Our Research
Our research focuses on Antibiotic Resistance Mechanisms in Neisseria gonorrheae and P2Y receptors
- Antibiotic Resistance in Neisseria gonorrhoeae
- Mechanisms of chromosomally mediated antibiotic resistance
- Biological fitness consequences of acquiring resistance to cephalosporins and compensatory mutations that increase fitness of resistant strains
- Development of novel antimicrobials for treatment of N. gonorrhoeae infections
- P2Y Receptors
- Regulation of P2Y Receptor signaling in platelets
- Signaling mechanisms of P2Y receptors
Antibiotic Resistance Mechanisms
My laboratory is focused on elucidating the mechanisms of antibiotic resistance in the pathogenic bacterium, Neisseria gonorrhoeae, the etiologic agent of the sexually transmitted infection, gonorrhea. In the last decade, the gonorrhea infection rate in the US has more than doubled. Complications arising from untreated infections include pelvic inflammatory disease (PID) and ectopic pregnancies in females, and gonococcal arthritis and an increased risk of both contracting and transmitting HIV in both sexes.
Over the past several decades, the steady and inexorable increase of resistance in this organism toward multiple classes of antibiotics, including penicillin, tetracyclines, macrolides, and fluoroquinolones, has severely restricted treatment options for gonorrhea infections. Recently, strains resistant to ceftriaxone, the last remaining effective antibiotic, have emerged, portending an era of untreatable gonorrhea.
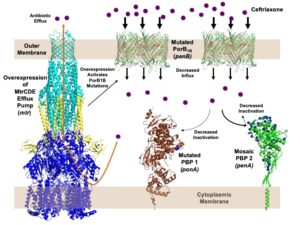
Nearly all strains resistant to ceftriaxone contain a highly mosaic penA gene encoding penicillin-binding protein 2 (PBP2), the lethal target of ceftriaxone, with over 60 amino acid mutations. It is the primary determinant of resistance to cephalosporins. Other mutations include mtr, which increases expression of the MtrCDE efflux pump, and penB, which encodes mutations in the major outer membrane porin, PIB (fig. 1).
We are investigating the structural mechanisms of resistance of PBP2, how the presence of a highly altered PBP2 impacts biological fitness and pathogenesis, and identifying compensatory mutations arising in the mouse model of gonococcal infection that increase fitness of mosaic penA-containing strains.
Platelet P2Y Receptor Regulation
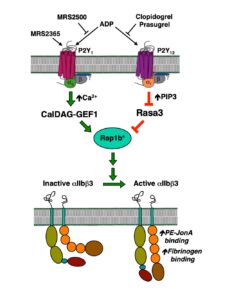
P2Y receptors are important receptors in platelet biology. When platelets encounter underlying tissue following disruption of the blood vessel, they form a small platelet clot due to the action of thrombin on PAR receptors on platelets. These platelets also release dense granules containing secondary mediators, resulting in additional aggregation of passing platelets and formation of a platelet plug. One of the most important of these mediators is ADP, which acts on two P2Y receptors: P2Y1 and P2Y12. The P2Y1 receptor couples to Gq, mobilizes intracellular Ca2+, and activates PKC, whereas the P2Y12 receptor couples to Gi and inhibition of adenylyl cyclase (the P2Y12 receptor is the target of the anti-platelet drug Plavix). Simultaneous activation of these two receptors is required for aggregation (Fig. 2). The P2Y1 receptor is uniquely regulated and rapidly desensitizes (t1/2 of ~18 sec), preventing further aggregation. We are investigating the molecular mechanisms of this rapid desensitization in knock-in mice expressing a non-desensitizing receptor mutant receptor.
Figure 2. Diagram of the simultaneous activation of P2Y1 and P2Y12 receptors leading to platelet aggregation.