 In the United States, respiratory infections are prevalent throughout the year and contribute significantly to the burden of disease on the healthcare system. These illnesses typically increase in frequency during the fall and winter months with peak activity from December to March. This increase can be attributed to colder temperatures forcing people to stay indoors in closer proximity, which facilitates respiratory transmission.
In the United States, respiratory infections are prevalent throughout the year and contribute significantly to the burden of disease on the healthcare system. These illnesses typically increase in frequency during the fall and winter months with peak activity from December to March. This increase can be attributed to colder temperatures forcing people to stay indoors in closer proximity, which facilitates respiratory transmission.
It is common for patients to seek medical therapy, including prescriptions for an antibiotic, after the onset of symptoms following infection. However, most respiratory infections including colds, flu, Respiratory Syncytial Virus (RSV), and Covid-19, are caused by viruses, which antibiotics do not treat.
Antibiotic-related adverse events are the second leading national cause of Emergency Department visits
Inappropriate antibiotic use causes significant health issues for patients and the community. Antibiotic-related adverse events are the second leading national cause of Emergency Department visits, and patients taking antibiotics are more likely to develop Clostridioides difficile infection or C. diff. The dangers of antibiotic over-prescribing also extend to the community in the form of multidrug-resistant organisms (MDROs), which cause an estimated 2.8 million hospitalizations and 35,000 deaths in the United States annually. These facts highlight the importance of judicious antibiotic use during winter.
Acute Respiratory Infections (ARIs) are an unfortunate hallmark of the holiday season. The most common ARIs are caused by viruses and include the common cold, influenza, Covid, and RSV. These infections pose a dilemma for clinicians in the outpatient setting because patients seeking a curative solution may be unaware that antibiotics are ineffective against viral illnesses. Given the fact that approximately 50% of all antibiotics used in the outpatient setting are prescribed inappropriately, effective antimicrobial stewardship, particularly surrounding seasonal illnesses, is critical.
Some 50% of all antibiotics prescribed in the outpatient setting are inappropriate, making effective antimicrobial stewardship, particularly surrounding seasonal illnesses critical.
Clinicians are encouraged take this opportunity to educate patients about the limitations of antibiotics and instead focus on providing targeted symptomatic relief. Uncomplicated viral ARIs are self-limiting, and symptom resolution typically occurs within one to two weeks without antibiotics. Table 1 summarizes common over-the-counter treatment options for symptomatic relief in patients with ARIs.

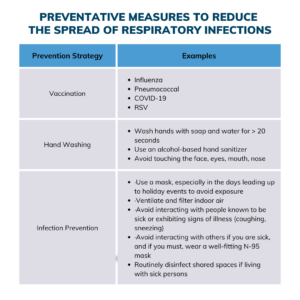
The best method to avoid these infections altogether is prevention. Clinicians are encouraged to educate patients on current immunization recommendations, which are updated regularly. Routine patient-centered care discussions ensure patients are protected from illness. Table 2 highlights effective methods, including available vaccines, for patients to avoid contracting viral ARIs.
Providers actively practice effective antimicrobial stewardship for patients and the community during the flu season by focusing on symptomatic treatment and preventative measures instead of prescribing unnecessary antibiotics. These practices reduce the risk of patient visits to the ED and instead allow patients to spend more time with friends and family this holiday season.
This article was written by Travis Jones, PharmD, CASP Pharmacist, UNC Hospitals, and James Stroud, PharmD Candidate 2024, UNC Eshelman School of Pharmacy.