What is polycystic kidney disease, or PKD, and how is it diagnosed and treated? Dr. Amy Mottl talks about this genetic disorder with Dr. Ron Falk, and the complications it can cause. She also discusses new treatments available for patients. Dr. Mottl is an Associate Professor of Medicine in the Division of Nephrology at UNC.

– Dr. Amy Mottl
Ron Falk, MD: Hello, and welcome to the Chair’s Corner from the Department of Medicine at the University of North Carolina.
This is our series where we discuss different genetic diseases with physicians who treat patients with these conditions. Last week we talked about cystic fibrosis. Today we’ll talk about a common genetic disorder known as polycystic kidney disease.
We welcome Dr. Amy Mottl, an Associate Professor of Medicine in our Division of Nephrology. Dr. Mottl is an expert in genetics and kidney disease, and she treats patients at UNC who have PKD, or polycystic kidney disease. Welcome, Dr. Mottl.
Amy Mottl, MD, MPH: Thank you.
Polycystic kidney disease and diagnosis
Falk: What is polycystic kidney disease, or PKD?
Mottl: PKD is the most common genetic disease affecting the kidneys. About 1 in 400 to about 1 in 1,000 live births actually will carry a PKD mutation. Some of those people may not ever have ill consequences from the genetic mutation because in some PKD patients, it’s so slowly progressive that it does not manifest in disease. However, the vast majority will have serious chronic kidney disease, often times ending up in end stage kidney disease, where they will require dialysis or a kidney transplant.
Falk: It’s a broad spectrum of disease outcome. How do you recognize the disease? How do you diagnose polycystic kidney disease?
Mottl: There are two overall methods that we can use to diagnose patients with PKD. Generally, and historically, before we had the genetic technology that we have now, we would do imaging studies of the kidneys.
Falk: Ultrasounds.
Mottl: Ultrasounds are usually the first line because they’re inexpensive and they’re benign.
Falk: What do you see?
Mottl: It depends on how far progressed a patient is. Very early on, a patient may have no cysts whatsoever. In childhood, the vast majority of people will be completely asymptomatic. As patients get older, we require more cysts to actually diagnose a patient. If someone is under thirty, they’ll usually need to have at least three cysts in one or both kidneys. As someone gets older, it’s very common to have cysts, especially in older age. Often times in very elderly people, into their seventies, we will require four cysts in each kidney to make a diagnosis.
Actually, these cysts can become very large and very numerous and the kidneys grow along with them. Some of these people will have kidneys the size of footballs or even larger, whereas a normal kidney is about the size of a fist. We’ll see large kidneys with lots of cysts.
Falk: What does a cyst actually look like?
Mottl: It’s a fluid-filled pocket, essentially. As I said, it can form as part of normal physiology of aging or with chronic kidney disease of any etiology (cause), however, these get extremely large and start to occupy a lot of the space of the health kidney tissue. It’s thought that this is why people develop worsening chronic kidney disease.
Falk: The cysts, these fluid-filled balls, grow in size and actually compress otherwise normal kidney tissue and make it so the kidneys don’t function as well over the course of time.
Mottl: Correct.
PKD genetic mutations & testing
Falk: There are two genetic forms of polycystic kidney disease. There are more, actually, but of the adult form of polycystic kidney disease, there are two genetic mutations. Can you tell us a little bit about that?
Mottl: Sure. We’re specifically talking about autosomal dominant polycystic kidney disease. Autosomal dominant diseases actually are passed on through the generations, but all you need is one abnormal genetic mutation in order to actually have the disease. It doesn’t skip generations, and anyone who has the genetic mutation will have the disease.
Falk: Although the disease can be substantially variable from one family to the next.
Mottl: It’s partly dependent on the severity of the mutations. Some mutations will just result in an abnormality of function of the protein which the gene codes for. But in some people, the gene is completely absent, it’s just not translated at all. Those people typically will have more severe disease—earlier onset, more rapid progression of their kidney disease, sometimes more symptoms associated with it.
Falk: The word choice that you have been using and is in the literature can sometimes be confusing to patients is ADPKD, which is autosomal dominant polycystic kidney disease, and that’s what you have just been describing, with really a different kind of disease process from one individual to another, depending upon the severity of the genetic mutation.
Mottl: Yes, but it’s also important to note that there is variability even within a single family, all of whom will carry the same mutation. There are other modifying genes and there are environmental factors that will also potentially influence how early a patient presents symptomatically with their disease and how rapidly it progresses. Unfortunately, we don’t really know what a lot of these genetic modifiers are.
With regards to environmental factors, blood pressure is probably the most important issue that luckily can be modified. If we can bring that blood pressure down, we find that it progresses much more slowly.
