UNC is on pace to become one of the few sites in the U.S. to incorporate intestinal ultrasound as an imaging technique for managing Inflammatory Bowel Disease.
For gastroenterologists, getting eyes on the gut traditionally requires timely MRI testing or endoscopy procedures. This means patients grappling with Inflammatory Bowel Disease (IBD) must return multiple times to collect the necessary data for managing their treatment regimen. However, a new wave of technological advancements and streamlined training processes are providing GI specialists the ability to assess treatment efficacy and disease progression within minutes.

Introducing Intestinal Ultrasound
Before, physicians managing IBD relied on stool and blood markers, pediatric growth indicators, and endoscopic signs of bowel healing. With access to high-resolution images of the bowel, provided by the ultrasound, gastroenterologists can measure the thickness of the bowel as a measure of inflammation in real-time during routine appointments.
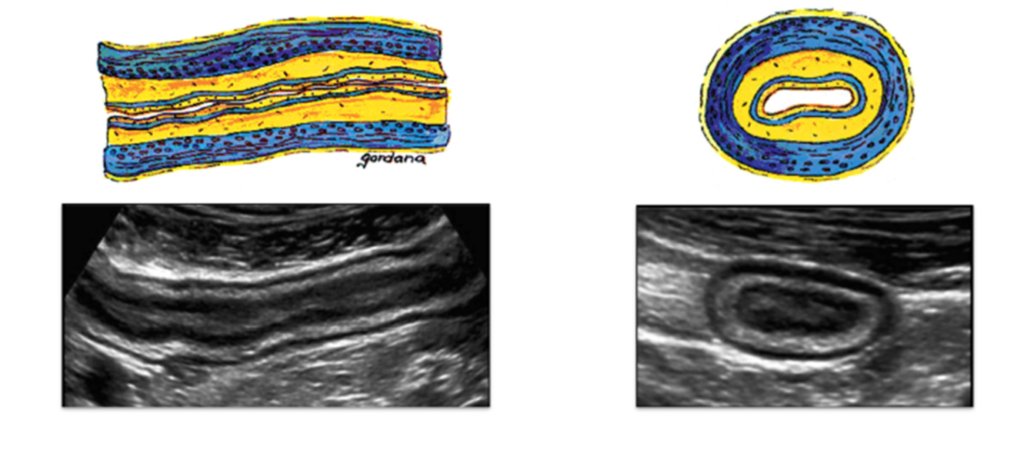
This revolutionary technology can display either the longitudinal or cross-section area of the bowel. Starting from the lumen (middle of the intestine), gastroenterologists can meticulously measure each layer, including the submucosa, muscularis propria, deep mucosa, and more, providing a comprehensive evaluation of inflammation and how the bowel is responding to treatment.
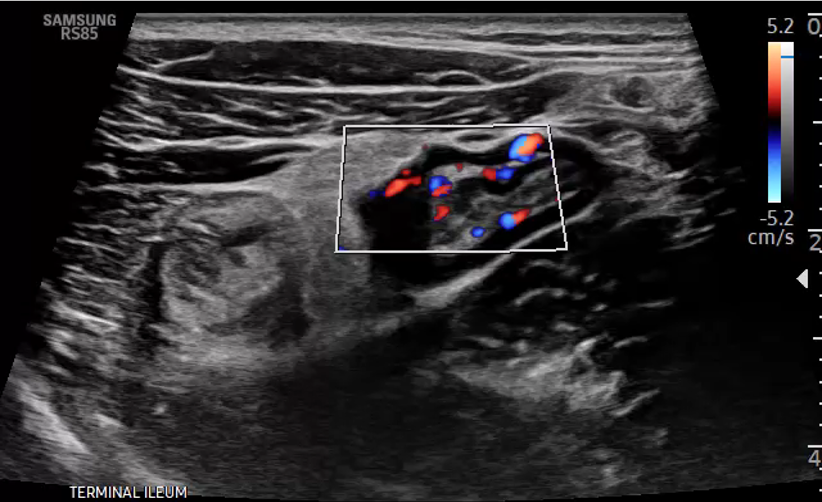
In IBD patients with bowel thickness, a specialized Doppler enhances diagnostics. Gastroenterologists can identify blood flow, visualized as blue and red signals on ultrasound, effectively differentiating active inflammation causing the bowel to appear thick from scarring.
Moreover, this advanced imaging technique enables the detection of abscesses, inflammatory fat, and loss of preservation of the bowel wall layer stratification. The IUS can be completed in less than 10 minutes during a routine care visit. Ultrasound is also beginning to emerge as an endpoint in IBD clinical trials. With these insights, gastroenterologists can refine treatment plans and tailor interventions to address specific manifestations of IBD.
The new care model does require clinics to purchase an expensive ultrasounds machine with high quality B-Mode, Doppler effect and two transducers. Training gastroenterologists to use the technology can also be a large financial investment. A generous donation from The Loewenthal Family Fund has supported the implementation of IUS at UNC.
“The power of philanthropy in medicine is evident by the development of this innovative intestinal ultrasound program,” Dr. Long said. “Gifts such as the one from the Lowenthal Family Fund will change lives for the better, and allow UNC to provide cutting edge care to our population of patients living with IBD.”
Insight from Europe
Although this imaging technique is not common practice in America, specialists in Europe have been using ultrasound as an imaging modality for patients with IBD for a decade. Through overseas studies patients have expressed the use of IUS helps them:
- Learn more about the disease
- Understand where symptoms come from
- Make informed decisions about managing their IBD
“Some of the medications can have complications or side effects,” Dr. Long, Professor of Medicine said. “When you’re showing a patient their inflamed bowel wall on ultrasound while explaining why we need to modify treatment, it helps them make an informed decision.”
The International Bowel Ultrasound Group, based in Europe, has created a certification program for gastroenterologists interested in learning IUS techniques. Comprised of three modules, the training requires three days of workshopping followed by up to four weeks of hands-on training at a certified center. Finally, specialists must demonstrate the ability to use IUS at an advanced workshop and through testing.
The University of Chicago, Mount Sinai Health System and Houston Methodist Hospital are currently the three certified sites actively using this technology in the United States. Drs. Long and Barnes are set to complete their training in May. Hans Herfarth, MD, PhD, Director of the IBD Center at UNC, is expected to be certified in 2025.
Putting the Probe in Program
UNC’s IBD center stands as one of the largest in the country, with over 3,000 patient visits from across the Southeast every year. Limiting the number of times someone has to return for testing would pave the way to more efficient and personalized care.
The non-invasive nature and lack of radiation makes IUS especially valuable for pregnant and pediatric patients.
Dr. Long envisions IUS training being implemented into the UNC Division of Gastroenterology’s Fellowship Program. These specialists would then be equipped to use IUS in clinic, ultimately shifting the way providers manage treatment for IBD patients.