2017-18 MSPE Appendix C & D
Medical School Information
University of North Carolina, School of Medicine, Chapel Hill: Class of 2018
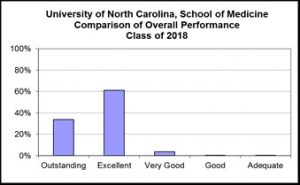
Assignment of the performance rating category is based primarily on grades and performance on USMLE exams, but may also reflect extraordinary leadership,
community service, or research productivity.
Medical School Information
University of North Carolina, School of Medicine, Chapel Hill: Class of 2018
I. Special programmatic emphases, strengths, mission and goals of the medical school:
The mission of the University of North Carolina, School of Medicine is to improve the health of North Carolinians and others whom we serve, accomplished by achieving excellence and providing leadership in patient care, education and research. The UNC Health Care System is a tertiary care referral center, receiving regional, national, and international referrals. According to U.S. News and World Report 2018 rankings, the UNC School of Medicine ranks second in commitment to training primary care physicians and twenty-fourth in excellence in research.
II. Special characteristics of the medical school’s educational program:
In 2014, the UNC School of Medicine implemented Translational Education at Carolina (TEC), a tripartite, translational medical school curriculum, comprising a Foundational Phase (Semesters 1-3); an Application Phase (semesters 4-5); and an Individualization Phase (semesters 6-8). TEC seeks to transform the way medical students learn the art and science of medicine by integrating basic sciences and clinical skills, providing longitudinal patient care experiences and offering earlier clinical opportunities in specialty fields to better inform students’ career choices. This curriculum reflects the ever-changing practice of medicine, allows early career differentiation and exploration, and incorporates the learning preferences of today’s medical students. The Class of 2018 is the first class to graduate from the new curriculum.
- Foundation Phase (semesters 1-3): the first phase comprises three semesters of organ-based blocks, clinical skills education, and professional development through courses in Patient Centered Care, Professional Development and Medical Sciences. Foundation Phase combines normal and abnormal human conditions, teaches through clinical cases and experiences, and employs active learning techniques, such as small group discussion and simulation. Coils represent basic sciences, such as biochemistry and microbiology, and specialty areas, such as radiology and behavioral science, which are integrated throughout the curriculum.
- Transition Course (one week): As part of the TEC curriculum, students complete a one week course to help facilitate the transition from the structured instruction of the classroom to the unstructured settings of clinical medicine. This course is completed during the week preceding the start of the Application Phase.
- Application Phase (semesters 4-5, plus one month): During Application Phase, students spend 12 months completing core clinical clerkship blocks in psychiatry, neurology, surgery, pediatrics, obstetrics and gynecology, internal medicine, and family medicine. Students can complete the Application Phase in one of four campus programs: Charlotte, Asheville, Wilmington and Central (Chapel Hill and surrounding areas). All campuses have the same course objectives and assessments, but each site is characterized by a unique curricular structure incorporating varying amounts of integration, self-directed learning and longitudinal emphasis. Regardless of campus assignment, all students will be prepared for Individualization Phase and their future career endeavors.
- Intensive Integration (meets monthly during Application Phase): in addition to the three phases of TEC as described above, students complete the Intensive Integration Course during this phase, in which they develop skills to apply clinically-relevant basic sciences, humanities, social and behavioral science, and population health to the care of patients, and demonstrate effective strategies for caring for patients with contextual challenges (poverty, under-insurance, low literacy, low English proficiency, limited social support, etc.) Students refine advanced communication skills such as delivering bad news, motivational interviewing, end-of-life care planning, and handing off care of patients. They continue to develop and improve skills to work effectively in teams across disciplines and professions. The course highlights translation of basic science principles to clinical medicine, examines strategies for improving systems of care, and gives students an opportunity to critically reflect with a faculty mentor on patient care encounters experienced throughout the Application Phase, exploring moral quandaries encountered in clinical decision making, stigma and the effects of social determinants of health on individual patients.
- Individualization Phase (semesters 6-8): This is the third and final phase of medical school education. During these 14 months, students develop individual core clinical interests and skills with focus on future career plans, and have many options to individualize their learning experience based on their career goal interests and their unique needs for clinical skills development.
Campus Branches
In the class of 2018:
23 students were selected to complete Application Phase at Carolinas Medical Center (CMC) in Charlotte, NC, one of the largest not-for-profit healthcare systems in the nation. Students in the Charlotte Program complete a curriculum that consists of six months of integrated longitudinal experiences and six months of inpatient experiences.