Falk: So, you’re trying to avoid hypertension in this population, from an early age and throughout life.
Mottl: Correct. If we have a family with PKD and there is a potentially affected child, we will recommend that they get screened for their blood pressure, and some nephrologists will even recommend yearly urinalyses to detect proteinuria—the leakage of protein into the urine, or hematuria—blood in the urine.
Falk: How does a patient find out they have polycystic kidney disease if there’s no clear family history?
Mottl: Usually they will just present symptomatically. We don’t typically screen for this disease, because it is a rare disease. Some patients will develop pain—flank pain, or pain in their back. I’ve had patients who have gone to the emergency room for this, and a CT scan is done and they see all these cysts and these large kidneys, and they’re diagnosed radiologically. Other patients may have some hematuria.
Falk: Blood in the urine.
Mottl: Correct. Then yet other patients may find that they have abnormal kidney function, on just routine screening with their doctors, and when we do an ultrasound, which is pretty typical to evaluate whether there are structural abnormalities contributing to it, then we’ll see the cysts as well.
Falk: Most patients will know, though, that they have a family history of polycystic kidney disease, from mom or dad in some portion of the family. That can at least raise the possibility of polycystic kidney disease. It’s interesting that so many patients find out by chance.
Mottl: It’s true, and actually about ten percent of mutations are spontaneous. When an embryo is forming, there can be just random spontaneous mutations that occur, so a patient can actually be the first person in their family to manifest with this particular disease.
Falk: Help us understand what “autosomal dominant” really means and how the disease would be passed from generation to generation.
Mottl: We have two copies of any gene that we have, and if there is a very important gene, or a very significant mutation in a gene, then there’s a major change physiologically. Autosomal dominant is a major mutation in an important gene. That means that if you have that mutation, then you will have symptomatic disease.
Falk: And your offspring—your children, have a chance of getting the disease as well.
Mottl: Since we give one copy of each of our genes to our children, all of the children will have a fifty percent chance of having the mutation.
Falk: How does a child find out, or how does a parent determine that their child has polycystic kidney disease, and when do the parents really need to know?
Mottl: The vast majority of people will not have any ill consequences of this disease until they’re at least young adulthood, so we typically don’t recommend screening of children. Some parents choose to know, in which case we can do a genetic test if the mutation is already known within that family. If it’s not, there are other approaches that we can take to define what the mutation is, so that we can test family members. Typically, we do not recommend it, because it can potentially affect the children in terms of anxiety, and the entire family, quite frankly. It can also potentially affect insurability, so in general we don’t recommend that.
Falk: What you would recommend is that the child go to their pediatrician and make sure that their blood pressure is okay.
Mottl: At least on an annual basis, I would say they should have their blood pressure checked, and possibly even a urinalysis.
Falk: A urinalysis, looking for protein in the urine, or perhaps blood, but mostly protein.
Mottl: Right, and actually protein in the urine is another factor that we can modify to some extent, so the more proteinuria that a patient has, generally, the more rapid progression of their chronic kidney disease. There are medications that we can use to try to minimize the amount of proteinuria. These medications are also blood pressure medicines, so they actually impact both of these important factors.
Autosomal recessive PKD
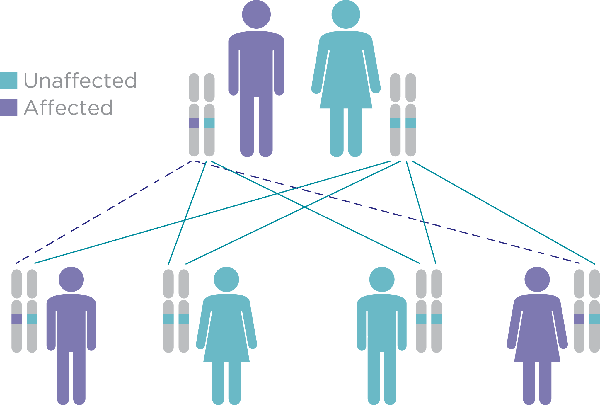
Falk: There are multiple types of polycystic kidney disease and there are differences in the genetic transmission or how an individual passes an abnormal gene from one generation to the next. The most common form of polycystic kidney disease is autosomal dominant, or ADPKD, but there are recessive forms of polycystic kidney disease also—instead of dominant, recessive. Can you describe those to us as well, please?
Mottl: For autosomal dominant polycystic kidney disease, if a person has the mutation, then they will manifest with the disease, whereas autosomal recessive polycystic kidney disease is very different.
You actually need to have two copies of the gene – you have to have a mom and a dad who are both carriers of these genetic mutations. They are not affected with this disease, but if they happen to pass on the mutated form of this gene to their offspring, and that offspring gets both copies, then they will have the disease. That is a very different disease from ADPKD. Autosomal recessive polycystic kidney disease is one we see predominantly in childhood.
