In January, the UNC Medical Center’s Anti-infectives Sub-committee approved a new Clostridioides difficile, or C. difficile, infection guideline to provide evidence-based best practices for diagnosis and management of the disease. The US Centers for Disease Control and Prevention estimates that CDI sickens an estimated 462,000 people in the US, leading to some 15,000 deaths each year. Lindsay Daniels chairs the sub-committee and is also the pharmacy lead for the Carolina Antimicrobial Stewardship Program (CASP) at UNCMC.

As a part of CASP’s years-long collaboration with the Healthcare-associated Infections Prevention Initiative (formerly the C. difficile Workgroup), a small group of experts led by UNC Children’s pediatric infectious diseases pharmacist and CASP member Bill Wilson developed the guideline. “The group benefited from the complementary lenses each person brought from their respective disciplines, from infection prevention to pharmacy to microbiology,” Wilson shared. “Because of the collaboration, we were able to deepen our understanding of each person’s role in the management of CDI. It allowed us to determine what areas of CDI management we each felt were most important to include in the guideline to best assist clinicians in appropriately diagnosing and treating CDI”. The guideline is tailored to the Medical Center’s existing microbiology lab procedures and pharmacy formulary. Kevin Alby, Tom Belhorn, Nikolaos Mavrogiorgos, Shelley Summerlin-Long, Kate Schultz, and Amy Selimos contributed to the guideline’s development.
The Medical Center drove down CDI rates a remarkable 42% following the implementation of a set of evidence-based practices, or a “bundle,” in 2016. Since that time, the HAI Prevention Initiative has continued to develop ways to lower infections further. The guideline is the latest contribution to those efforts.
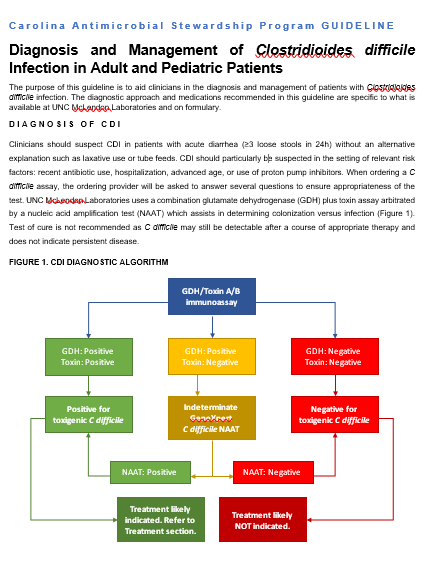
Recent data from Infection Prevention shows that clinicians sometimes order tests for C. difficile even when the patient’s stool does not meet testing criteria. This can result in a positive test for C. difficile because the bacteria may be present in a healthy gut and only becomes pathogenic when conditions (such as recent antibiotic use) cause the bacteria to flourish. In cases where a test is ordered inappropriately and C. difficile is detected, treatment may be started unnecessarily, leading to additional antibiotic exposure that is otherwise not needed. To help prevent this, UNCMC’s McLendon Lab, which tests microbiology samples, uses tests that can help a healthcare provider discern the difference between colonization and infection. The group of experts developing the guideline identified this as a common area of confusion for clinicians. For that reason, the guideline includes a section reviewing when it is appropriate to send a test for C. difficile and how the microbiology lab processes each sample to reduce overtreatment.
The guideline helps providers determine what actions to take based on microbiology lab results, the severity of symptoms, and whether or not the patient has had CDI in the past. For example, it recommends:
- In patients with CDI, all antibiotics not targeting C. difficile should be reviewed and stopped as soon as feasible.
- Enteral vancomycin is the preferred antibiotic for most patients with CDI.
- Patients with CDI should be placed on enteric precautions until 30 days after completing CDI treatment. C. difficile forms spores which are easily spread and not eliminated by alcohol-based cleaners. Wearing appropriate personal protective equipment and washing hands with soap and water are critical for preventing the spread of C. difficile to additional people.
“It is our intention that this guideline will help clinicians in the management of CDI,” Wilson said, “and also to serve as an educational tool for the various health care professional students that frequent the wards and intensive care units of UNC Medical Center.”