Heart failure is a common cause of hospitalization and re-hospitalization, particularly in individuals over the age of 65. And approximately half the people who are hospitalized with heart failure (HF) have reduced ejection fraction (HRrEF). A normal ejection fraction is more than 55%, while heart failure with reduced ejection fraction is 40% or less, which means the amount of blood pumped is not enough to meet the body’s needs. A new project will design care protocols to enhance patient care and subsequently decrease hospital admissions and ED visits for HFrEF.

Laura Loehr, MD, PhD, MS, associate professor in general medicine and clinical epidemiology, is a cardiovascular epidemiologist leading the Department of Medicine’s latest Value-Care Action Group (VCAG) project with Jamie Cavanaugh, PharmD, CCP, associate professor in general medicine.
“Guideline recommended therapy for heart failure with reduced ejection fraction is revolutionary in preventing heart failure hospitalizations and mortality, but it is complicated and includes treatment with ace inhibitors or angiotensin receptor blockers, beta blockers and diuretics,” said Loehr.
“Getting patients up to the recommend medical therapy for heart failure with reduced ejection fraction (HFrEF) will require multiple visits for the addition of recommended medications and the advancement of dosages, while monitoring for side effects.”
Loehr adds patients with HFrEF frequently have co-morbid conditions, which makes optimizing heart failure medications more difficult. The project will be designed for optimizing medications, managed by Cavanaugh, who is a clinical pharmacist practitioner. Medical student Paige Della-Penna will work with Loehr on the self-care part of the project.

“Optimization of guideline recommended medications reduces heart failure morbidity and mortality. By avoiding heart failure exacerbations, patients will need to access the ED and hospital less often, thereby reducing the total cost of care,” said Cavanaugh. “Heart failure regimens can be complex and require significant patient education to achieve a patient centered regimen with high adherence. We will work with patients to provide education and optimize their regimens in a way that best fits their needs. That includes providing some visits by video and phone to allow flexibility for patients with barriers to coming in for a visit.”
Preliminary Work
In 2017-2018, Cavanaugh led a retrospective analysis of patients who had been hospitalized for HFrE, working with two pharmacy students.
The analysis showed 228 patients with an EF < 35 were not following guideline recommended therapy of an ACE inhibitor or beta blocker. Of the patients with HFrEF, 30% of the patients were not on an ACE/ARB, and 18% patients were not on a beta blocker. A prior survey of providers also showed reluctance to titrate up meds when a patient was stable, with a preference to defer to cardiology, although uptitration of guideline recommended therapies (when tolerated) for HFrEF is recommended, even when the patient is stable.
In 2019, Amy Shaheen, MD, joined the group to focus on implementation in the General Internal Medicine Clinic. Loehr joined the VCAG group in 2020, to continue efforts focused on improving care for heart failure patients.
“It’s not just re-hospitalization that is concerning,” Loehr said. “We know that significant mortality is associated with heart failure with 30-day and one-year case fatality of approximately 10% and 30% respectively. Having a structured and close follow-up with patients who have been hospitalized for HFrEF will enhance their follow-up care.”
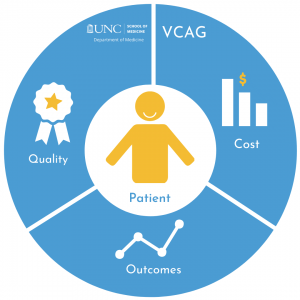
This project is one of many Value Care Action Group improvement efforts taken up by the department of medicine. Champions in each medicine division are currently encouraging the review of current practices, looking for improvements for high-value outcomes in healthcare. High-value is defined by the quality of patient-centered care achieved per unit of cost derived from measuring health outcomes against the cost of delivering the outcomes. Ron Falk, MD, chair of the department created the group in 2016. Scott Keller is the director of business development keeping the team focused on value-oriented care models. Darren DeWalt, MD, functions as medical director for the team and helps define the projects. John Vargas is the project manager.