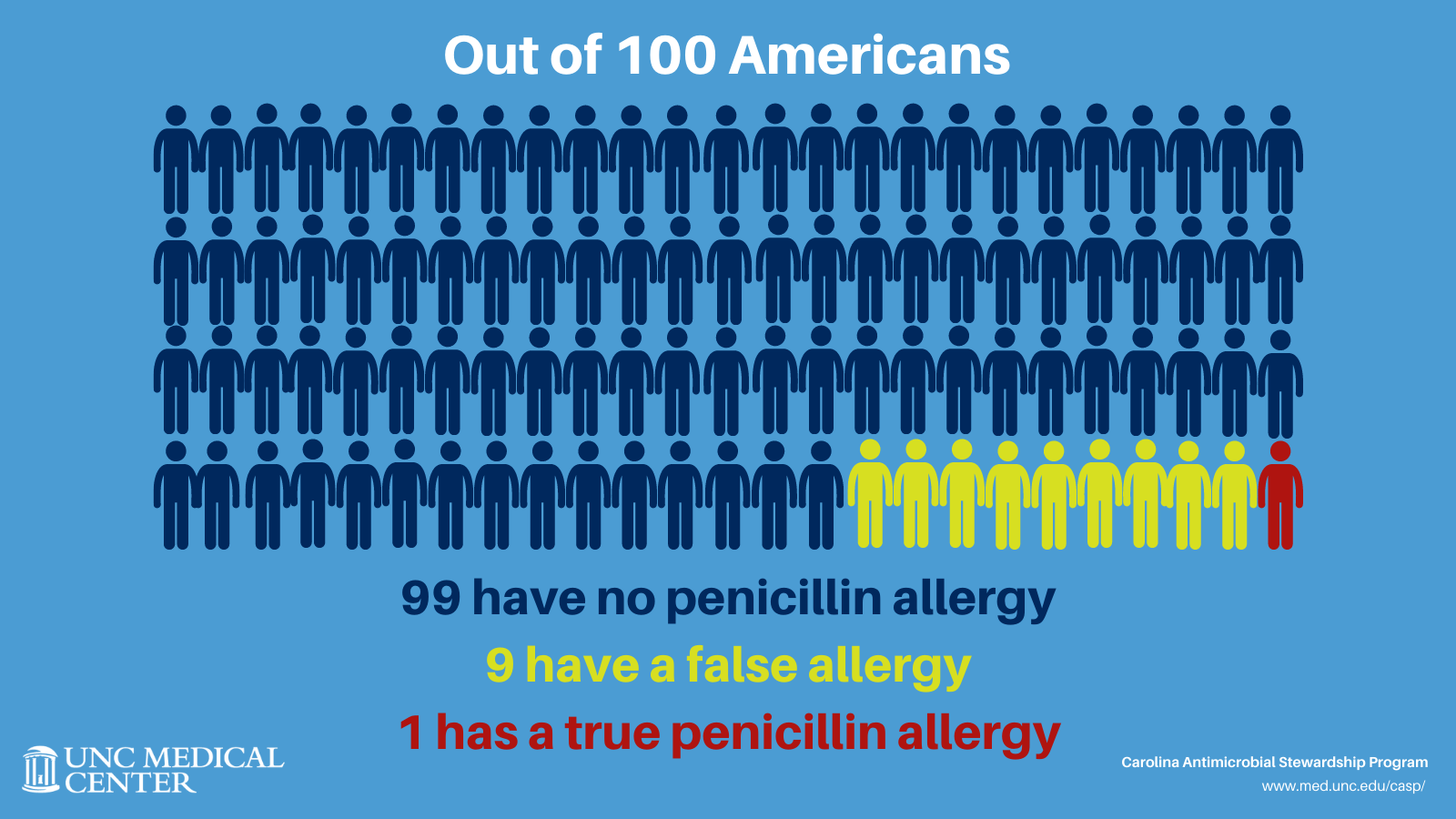
One in ten Americans believes they are allergic to penicillin. However, when assessed, the vast majority of these may not be allergic at all and can safely use penicillin antibiotics—which includes penicillin, amoxicillin, Augmentin, ampicillin, and Zosyn, among others–to treat some infections.
