Listening to Your Body
Abrupt swelling of the entire arm, numbness, and tingling in the hand and fingertips, arm turning bluish. All unusual things happen to an active and otherwise healthy person. “It makes you think about how well you know your body; how much are you aware of what it might be telling you,” recalls Sydnee Yates as she talks about her medical journey. “It makes you learn a lot about yourself. Some people have symptoms, and they don’t ever get tested. The entire time, there was a part of my mind wondering if I was being overdramatic, maybe overthinking. It was extremely relieving when doctors explained to me that my symptoms and condition were very much real and would require surgical intervention.”
 28-year-old Sydnee sits on her couch, relaxed in a t-shirt, her hair cropped in a short bob with bright pink ends. Her lip ring an extension of herself as she looks into the computer camera and, over a zoom interview, recounts her experience at UNC Medical Center in Chapel Hill.
28-year-old Sydnee sits on her couch, relaxed in a t-shirt, her hair cropped in a short bob with bright pink ends. Her lip ring an extension of herself as she looks into the computer camera and, over a zoom interview, recounts her experience at UNC Medical Center in Chapel Hill.
In February 2021, Sydnee was working the third shift at Michael’s, an art supply store in Durham, stocking shelves when she noticed a numbing feeling in her right arm. Sydnee describes the sensation, “It felt like when you fall asleep, and you wake up, and your arm is numb, and right before it starts tingling, because when your arm starts tingling, it means blood circulation is getting through. It’s the moment right before that. If you were to touch me, I could still feel that you were touching me, but not really.”
Also concerned about the blue tint and the swelling of her arm, she contacted her parents. Her father is an EMT, and her mother is a cardiac sonographer. Her mother recommended she go to her primary care physician. However, since her PCP did not have any openings, she went to local urgent care instead. The team there did an EKG and ruled out a stroke. “Honestly, the woman at Urgent Care dismissed me a little bit. She told me that the mind could do crazy things to the body,” says Sydnee. “I’ve struggled with some mental health issues in the past, so I figured she could be right.”
Sydnee went home and took the next day off work, relaxing around the house. The following day she went to work and began to experience the same symptoms. Later that night, after showering, she took another look at her body. She was surprised to see that the blood vessels underneath her right armpit were bright blue. “It looked like someone had been choking out my arm.”
Another trip to urgent care, but they sent her straight to the emergency room at UNC Medical Center in Chapel Hill. The ER team did multiple tests to figure out the issue, and in the early morning hours, they discovered that Sydnee had blood clots in the veins of her right shoulder. At this point, a physician came in to talk with her about a condition they thought she had called Thoracic Outlet Syndrome (TOS).
Diagnosis
 TOS is a group of symptoms that occur when the blood vessels or nerves in the space between the collarbone and the first rib are compressed. This often occurs in competitive athletes who make repetitive overhead motions, like baseball pitchers or swimmers, but can happen to anyone.
TOS is a group of symptoms that occur when the blood vessels or nerves in the space between the collarbone and the first rib are compressed. This often occurs in competitive athletes who make repetitive overhead motions, like baseball pitchers or swimmers, but can happen to anyone.
Specifically, Sydnee had Venous Thoracic Outlet Syndrome, which affects 5% of all patients with TOS. Venous TOS occurs when the subclavian vein that runs under the collarbone is pinched by the first rib. Eventually, enough scar builds upon the vein that it is completely blocked and a blood clot forms.
The initial phase of venous TOS is usually asymptomatic, involving compression injury of the vein between the clavicle and first rib, scar tissue formation, contraction around the outside of the vein, and fibrosis and wall thickening within the wall of the vein itself. A blood clot or deep vein thrombosis (DVT)eventually forms in the damaged subclavian vein, leading to obstruction and symptoms like those experienced by Sydnee. Substantial arm swelling and bluish discoloration are very common. The tingling and numb sensation can also occur related to the swelling or to irritation of the nerves that course next to the vein.
“During that hospital visit, they did discuss with me TOS, but I didn’t really understand,” recalls Sydnee. “They talked to me about the procedure, which included taking out a rib, and I was like, wait…what? I was completely overwhelmed, and all I wanted to do was go home, snuggle with my cat and digest everything that had happened to me in the last 24 hours.”
