A rounding intervention promises to improve resident-patient connections, fostering meaningful face time.

A new curriculum for physicians, nurses, care managers, pharmacists, and medical students is now available to implement a multidisciplinary bedside rounding strategy on their teams and units. Educational materials can be accessed here.
The Accreditation Council for Graduate Medical Education (ACGME) has selected UNC Medical Center as a funding recipient for Back to Bedside, a resident-led initiative to empower medical residents and fellows to find new ways to increase time with patients, to in turn, improve physician and patient well-being.
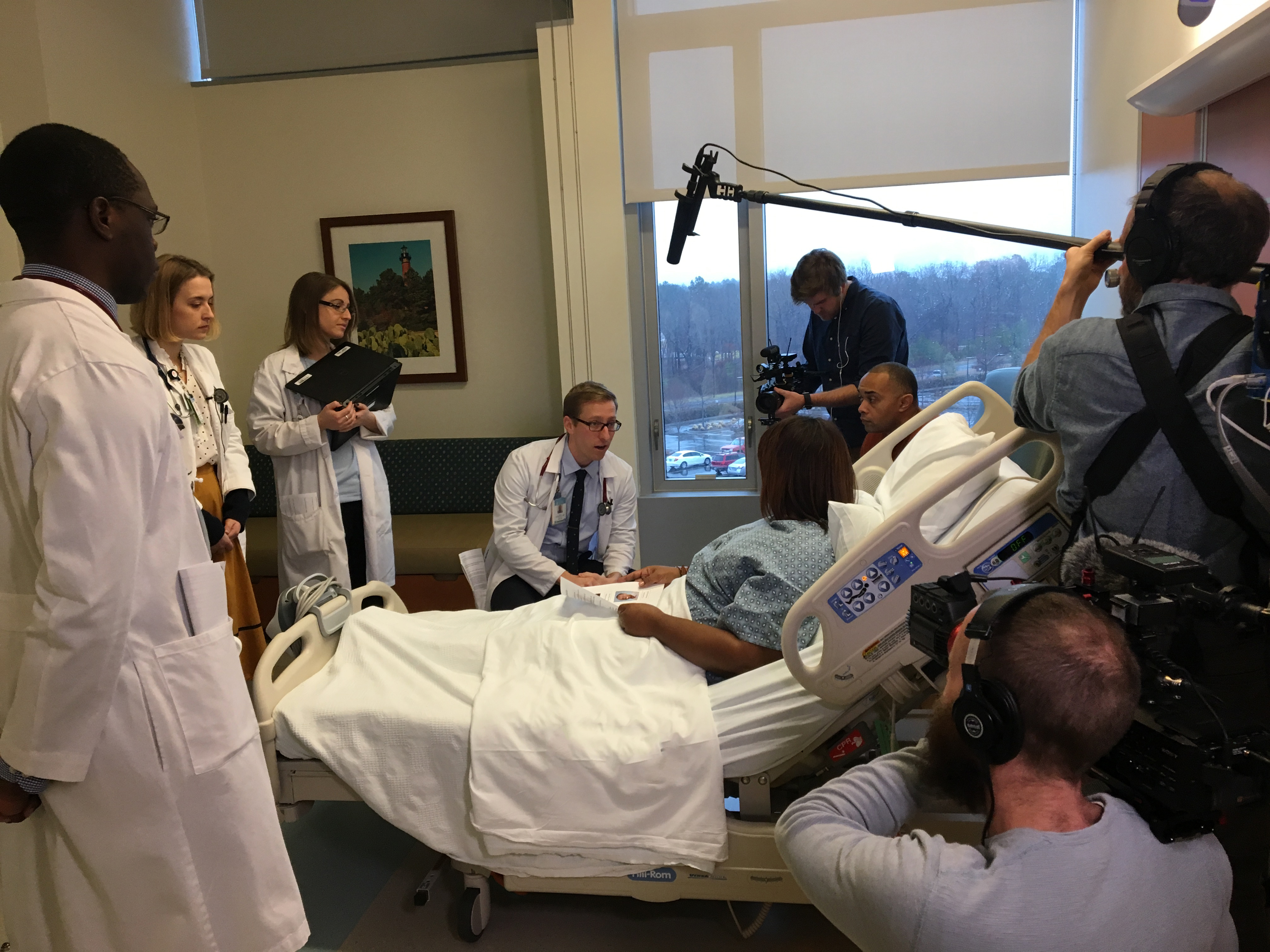
The UNC Department of Medicine team received the grant for creating a rounding intervention that reduces the amount of overhead with traditional rounding styles. Led by residents Kathryn Haroldson, MD, and Heath Patel, MD, the project focuses on increasing meaningful face time with patients on rounds. The team included Anthony Mazzella, MD, Rosanne Tiller, MD, Lila Stanton, MHA, and Debra Bynum, MD. Loretta Muss, coordinator of the UNC Patient and Family Advisory Council, also played a key role.
“An important component of our project was having access to patients who have been through our system,” said Dr. Mazzella. “We began working with Loretta and council members who have been our patients before and are now able to advise physicians. This has become a valuable pathway for change that can directly impact the physician-patient relationship.”
The previous rounding system offered limited patient engagement, as many important clinical discussions occurred away from the bedside. In addition, nurses had not been routinely involved during academic rounds, leading to ineffective multidisciplinary communication. This is known to increase dissatisfaction with patients, their caregivers, and providers. The team hypothesized that by rounding and discussing each problem in the patient’s room rather than outside a closed door, a patient’s involvement in their own care would increase, while at the same time shorten the duration of rounds overall.
Residents, attendings, nurses and patients were surveyed prior to the pilot and will be surveyed again after implementation. A timekeeper documents overall rounding time as well as time spent per patient interaction. Preliminary data shows overall shorter rounding time, but with increased time spent with each patient, dropping from 11 minutes 45 seconds to 9 minutes and 22 seconds. Meanwhile, bedside time increased from 40 to 70%.
“We’re very fortunate to be here in this institution and have the support to make this work,” said Dr. Mazzella. “Dr. Ron Falk, Janet Hadar and everyone in medicine has enabled us to focus on the heart of medicine, to help us engage with patients on a more meaningful level.”
Curriculum for Implementing Multidisciplinary Bedside Rounds
The new curriculum consists of an educational booklet and multiple videos for physicians, nurses, care managers, pharmacists, and medical students to implement a multidisciplinary bedside rounding strategy on their teams and units. Educational materials can be accessed here.