examination is painless; however, it is associated with unpleasant sensations of pressure in the neck during introduction of the instrument and in the upper abdomen. This discomfort can be significantly reduced by the administration of appropriate medication.
In colonoscopy , which involves endoscopic examination of the bowel, the endoscope is introduced through the anus and advanced up the entire length of the colon to the entrance of the small bowel. Once the junction between the small bowel and colon (the ileocecal valve) is passed, the terminal portion of the small bowel can also be examined. Colonoscopy requires more intensive preparation. Patients are not permitted to consume any solid food for 24 hours prior to the examination. On the day before the examination, the patien t may eat breakfast but for lunch, only clear broth is allowed. In the afternoon, the patient must also consume a suitable irrigating solution (3–5 liters) in order to cleanse the bowel. Various solutions are available with different tastes. After this, only mineral water or tea is allowed.
Colonoscopy may be painful, particularly when there are inflammation-related adhesions in the abdomen. Patients may be given injections that help relax them and relieve pain, making the examination tolerable.Proctoscopy is the simplest and least invasive endoscopic method. It involves examination of the distal rectum and covers the last 5 –10 cm above the anus. More commonly, however, patients undergo sigmoidoscopy, a procedure permitting inspection of the distal 30–40 cm of the colon. Prior to both procedures, the bowel is cleansed with an enema. Then, the examiner inserts either a short, stiff tube (rectoscope) or a short flexible endoscope (sigmoidoscope). Both procedures offer the capability of obtaining tissue samples (biopsies). Both methods are sufficient for evaluation and follow up of inflammation in the area of the rectum.
Endoscopic pictures of ulcerative colitis



