What causes Inflammatory Bowel Diseases (IBD)?
Despite numerous studies, the actual cause of the inflammatory bowel diseases remains elusive. It is likely, however, that these chronically recurring episodes of inflammation in the human bowel are related to a complex interaction between various environmental factors and a hereditary predisposition for these diseases.
In recent years, research has identified various sites (genes) within the human genome that may be associated with these diseases. 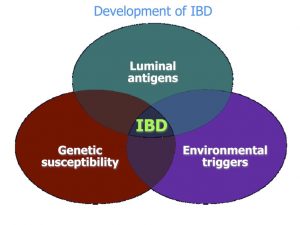 To date, changes in multiple genes (nearly 40) have been discovered that play a greater or lesser role in the development of Crohn’s disease and ulcerative colitis. The most important of these changes of the genetic material in patients with Crohn’s disease was identified by scientists in 2001. They showed that changes (mutations) in the so-called NOD2/CARD15 gene significantly increase the risk of developing Crohn’s disease. Such changes appear to be at least partially responsible in about 20% of all Crohn’s patients for the occurrence of this disease. On the other hand, it is clear that this hereditary predisposition alone cannot lead to the outbreak of disease: this requires the presence of further, as yet unidentified factors. Changes in the NOD2/CARD15 gene are found in about 4% of individuals, who do not develop this disease. This means that genetic predisposition requires the action of other, still unknown factors in order for an affected individual to actually develop the disease. These factors may include viruses or bacteria, changes in nutritional behavior or the consumption of certain preservatives or other food additives, as well as disturbances of the body’s own immune defense system or the intestinal barrier (see figure “Development of IBD”). To date, no definitive evidence has been found to prove a connection between these factors and the development of inflammatory bowel disease. It is, however, very probable that environmental factors play a role. Crohn’s disease, for example, is much more common in Western industrial nations than in other regions of the world. On the other hand, it is very unlikely that IBD is due to an underlying infectious disease – hence, infecting other persons with the disease is not possible.
To date, changes in multiple genes (nearly 40) have been discovered that play a greater or lesser role in the development of Crohn’s disease and ulcerative colitis. The most important of these changes of the genetic material in patients with Crohn’s disease was identified by scientists in 2001. They showed that changes (mutations) in the so-called NOD2/CARD15 gene significantly increase the risk of developing Crohn’s disease. Such changes appear to be at least partially responsible in about 20% of all Crohn’s patients for the occurrence of this disease. On the other hand, it is clear that this hereditary predisposition alone cannot lead to the outbreak of disease: this requires the presence of further, as yet unidentified factors. Changes in the NOD2/CARD15 gene are found in about 4% of individuals, who do not develop this disease. This means that genetic predisposition requires the action of other, still unknown factors in order for an affected individual to actually develop the disease. These factors may include viruses or bacteria, changes in nutritional behavior or the consumption of certain preservatives or other food additives, as well as disturbances of the body’s own immune defense system or the intestinal barrier (see figure “Development of IBD”). To date, no definitive evidence has been found to prove a connection between these factors and the development of inflammatory bowel disease. It is, however, very probable that environmental factors play a role. Crohn’s disease, for example, is much more common in Western industrial nations than in other regions of the world. On the other hand, it is very unlikely that IBD is due to an underlying infectious disease – hence, infecting other persons with the disease is not possible.
The role of psychological factors remains controversial. While psychic stress may, under certain circumstances, provoke an acute flare-up of an existing disease, it is not the underlying cause of inflammatory bowel disease.
We also do not know the exact reason why many patients with IBD also suffer from inflammatory changes in other organs, such as the joints, skin or eyes. One explanation is an overreaction on the part of the body’s immune defenses to either invading microbes or even the body’s own tissues. This, however, has not yet been proven.
 On the other hand, the causes of many other complications of these bowel diseases are known (see figure “Complications outside of the bowel”). For example, the reduced absorption of vitamins and some trace elements (minerals) in patients with IBD is responsible for symptoms such as night blindness, deafness, changes in taste sensation, vulnerability to infection, hair loss, infertility (in men), growth retardation (in children) and certain skin changes frequently seen in these patients. Anemia may be caused by iron deficiency, by loss of blood from the bowel or by vitamin B12 malabsorption. A reduced uptake of bile acids in the small bowel and an increased absorption of bilirubin in the colon is responsible for the increased risk of gallbladder stones, while kidney stones may result from the increased loss of water.
On the other hand, the causes of many other complications of these bowel diseases are known (see figure “Complications outside of the bowel”). For example, the reduced absorption of vitamins and some trace elements (minerals) in patients with IBD is responsible for symptoms such as night blindness, deafness, changes in taste sensation, vulnerability to infection, hair loss, infertility (in men), growth retardation (in children) and certain skin changes frequently seen in these patients. Anemia may be caused by iron deficiency, by loss of blood from the bowel or by vitamin B12 malabsorption. A reduced uptake of bile acids in the small bowel and an increased absorption of bilirubin in the colon is responsible for the increased risk of gallbladder stones, while kidney stones may result from the increased loss of water.
In both main types of IBD, serious complications such as acute ballooning of the bowel (“toxic megacolon”) or perforation, the formation of a hole in the wall of the bowel, may occur in a few patients. Peritonitis, the inflammation of the membranous lining of the abdomen, and intestinal obstruction or paralysis (ileus) may result. These are life-threatening conditions requiring immediate hospital admission and often emergency surgery. Extensive intestinal hemorrhage occurs most often in patients with ulcerative colitis.

Stenoses caused by inflammation or scar tissue formation and fistulae between the bowel loops and other organs are direct consequences of Crohn’s disease (see figure “Stenosis in the ascending colon”).