MD Curriculum
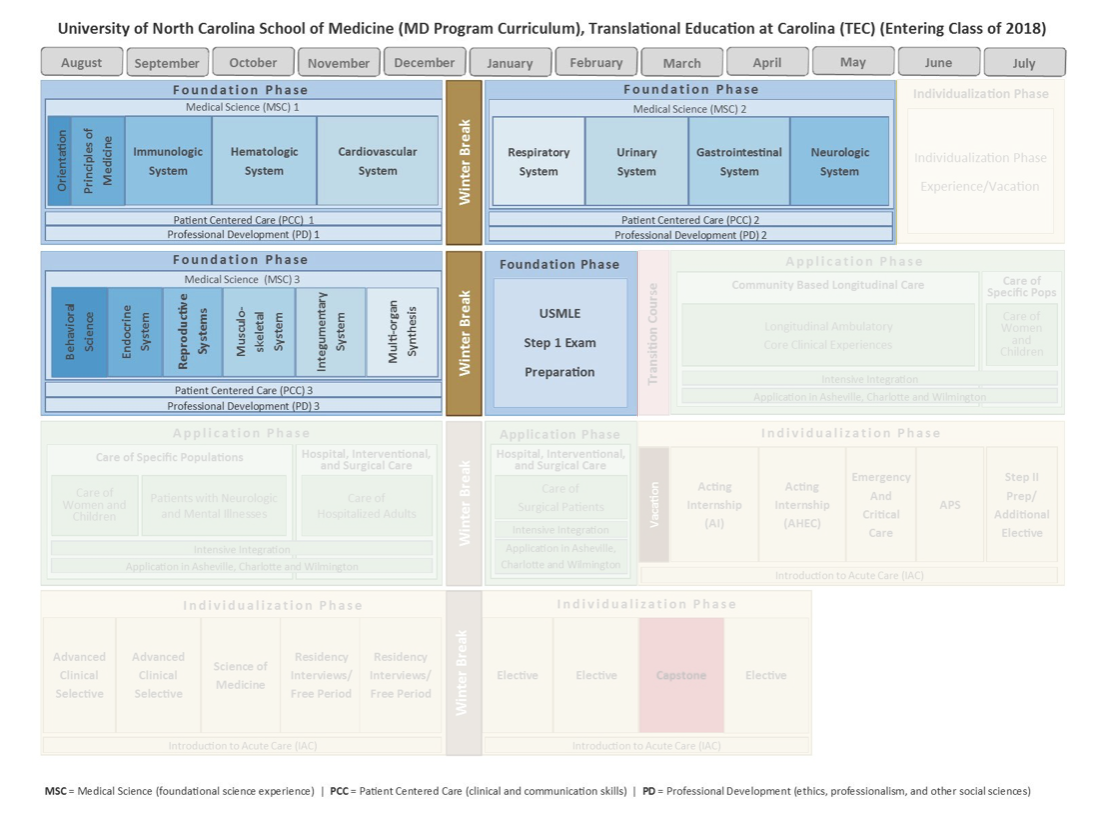
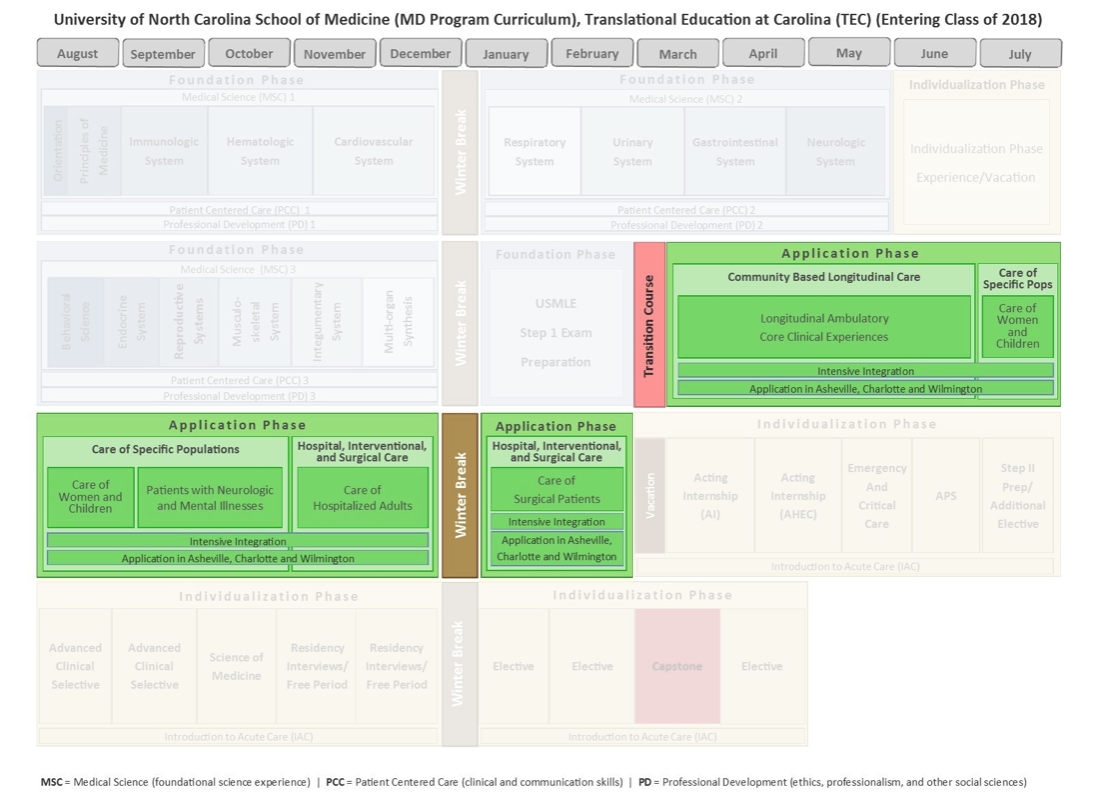
The School of Medicine’s Translational Education at Carolina (TEC) curriculum has been designed to transform the way medical students learn the art and science of medicine through integrated basic science and clinical skills blocks, longitudinal patient care experiences, and flexible clinical experiences that give them opportunities in specialty fields well before they apply to residency programs. This redesigned curriculum reflects the needs of future physicians, the desire for early differentiation and exploration, and the realities of adult learners today.
The TEC curriculum consists of three phases:
Foundation Phase
August through June of Year One
August through December of Year Two
This 16-month foundational education replaces the traditional curriculum often seen in the first two years of medical school. The foundation blocks integrate normal and abnormal human conditions, teach the basics through cases and clinical experiences, and rely extensively on active learning techniques.
Application Phase
March of Year Two through February of Year Three
The redesigned clinical experience at UNC begins six months earlier than it does in traditional four-year medical schools. These experiences are designed around the needs of patients in specific settings rather than being organized according to departments and specialties. For instance, the Reproductive and Early Life Care block reorganizes the traditional Obstetrics/Gynecology and Pediatrics clerkships into an experience that reflects the continuum of care from prenatal care through adolescent medicine.
MD/PhD students are uniquely positioned to complete the first 16-week block of the Application Phase prior to beginning their PhD training.