Endoscopic pictures of Crohn’s disease



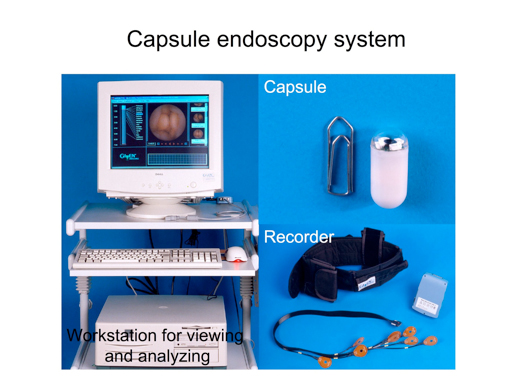
Capsule Endoscopy and Balloon Endoscopy
Two relatively new endoscopic techniques include capsule endoscopy and double or single balloon endoscopy. Capsule endoscopy makes it possible for the first time to examine the small bowel in its entirety. This was formerly possible only indirectly using radiological methods. Unfortunately, capsule endoscopy, while permitting us to inspect the small bowel, lacks the capacity for tissue biopsy. The method is also not suitable for examination of the stomach or colon. For patients with Crohn’s disease, capsule endoscopy is associated with a certain risk because, although the endoscopy capsule is relatively small, it may still become retained in an area of stenotic bowel. In the worst case, this can result in acute intestinal obstruction, requiring immediate surgery. At present, capsule endoscopy has not become an established option in the diagnosis of inflammatory bowel diseases and should only be used when answers to very special questions are being sought. Future studies will determine the value of capsule endoscopy for therapeutic decision-making in areas in which this method can provide additional information.
 The second new endoscopic technique is double balloon endoscopy, which uses a specially designed endoscope permitting examination of significantly longer stretches of the small bowel than has been possible using conventional endoscopes. Unlike capsule endoscopy,double balloon endoscopy has the capacity to obtain tissue specimens from the small bowel, as well as to stop bleeding and remove polyps. It is possible that, in the future, this technique will make it possible to dilate narrowed areas of the bowel (stenoses) that to date require surgery. As with capsule endoscopy,the benefit of this method for patients with confirmed inflammatory bowel diseases must be evaluated in further studies. You may now be asking yourself whether all of these examinations must be performed. You can relax. The more extensive array of methods is normally required only to confirm the initial diagnosis of a disease and to determine its extent and severity.
The second new endoscopic technique is double balloon endoscopy, which uses a specially designed endoscope permitting examination of significantly longer stretches of the small bowel than has been possible using conventional endoscopes. Unlike capsule endoscopy,double balloon endoscopy has the capacity to obtain tissue specimens from the small bowel, as well as to stop bleeding and remove polyps. It is possible that, in the future, this technique will make it possible to dilate narrowed areas of the bowel (stenoses) that to date require surgery. As with capsule endoscopy,the benefit of this method for patients with confirmed inflammatory bowel diseases must be evaluated in further studies. You may now be asking yourself whether all of these examinations must be performed. You can relax. The more extensive array of methods is normally required only to confirm the initial diagnosis of a disease and to determine its extent and severity.
The choice of method depends on individual factors, particularly the patient’s current physical condition. Endoscopy and radiological methods can be used to complement each other. Usually, endoscopy is used to examine the more easily accessible segments of the digestive tract, since radiation exposure is avoided and it is normally possible to obtain tissue samples (biopsy) from suspicious areas for microscopic evaluation. In order to properly evaluate the small bowel, as well as in cases in which the presence of fistulae or severe narrowing (stenosis) in the colon are suspected, it will not be possible to avoid radiologic examinations. The exact analysis of fistulae and/or abscesses can often be done using a special ultrasound examination of the rectum (endosonography) or with MRI.
In endosonography, an ultrasound transducer head is introduced through the rectum as in proctoscopy or sigmoidoscopy. This permits ultrasound examination of underlying tissue and determination of possible fistula formation.
Radiological examinations represent another option for examining the digestive tract. One method makes use of a solution (contrast medium) that is not penetrated by x-rays to show the contours of the esophagus, stomach, small bowel or colon. In cases of IBD, examination of the small bowel is particularly important. In such cases, the small bowel can be examined using a special method called small bowel follow through (SBFT). The patient drinks first contrast media, which is then propelled by the motions of the stomach and the small bowel throughout the gastrointestinal tract. Sometimes a tube is passed through the stomach into the duodenum, which permits direct application of a diluted contrast medium in the small bowel. The segments of the small bowel between the duodenum and colon, which are not accessible to endoscopy, can be examined using this method.
New possibilities have become available for imaging the small bowel using computed tomography (CT) or magnetic resonance imaging (MRI). Both methods generate “slices” of selected regions of the human body (see picture below) . The CT is particularly useful in the search for abscesses (encapsulated collections of pus), which are frequently encountered in IBD.
Radiology
Radiological examinations represent another option for examining the digestive tract. One method makes use of a solution (contrast medium) that is not penetrated by x-rays to show the contours of the esophagus, stomach, small bowel or colon. In cases of IBD, examination of the small bowel is particularly important. In such cases, the small bowel can be examined using a special method called small bowel follow through (SBFT). The patient drinks first contrast media, which is then propelled by the motions of the stomach and the small bowel throughout the gastrointestinal tract. Sometimes a tube is passed through the stomach into the duodenum, which permits direct application of a diluted contrast medium in the small bowel. The segments of the small bowel between the duodenum and colon, which are not accessible to endoscopy, can be examined using this method.
New possibilities have become available for imaging the small bowel using computed tomography (CT) or magnetic resonance imaging (MRI). Both methods generate “slices” of selected regions of the human body (see picture below) . The CT is particularly useful in the search for abscesses (encapsulated collections of pus), which are frequently encountered in IBD.

How does the physician monitor the course of inflammatory bowel diseases?
It is important for you, the patient, to understand that, while both ulcerative colitis and Crohn’s disease are chronic diseases of the bowel that can become and remain inactive, careful medical attention is crucial for monitoring and control of your disease. This means regular visits to the physician: at least twice a year is recommended, even when you are free of symptoms. If, however, drugs are required to control your disease, follow-up examinations should be done at least every three months. Beside a physical examination including palpation of the abdomen and examination of the bowel, patients undergo blood tests that help identify signs of inflammation or of nutritional deficiencies.
During an acute disease episode or flare-up, patients do not necessarily have to re-undergo the entire battery of tests. In those cases in which symptoms are significantly different than in earlier disease phases, however, it may be helpful to re-assess the extent of the disease, since changes may occur, possibly necessitating a modification in treatment strategy. In ulcerative colitis, this is particularly important in cases in which the initial extent of the disease did not involve the entire colon. In Crohn’s disease, significant changes in symptoms usually necessitates re-examining both the small bowel and colon in order to exclude the presence of fistulae, stenoses or other complications. If, however, there are no changes and the disease remains inactive, these invasive methods are not necessary. Patients who have suffered from ulcerative colitis for a long period of time (more than 10 years), however, should undergo regular colonoscopy (once a year is recommended) in order to exclude the development of malignant tumors in the bowel. This is particularly important in extensive colitis.