Falk: Which is more common, autosomal dominant, or the recessive variant?
Mottl: Autosomal dominant is by far more common. That’s really because of the way it’s transmitted.
Falk: Two abnormal genes rather than one abnormal gene.
Mottl: Right.
Treatment for PKD
Falk: Let’s talk a little bit about treatment. You’ve already said some approaches: make sure hypertension is well-controlled—get that blood pressure down, and then if there is protein in the urine try to lower that amount of protein, again by using drugs that modify blood pressure that also can modify the amount of protein in the urine.
Mottl: Right. There’s a class of medicines called renin-angiotensin inhibitors which basically inhibit a pathway of hormones that can play a significant role in the progression of hypertension and proteinuria. With these medications, it can hit both of these factors.
Falk: Are there treatments that are specifically designed at the underlying cause of polycystic kidney disease, or are there treatments available that decrease the size of cysts, or their growth?
Mottl: You know, it’s interesting, because there is specifically one class of medicine which are antidiuretic hormone antagonists.
Falk: ADH inhibitors.
Mottl: Yes, ADPKD, or autosomal dominant kidney disease is actually an abnormality in a protein which signals the cell how to react to its external environment.
It’s actually located on something called a “cilia,” so ADPKD is what we call a “ciliopathy.” Cilia are these finger-like projections emanating from a cell into its environment, so that it can sense what is happening in that environment. These particular cilia are located on cells which line the tubules which collect the urine once it’s filtered within the kidney.
The mutation that patients with ADPKD carry actually interferes with a pathway located within these cilia, to be able to respond to the environment within the tubules that allow urine to flow. There’s actually a hormone called antidiuretic hormone or ADH, which can cause further problems. So, when we inhibit this hormone from acting, it actually can slow the progression of this disease. Recently, actually just in May of 2018, a drug that does this very thing was recently approved by the FDA. It’s called Jynarque.
The one issue for this medication is that is does have a lot of negative side effects. It can cause elevations in the liver enzymes which potentially can lead to liver damage, but it’s also really hard to tolerate because one of the functions of antidiuretic hormone is to allow the absorption of water from the urinary tract, so by inhibiting it, all of the water that a person drinks is excreted in the urine. People have what we call “polyuria,” they have excess volumes and frequency of urination and because of this they can get dehydrated very easily. Patients have to drink a lot of water, and they have to go to the bathroom a lot, which can really interfere with their quality of life, particularly at night when they’re trying to sleep.
Falk: The kidney filters about 180 quarts of blood a day, and you know you don’t urinate 180 quarts of blood a day, and the reason why you don’t is that you have tremendous absorptive capacity in kidneys that decrease the amount of urine to about one and a half to two and a half quarts of urine a day. One of the ways that the kidney holds on to water is through this hormone, ADH. What you’re describing is the inhibition of ADH that now causes an incredible amount of urination that requires a lot of drinking of water, just to keep up.
Mottl: Right, and actually in the trials, about twenty-five percent of the participants could not even tolerate it to continue treatment with the drug.
Falk: It does apparently work, to a certain extent, however.
Mottl: It does, so part of the trials for PKD generally involve serial imaging—repeated ultrasounds or MRIs to look at the volume occupied by the cysts. It does appear to decrease the rate of growth of these cysts. It even has some signals wherein it slows the rate of progression of kidney disease, but the rate at which it slows it is fairly mild. Typically, somebody would have to take the drug for at least ten years to delay their progression to kidney failure by one year.
Falk: In other words, this drug may work, it has real side effects, mostly an inability to sleep because you’re drinking water so much, and you have to take it for a long period of time for an effect to be observed. Would you then recommend anybody taking this drug?
Mottl: I think that each patient has to have that conversation with their nephrologist and have a serious discussion on the downsides of this drug. Some people have very rapid progression of disease, and may want to try it. It just has to be individualized according to the patient.
Complications from PKD
Falk: Patients with polycystic kidney disease can have disease outside of their kidneys. Where else can it be?
Mottl: Most people will actually also have cysts in their livers, but interestingly, those cysts actually don’t seem to cause a problem. There is generally not progressive liver disease in these patients. They can also have cysts in their pancreas. Women can have cysts in their ovaries, there are even cysts in the part of the reproductive system of men.
There are also some other ways that it can impact other organ systems. For instance, many people will have mitral valve prolapse—this is an abnormality in the way that one of the heart valves closes. We used to treat with antibiotics prophylactically for patients who were undergoing dental procedures or invasive procedures, but we’ve now found out that we don’t need to do that. It is generally thought to be a pretty benign abnormality, and there’s really no long-term ill consequences from that.