20 students were selected to complete Application Phase in Asheville, NC, in an alternative curriculum of Longitudinal Integrated Clerkships Mission Hospital and the Mountain Area Health Education Center (MAHEC).
3 students were selected to complete Application Phase in Wilmington, NC, in our inaugural cohort of students completing third year at New Hanover Regional Medical Center and Southeast Area Health Education Center (SEAHEC). Wilmington students follow the same curriculum as Central Campus students.
3 students were selected for the inaugural cohort of F.I.R.S.T. (Fully Integrated Readiness for Service Training), a three-year medical school curriculum to fast-track into UNC Family Medicine Residency, followed by three years of service in North Carolina with ongoing support in practice. Curriculum starts March of Foundation Phase.
Additional Degrees
Approximately 35%% of students in this class took a leave of absence, usually following third year, to conduct research, complete an M.P.H., M.S.P.H. (usually at the UNC Gillings School of Global Public Health), an M.B.A. (usually at the UNC Kenan-Flagler Business School) or other graduate degree. M.D./Ph.D. students usually go on a leave of absence after second year.
Average length of enrollment (initial matriculation to graduation, in calendar years) at UNC/SOM:
All graduates: 4,23 years
M.D. only: 3.87 years
M.D./M.P.H.: 4.78 years
M.D./M.B.A.: 4.77 years
M.D./Other 4.77 years
M.D./Ph.D.: 8.40years
Description of the evaluation system used at the medical school:
Grades Used in the Foundation Phase Are: Grades Used in the Second Year Are:
P: Pass, Entirely Satisfactory H: Honors, Clear Excellence
F: Fail, Failed P: Pass, Entirely Satisfactory
W: Withdrew from Course BE: Credit by Examination
W: Withdrew from Course
Grades Used in Application and Individualization Phase:
H: Honors, Clear Excellence
HP: High Pass, Above Average
P: Pass, Entirely Satisfactory
F: Fail, Failed
Temporary Grades:
AB: Absent from Examination
IN: Incomplete other than final examination
GRADING
All campuses adhere to the same assessment structure and grading standards.
- Foundation Phase: all Medical Science, Patient Centered Care and Professional Development courses are graded on a Pass/Fail basis. Students receive a Pass (P) on their official transcripts for each course within a semester in which they demonstrate satisfactory performance. Students who successfully pass all blocks within a course receive a Pass (P) for the semester-long course on their official transcripts.
- Application Phase: all courses, with the exception of Intensive Integration, use the following grading standards that rely on a 100 point scale. Passing is defined as scoring greater than 2.5 SD below the mean on final score calculation. Students who fail are required to retake the full course. Of students who meet this criteria, Honors/High Pass/Pass is awarded using the following guidelines.
Honors: top 30-35%
High Pass: middle 40-50%
Pass: lower 20-25%
- Individualization Phase: all Individualization Phase courses are graded on a scale of Fail, Pass, High Pass, and Honors. Research electives are an exception, and are graded on a Pass or Fail basis.
Medical school requirements for successful completion of USMLE Step 1and 2: (check all that apply):
| USMLE Step 1:
√ Required for promotion □ Required for graduation □ Required, but not for promotion/graduation □ Not required |
USMLE Step 2 Clinical Knowledge:
□ Required for promotion Required for graduation √ Required, but not for promotion/graduation □ Not required √ Required for NRMP |
USMLE Step 2 Clinical Skills:
□ Required for promotion □Required for graduation √ Required, but not for promotion/graduation □ Not required √ Required for NRMP |
Medical school requirements for successful completion of Objective/Observed Structured Clinical Evaluation (OSCE) at medical school. OSCEs are used for (check all that apply):
√ Completion of course
√ Completion of clerkship
□ Completion of third year
√ Graduation
Utilization of the course, clerkship, or elective director’s narrative comments in composition of the MSPE. The narrative comments contained in the student’s MSPE can best be described as (check one):
√ Reported exactly as written
□ Edited for length or grammar, but not for content
□ Edited for content or included selectively
Utilization by the medical school of the AAMC “Guidelines for Medical Schools Regarding Academic Transcripts.” This medical school is (check one):
√ Completely in compliance with Guidelines’ recommendations
□ Partially in compliance with Guidelines’ recommendations
□ Not in compliance with Guidelines’ recommendations
Description of the process by which the MSPE is composed at the medical school (including number of school personnel involved in composition of the MSPE):
Each MSPE is drafted by a staff writer, reviewed by the student, and the Dean or a member of the Student Affairs staff. Students read the final version (and may have it reviewed by their academic advisor) before submission.
Students are permitted to review the MSPE prior to its transmission (check one): √ Yes □ No