The power of observation in advancing clinical medicine and research is undeniable. To quote DH Lawrence: “What the eye doesn’t see, and the mind doesn’t know, doesn’t exist.”
But how to resolve a conundrum where the mind is convinced that a phenomenon must exist, but the eyes cannot confirm or deny its existence?
We encountered one such conundrum in our research with focused ultrasound. We will call it ‘The curious case of disappearing ablation!’
It so happens that when we treat patients with focused ultrasound, we see a well-defined ablation on imaging immediately after the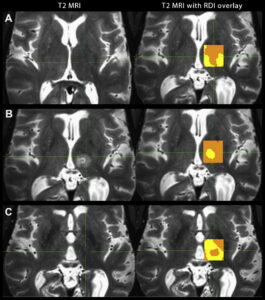 surgery. However, as time passes, the ablated tissue disappears and becomes indistinguishable from the surrounding brain. This disappearance adversely impacts patient care, especially when formulating a well-informed treatment plan.
surgery. However, as time passes, the ablated tissue disappears and becomes indistinguishable from the surrounding brain. This disappearance adversely impacts patient care, especially when formulating a well-informed treatment plan.
Francesco Sammartino, whom I had the privilege of working with, took this challenge head-on. Together, we consulted with Frank Yeh at the University of Pittsburgh, who suggested using an analytical tool developed in his lab. Frank named it “restricted diffusion imaging” (RDI). We implemented this novel approach and, to our utmost surprise, detected the ablated tissue even one year after the treatment.
The three panels, A, B, and C, compare conventional imaging (left image) and RDI (right image) at three time-points: before surgery, 24-hours after surgery, and one year after surgery. The open-access link to our full paper, “Longitudinal analysis of structural changes following unilateral focused ultrasound thalamotomy,” is available here: https://bit.ly/3qSwbDT
This transformative approach revealed interesting insights and had implications that we will share in our next post of the series.
If you are a resident, medical student, or imaging researcher interested in participating in this research, please email Dr. Vibhor Krishna at vibhor_krishna@med.unc.edu.