As a pediatric resident, Zachary Willis, MD, MPH developed an early interest in antimicrobial stewardship. In his role as director for pediatric antimicrobial stewardship with UNC Medical Center’s Carolina Antimicrobial Stewardship Program (CASP), he was compelled to find ways to optimize antimicrobial use at UNC Children’s Hospital and across the Medical Center.
To that end, CASP tested an intervention called antibiotic time-outs in a 2017 pilot. It involved antimicrobial stewardship pharmacists identifying patients daily and asking a small group of pharmacists to review their antimicrobial therapy.
Antibiotic time-outs are formal reassessments of antimicrobials prescribed to inpatients. A time-out provides a structured opportunity to review a patient’s antimicrobial therapy 36 to 72 hours into the regime. The healthcare provider takes new information into account–such as results from blood or urine cultures and how the patient is responding to the drug — and decides if adjustments are needed to the drug, dose, duration, or route. For example, drugs can be selected to more precisely target the organism identified in a culture, discontinued if the patient is not found to have an illness that will respond to antimicrobials after all, or changed from the IV to oral route and vice versa. In approximately two-thirds of patients at UNC Hospitals, a time-out confirms that no change is needed.
It turns out, CASP was ahead of the curve. “By early 2018, the Centers for Disease Control and Prevention and the Centers for Medicaid and Medicare Services were placing increased emphasis on antibiotic time-outs,” Willis said, referring to two federal divisions with a stake in ensuring hospital participation in antimicrobial stewardship. “However, colleagues at other institutions all seemed to agree that they were difficult to implement.” In its pilot, CASP found that adherence to time-outs was good, and the participating teams found time-outs beneficial to patient care. However, the team recognized that more support would be needed to continue and expand the antibiotic time-out process.
In August 2018, Willis received support from the UNC Institute for Healthcare Quality Improvement (IHQI) to implement routine, documented, meaningful antibiotic time-outs for medical patients at UNC Hospitals Hillsborough Campus. Hillsborough’s geriatrics and general medicine services participated in the pilot. The project also provided an opportunity to contribute to the small but growing evidence base on time-outs. In early 2019, Michael Swartwood joined as project manager, expanding its ability to manage data and provide timely feedback to teams on their progress. Willis, Swartwood, and their collaborators plan hope to demonstrate how time-outs can be a useful tool to optimize antimicrobial treatment and reduce unnecessary, redundant, or longer-than-needed antimicrobial use, as a part of a holistic antimicrobial stewardship program.
In the past year, all participating services have exceeded the 80% performance benchmark for eligible patients receiving an antibiotic time-out within the time window, according to Swartwood. “We’ve been impressed with the results we’ve seen at the Medical Center so far,” Willis shared. More results are expected to be published later this year.
The long-term goal of the IHQI award was to take the approach refined at Hillsborough Hospital and expand across UNC Hospitals and then potentially to the entire UNC Health system. Two hospitalist services joined the two pilot services, all at Hillsborough. Later, the project added more services from the main UNC Hospitals campus: first family medicine services, followed by two pediatric general medicine services. The most recent addition to the project was the pediatric ICU, bringing the total number of participating teams to nine.
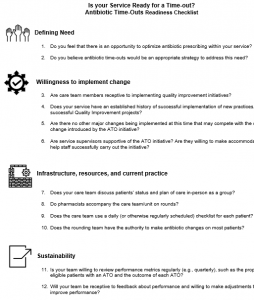
Willis hopes that in time, the initiative will be hospital-wide. CASP recently created a checklist to help a patient care team determine whether conditions are favorable to begin implementation of antibiotic time-outs.
“Committing to antibiotic time-outs is a culture change. As with any habit, it takes time for it to become second-nature. Across our participating services, we’ve seen nurse coordinators, physicians, and pharmacists take the lead to ensure that time-outs happen consistently,” Willis explained. “Service leaders can help by encouraging their teams to participate and adapting the time-out process to their teams’ needs.”
So far, antibiotic time-outs have worked well consistently without prompts in the electronic medical record system. However, as more patient care teams initiate time-outs, integrating an automated best practice alert in a patient’s medical record will ensure that all eligible patients receive a time-out during the window when time-outs can be most helpful. “We are working closely with Information Services to develop a prompt for the care team of any patient who has recently started an antimicrobial to complete a time-out. It’s just one more tool we have in our arsenal to make sure we’re doing the best we can by our patients to prevent harms caused by unnecessary antimicrobial use,” Willis said.