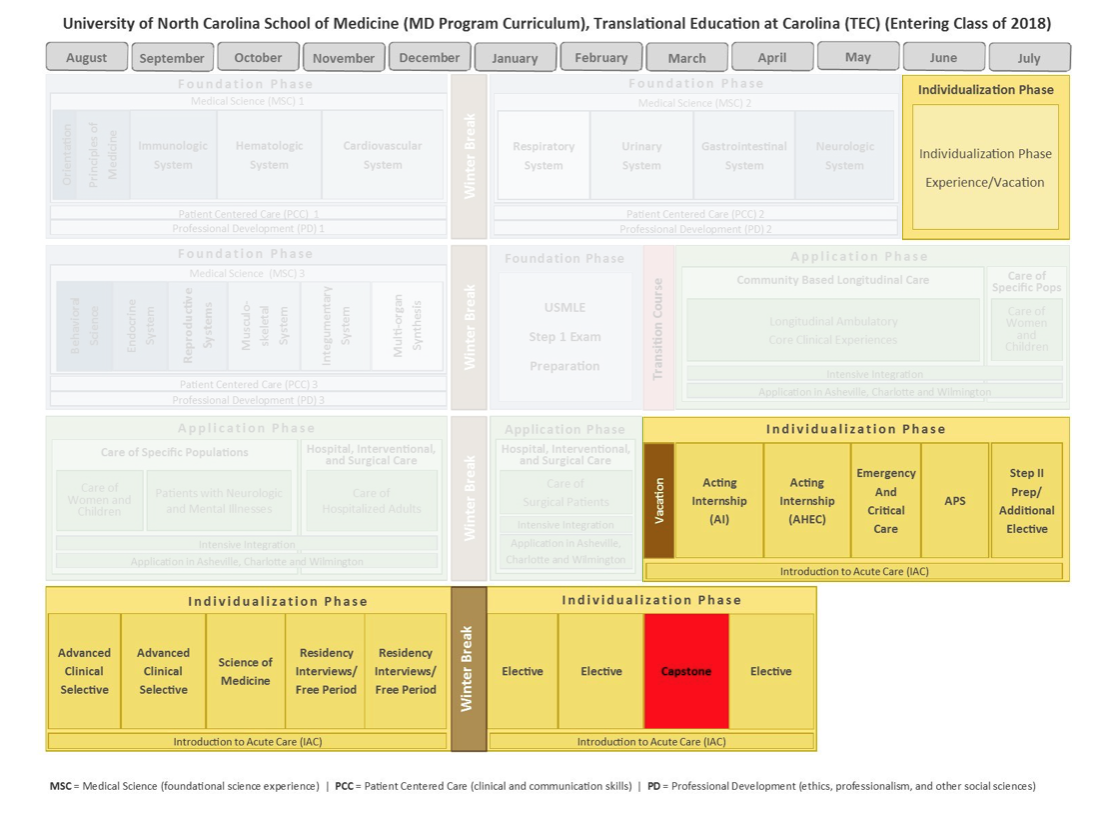
Individualization Phase
Summer between Years One and Two
March of Year Three through May of Year Four
An earlier start into what is traditionally the fourth year of medical school allows students to have more time to take clinical electives, which in turn helps them choose their future specialties. Students work with their career goal advisors to develop an individualized learning plan and personalize their learning experience. The Individualization Phase includes optional tracks that focus on medical education, global health, rural and community medicine, and other student personal interests.
 |
||
|---|---|---|
 |
||
 |
Click here for more information and a complete view of the current TEC calendar.
Guiding Principles of the UNC School of Medicine Curriculum
- Be student-centered and patient-based, while being population, public health, and globally inspired
- Facilitate the translation and integration of basic, clinical, and population science to enhance human health and well being
- Provide a strong foundation for entry into graduate medical education within the broad opportunities of medicine, while being flexible and individualized
- Be responsive to the changing healthcare environment
- Focus on promoting, supporting, and maintaining health, not just treating disease
- Incorporate strengths of the university, including opportunities for inter-professional and cross-disciplinary education
- Provide longitudinal engagement with faculty and robust mentorship
- Incorporate multiple modes of student learning
- Instill intellectual curiosity and develop an aptitude for critical thinking and lifelong learning
- Promote the development of leadership skills, professionalism, ethics, humanism, and service to others
For more information about the MD-PhD Program curriculum, requirements, and supplemental learning opportunities, check out the following pages:
- About the MD Curriculum
- Program Requirements
- Bridging the Gap
- Events and Opportunities
- Student-Led Initiatives
UNC Department of Medicine’s Physician Scientist Training Program
After completion of Medical School, the Department of Medicine at the University of North Carolina is committed to the development of physician-scientists and offers a program to recruit and train young physicians interested in pursuing academic careers in medical research.
This program allows candidates with significant research experience (PhD, MPH, or equivalent research background) to complete Internal Medicine residency, fellowship, and postdoctoral research training via the ABIM Research Pathway.