Calculating the risk of heart failure, cardiogenic shock, and death at the time of an angioplasty procedure can be critically important because early initiation of blood pressure support can improve survival.
For the interventional cardiologist treating a patient with a heart attack, nothing is more important than being able to make the best decision when the clock starts ticking. A heart attack that completely blocks a major artery puts a patient at the highest risk for death. When a major artery is blocked, heart tissue is starved for oxygen and begins to die very quickly.
This type of heart attack, known as a STEMI (ST-segment elevation myocardial infarction), leads to significant changes on an electrocardiogram. The cardiologist treats the heart attack by opening the blocked artery to perform an angioplasty (angioplasty performed for STEMI is known as emergency primary percutaneous coronary intervention or PPCI). This procedure involves threading a catheter to the heart, putting a wire in the artery and then tracking a balloon over the wire. The balloon is inflated and deflated at the site of the blockage to restore blood flow, and in most cases, a stent is implanted. Then, the cardiologist must determine if the patient needs mechanical support for a failing heart. Calculating the risk of heart failure, cardiogenic shock, and death at the time of the procedure can be critically important because early initiation of blood pressure support can improve survival.
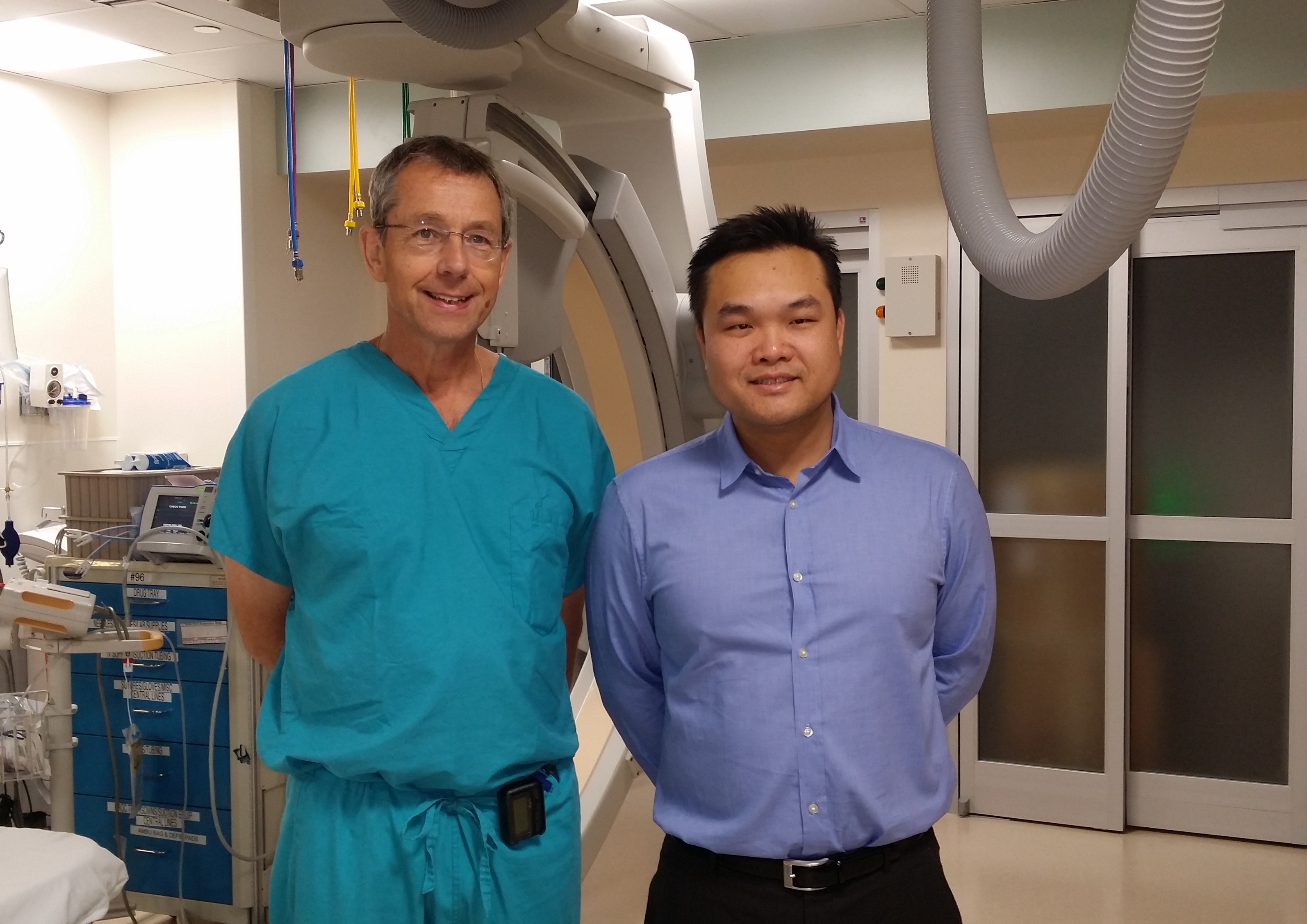
Two interventional cardiologists at UNC, George “Rick” Stouffer, MD, and Michael Yeung, MD, led a study that showed a simple hemodynamic ratio determined at the time of angioplasty provides a rapid prediction for in-hospital mortality in STEMI patients.
“Our results show that a simple index predicted mortality at a level consistent with the more commonly used and more cumbersome prognostic indices,” said Dr. Stouffer, chief of cardiology, co-director of UNC’s McAllister Heart Institute and the Henry A. Foscue Distinguished Professor of Medicine. “Knowing which patients will likely survive this type of heart attack enables us to treat them much more aggressively.”
The researchers conducted a retrospective single-center study examining simple hemodynamic parameters obtained at the time of cardiac catheterizations. Current 30-day mortality rates for patients with STEMI range from 2.5% to 10%, and 10.5%–24% of those patients require mechanical support, such as a balloon pump or impella.
“Our question was, when people come in with a heart attack, how do we identify those–while on the table in the cardiac catheterization lab–who are at high risk of dying versus the people who will make it,” said Dr. Yeung, an assistant professor of medicine affiliated with UNC Cardiology at Nash in Rocky Mount, who also leads UNC’s cardiology mission trips to Nicaragua twice annually. “We’re looking at how much they’re congested and how well the heart is pumping, to determine whether they will do well or not.”
The project examined the utility of an index based on systolic blood pressure (SBP) and left-ventricular end-diastolic blood pressure (LVEDP) ratio measured at the time of PPCI. Researchers examined adult patients age 18 and older treated at UNC between 2007 and 2011. They found the SBP/LVEDP ratio was an effective, rapid way to calculate risk.
“When we have a patient on the table, in the middle of the heart attack, we don’t have a lot of time,” said Dr. Yeung. “But what we’ve found is that LVEDP, a measurement of filling pressures and systolic blood pressure, a measure of how well the heart is pumping, is all that’s necessary to make a rapid assessment of the size of the heart attack and risk of death. It’s a simple way to calculate in our head how sick the patient is.”
This first phase of the study was recognized as the editor’s choice for Catheterization and Cardiovascular Interventions, published by the Society for Cardiovascular Angiography and Interventions Foundation in September, 2017.
The second phase of the study, soon to be published, looks at hemodynamic parameters and how they correlate to the size of the heart attack.
Since 2008, UNC Medical Center has been a leader in STEMI treatment and has been recognized annually by the American Heart Association for excellence in STEMI care.
Other participants in this study include Mike Sola, MD; Kiran Venkatesh, MD; Melissa Caughey, PhD; Rob Rayson, MD; and Xuming Dai, MD.