An increasing focus on high-value care and the implications around length of stay (LOS) has the potential to profoundly impact both patients and hospital systems. As hospitals face lower patient capacities and increasing costs, studies show an understanding of the factors that contribute to LOS can improve the management of LOS.
 Nick Shaheen, MD, MPH, chief of the division of gastroenterology and hepatology, champions the newest Value-Care Action Group (VCAG) project in the department of medicine, led by Shifali Arora, MD, assistant professor of medicine in gastroenterology.
Nick Shaheen, MD, MPH, chief of the division of gastroenterology and hepatology, champions the newest Value-Care Action Group (VCAG) project in the department of medicine, led by Shifali Arora, MD, assistant professor of medicine in gastroenterology.
“This is a combined hospital and department effort and an opportunity where improvements will greatly benefit GI and our hospital colleagues. Dr. Arora is making great progress with a large focus on communication. Improvements in endoscopy workflows will ensure a high level of patient care progresses efficiently and reduces length of stay.”
Arora explained the VCAG project in the following questionnaire.
How did this VCAG project come about?
“As the general GI inpatient service has become busier, the division was looking for ways to change the infrastructure to allow for better communication, dedicated time for education and improved efficiency. As part of that, we started to look at our inpatient endoscopy workflows to re-evaluate that as well. The goal is to reduce the number of endoscopy cases that get bumped, thereby potentially reducing hospital LOS.”

What new processes will be put in place?
“The project on improving inpatient endoscopy focuses on nursing/team communication, nursing/patient education, and modifying our current prep process. We are creating a new epic order set for colonoscopy preps that will include clearer guidance on steps to achieving adequate preps as well as concerning signs/symptoms that should warrant evaluation from the managing team.”
What is the timing for this project?
“The project is slated to start in July. We are currently gathering baseline data and working on the components of the order set.”
How will the value of care be improved?
“The hope is this project will allow for better communication between GI procedures, our fellows and the floor teams which will allow for increased and more efficient throughput in the procedure unit as well as fewer cancelled procedures. We also hope this leads to clearer post-procedure communication facilitating discharge. If we are able to improve efficiency for inpatient procedures, the downstream impact includes a decreased length of stay for our patients and a consequent cost reduction as well.”
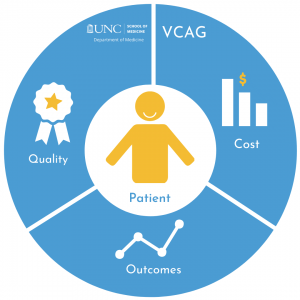
About Value-Care Action Group
VCAG encourages the review of current practices, looking for improvements for high-value outcomes in healthcare. High-value is defined by the quality of patient-centered care achieved per unit of cost, derived from measuring health outcomes against the cost of delivering the outcomes. Ron Falk, MD, chair of the department of medicine, created the Value-Care Action Group (VCAG) in 2016 and appointed value-care champions in each medicine division. VCAG projects have included the outpatient diuresis clinic, the inpatient diabetes management service and a patient education initiative that has improved care for cancer patients while reducing unnecessary visits to the ED. New VCAG awardees and projects for FY-2022 were recently announced. Scott Keller is the director of business development keeping the team focused on value-oriented care models. Darren DeWalt, MD, serves as medical director for the team and helps define the projects. John Vargas is the project manager.