Venous Thrombosis
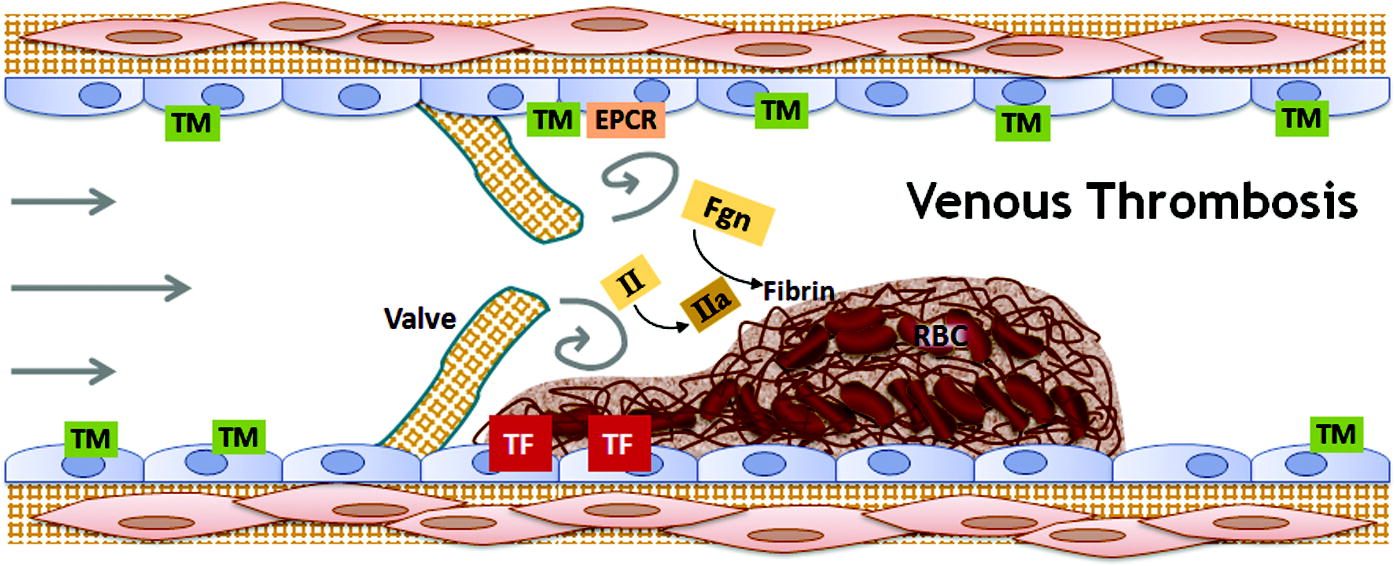
Venous thromboembolism kills about 300,000 Americans each year and is the leading cause of loss of disability-adjusted life years in hospital patients around the world, making the disease a major public health concern. Venous thrombosis can also lead to dangerous complications, such as pulmonary embolism and post-thrombotic syndrome. Venous thrombosis occurs when red blood cell-rich thrombi form in veins; this is often due to abnormal interactions between three components: blood hypercoagulability, abnormal blood flow, and endothelial dysfunction. We have helped to elucidate specific pathobiological mechanisms contributing to venous thrombosis, including specific roles for fibrinogen, prothrombin, factor VIII, and factor XIII. We are interested in further discerning mechanisms and potential therapeutic targets to determine new and more effective treatments.
Figure: Interplay between abnormalities in blood components, the vasculature, and blood flow contribute to the development of venous thrombosis. Abbreviations: TM, thrombomodulin; EPCR, endothelial protein C receptor; II, prothrombin; IIa, thrombin; TF, tissue factor; Fgn, fibrinogen; RBC, red blood cells