There are two main reasons for this. First, some childhood rashes – not related to penicillins–can be misinterpreted as a reaction to penicillins. In other cases, some people are allergic to penicillins, and they lose their sensitivity to it about ten years after the initial reaction. After this time, an individual can safely take penicillins if needed. Unfortunately, once an allergy of any kind is documented in a patient’s medical record, it is rarely questioned.
A growing number of medical professionals believe penicillin allergies should be reevaluated. Experts agree that penicillin antibiotics are the best option to treat many common infectious because they have less risk of side effects or complications that may be associated with other antibiotics. Using penicillins instead of other broader-spectrum antibiotics is also better for population health, as it can help slow antibiotic resistance. A bonus is this antibiotic class is often lower cost than the alternative beta-lactam antibiotics.
Under the leadership of Renae Boerneke and Michael Swartwood, the Carolina Antimicrobial Stewardship Program (CASP) set out to develop and test an intervention to help patients learn if they are, in fact, allergic and then ensure their medical records are updated to reflect any changes. Gary Burke, Lindsay Daniels, Mildred Kwan, Nikolaos Mavrogiorgos, Ashlyn Norris, and Kalynn Northam were collaborators on developing the pilot.
The first step in the project was to determine how common penicillin allergies are in the UNC Emergency Department (ED) to inform the development of the intervention. Since EDs are the point of entry into healthcare for many patients across the US, with more than 130 million visits each year, it is a natural setting to test this type of intervention. Infectious Diseases Pharmacy Resident Ashlyn Norris examined data from adults who were discharged from the UNC Medical Center’s Emergency Department any time between 2017 and 2020. She found that 14% (8,573) of these had a penicillin allergy documented in their medical record.
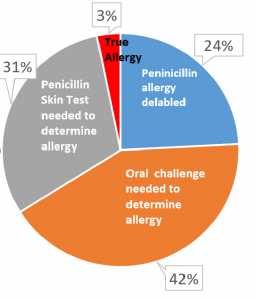
Norris’s next step was to determine the percentage of penicillin allergy-positive patients that could be delabeled, which removes an allergy from a patient’s medical record, using a penicillin allergy assessment within the ED. She carried out penicillin allergy assessments on a sample of 95 ED patients in December 2020. Of the 95 patients assessed, Norris interviewed 62 (65%) to learn more about their previous reactions. Based on their responses, 15 (24%) had their past penicillin allergy delabeled. Of the 15 patients that were delabeled, 6 (40%) received antibiotics during their admission, 4 (73%) of those patients received a penicillin, and 2 (37%) received an antibiotic in the same drug class (cephalosporin) without adverse reactions. Two (3%) patients did not qualify for further assessment due to an allergic reaction to penicillin in the past five years. Patient assessments took approximately 20 minutes to complete, including chart review, patient interview, and documentation in the medical record.

“Appropriately updating patient allergy profiles could decrease the use of alternative broad-spectrum antibiotics, rates of complications, antibiotic resistance, and overall healthcare costs,” Norris said.
The majority of patients required further evaluation, either a skin test or an oral challenge, to determine their allergy status. Some 26 (42%) patients met the criteria for an oral amoxicillin challenge, which involves giving a small dose of amoxicillin to a patient at low risk for a true allergy. The patient is monitored for a reaction and receives treatment if a reaction occurs. If they tolerate it with no problems, the allergy can be removed. If they have a reaction, the person receives treatment, and their allergy is updated to reflect a true allergy. Another 19 patients (31%) qualified for a penicillin skin test, where a small amount of penicillin is placed under the skin to test for a reaction. PST and amoxicillin challenges were not carried out as a part of this pilot, though the results suggest there is potential for an even greater number of patients to be delabeled.
“The results from this pilot study are promising. We are exploring ways to make penicillin allergy assessments routine in the ED. We also hope to improve the efficiency and sustainability of allergy assessments to allow this important stewardship intervention to continue,” Norris said. “Appropriately updating patient allergy profiles could decrease the use of alternative broad-spectrum antibiotics, rates of complications, antibiotic resistance, and overall healthcare costs.”