Another one that can potentially have a major consequence is we can see brain aneurysms in some people. Interestingly, it tends to follow within families, so when I have a patient whose father or grandparent might have had a brain aneurysm, I will seriously discuss potential screening with brain MRI’s to look for it. It’s a complicated issue, however, because there’s not a lot that we can do about it, but it is something that should be discussed with each patient.
Falk: When a patient with PKD comes to visit you, and you’re seeing them in clinic, what are you looking for? What do you do in one of those clinic visits?
Mottl: I am asking the patient about any symptoms they may have from their PKD—if they’re having any flank pain–
Falk: Because of size.
Mottl: Because of the size of the cyst, right. Sometimes these cysts actually can rupture and cause significant pain. If it’s actually a blood-filled cyst, which in and of itself is benign, if it happens to be blood-filled, and it ruptures, patients can have serious hematuria—blood in their urine—that they can visibly see when they urinate. That can be very disconcerting to patients. It’s actually generally not concerning.
Falk: Except it hurts.
Mottl: It does hurt. That’s very true, but patients’ main worry is that they’re going to bleed seriously, but it doesn’t take much blood to turn the whole toilet bowl red. It’s generally very self-limited, and I just ask patients to let me know if it doesn’t start to clear up over the course of a couple of days.
Thinking about symptoms, talking about polyuria—polyuria is when somebody has to go to the bathroom a lot—this is something that can sometimes cause problems, particularly at night if the patient has to go to the bathroom a lot. One of the first manifestations of polycystic kidney disease can sometimes be just having to go to the bathroom a lot because it impacts the ability to concentrate or hold on to the water in the kidney.
Then, I’m also monitoring them with labs, so I’m following their kidney function with what we call a serum creatinine, and I’m also looking at their urine to determine how much protein there is. I’ll generally quantify precisely how much that is, and I’ll follow that on an annual basis, because as we said before, the more protein a patient has in their urine, the worse the prognosis, and there are things we can do about that.
Falk: You also want to make sure that their blood pressure is under good control.
Mottl: Absolutely, that’s actually the most important thing that we do in clinic.
Falk: You described a cystic bleed. Cysts can also get infected. That doesn’t happen commonly, but when it does happen, it is a real concern. How do you treat an infected cyst?
Mottl: When a urinary tract infection—an infection that can occur within the urinary tract from the urethra to the bladder, all the way up to the kidneys—if it occurs in the kidney itself, when a person has an infected cyst, we call that “pyelonephritis.” That’s a more serious infection than if someone just has an infection in their bladder. There are specific antibiotics that we would want to use that can penetrate that cyst. Sometimes antibiotics can’t get into the cyst like it needs to in order to treat the infection. Often times, we can do this with oral drugs at home, but sometimes patients need to be hospitalized.
Lifestyle changes that can help PKD
Falk: What other kind of lifestyle changes would you suggest a patient do that improves their long-term outlook?
Mottl: There’s no specific diet that a patient necessarily needs to follow, although we always recommend a healthy diet—fruits, vegetables, lean meats, etc. Some investigated looking at restricting how much protein a patient consumes, and it’s not clear whether that helps. Typically, we will just recommend that patients consume the recommended daily protein intake which is about .8 grams per kilogram of body weight.
I also tell all of my patients that they should get regular exercise, because one of the consequences of having chronic kidney disease of any cause is that patients are at increased risk for cardiovascular disease. Regular exercise and good nutrition is critical for this.
Falk: Healthy lifestyle.
Mottl: That’s right.
Falk: Dr. Mottl, thank you so much for being here today.
Mottl: It was my pleasure. Thank you for having me.
Falk: Thanks so much to our listeners for tuning in. Next time, we will be talking with Dr. Raj Kasthuri, about hereditary hemorrhagic telangiectasia, HHT, a genetic disease that affects blood vessels. You can subscribe to the Chair’s Corner on iTunes, SoundCloud, or like us on FaceBook.
Visit these sites for more information:
// var audio; var playlist; var tracks; var current; init(); function init(){ current = 0; audio = $(‘audio’); playlist = $(‘#playlist’); tracks = playlist.find(‘li a’); len = tracks.length – 1; audio[0].volume = .90; playlist.find(‘a’).click(function(e){ e.preventDefault(); link = $(this); current = link.parent().index(); run(link, audio[0]); }); audio[0].addEventListener(‘ended’,function(e){ current++; if(current == len){ current = 0; link = playlist.find(‘a’)[0]; }else{ link = playlist.find(‘a’)[current]; } /* run($(link),audio[0]); stops from going to next track */ }); } function run(link, player){ player.src = link.attr(‘href’); par = link.parent(); par.addClass(‘active’).siblings().removeClass(‘active’); audio[0].load(); audio[0].play(); }