Once the blood clots were gone, Sydnee went home to recover with blood thinner medication, and an appointment was set up with the TOS team to plan for the next step in her care – rib resection. However, before her appointment, Sydnee was getting ready to go to work one night, and she started to experience the numb feeling in her hand again. This time she understood its significance and headed directly to the ER, where an ultrasound found that the clot had returned. “At some point, after we did the ultrasound, I told the nurse that somebody’s got to come to talk to me because I have questions and I need answers. I’m low-key freaking out over here.”
Getting Answers and Creating a Plan
Dr. Katharine McGinigle, Co-Director of the TOS program and Surgical Director of ERAS, and her Advanced Practice Provider Jessica Curcio met with Sydnee and her parents to talk about Venous TOS and to answer all questions they had about the procedure. “It was like a breath of fresh air. Talking to all of Dr. McGinigle’s team, they were all just absolutely wonderful. Jessica reassured me that the team would be by my side. She was amazing to talk to. So they let me go home, pack a bag, and prepare myself for the surgery scheduled for Monday.”
Sydnee returned and was ready for the next steps, the first of which was the removal of the blood clot. During the procedure, Dr. McGinigle noticed that her minor pectoral muscle was so tight that it was causing damage to the other side of the subclavian vein, so they would have to make a second incision to cut the muscle and open some more space. But before surgery could take place, Sydnee had some personal concerns she shared with the team.
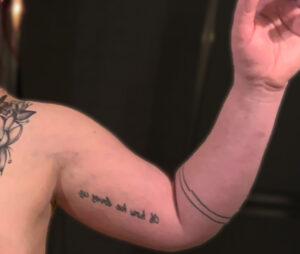
“When I was in the operating room prep, I requested that I not have to take out my piercings. I knew they would be taking out a piece of my body, my rib, and I felt like my piercings are part of who I am. They understood and allowed me to keep them in during the procedure. The other thing I brought up was the tattoo on my shoulder. All I kept thinking was that the tattoo would be destroyed after the surgery. I shared this fear with Dr. McGinigle, and she immediately took out her phone, got a picture of it, and took my concerns seriously. It’s crazy, but where she actually made the incision on the flower, it looks cooler than it did before. Dr. McGinigle’s bedside manner is phenomenal.”
Dr. McGinigle brought Sydnee into the OR. She made an incision above the collarbone, exposing the vital nerves and blood vessels to and from the arm. They divided the muscles that attached the first rib to the neck, allowing them to expose the rib and then remove it, which opened up the space, causing pinching and damage. Finally, they then carefully cut the scar tissue away from the vein and nerves to give them a fresh start and release them from the inflammatory scarring process they had been going through.
The other incision made just inside the shoulder where a tanktop strap would be was made to cut the minor pectoral muscle. This is a small muscle that connects the rib to the shoulder and can also cause pinching and damage to the underlying vein and nerves. Once this muscle is cut, the vein was able to expand again.
 The next step for Sydnee was recovery. “When I woke up the next day, it was pretty painful. Having a rib removed is pretty traumatic. It hurt to talk or cry or do anything. But all the nurses at UNC were awesome and helpful.”
The next step for Sydnee was recovery. “When I woke up the next day, it was pretty painful. Having a rib removed is pretty traumatic. It hurt to talk or cry or do anything. But all the nurses at UNC were awesome and helpful.”
She was in the hospital for five days and was discharged with a follow-up appointment the following Friday. “Now I can’t really lay down for too long, and I can’t really sit up for too long. I’m up and down all the time. Dr. McGinigle said that it should take about six weeks for me to fully get back to where I don’t really notice it.”
TOS Team at UNC
The UNC TOS team is a multidisciplinary team led by the Division of Vascular Surgery. In addition to Dr. McGinigle, Dr. Luigi Pascarella is a vascular surgeon who also performs operations to treat TOS. Additionally, Dr. Andrew Lobonc is a pain anesthesiologist who helps with the diagnosis and management of patients with TOS and nerve pain. The patients are also supported in their outpatient care by Jessica Curcio, ND PA-C, Kristin Walsh, NP, and Sarah Miller, RN, as well as many physical therapists throughout the state. This team is unique in that they perform a high volume of these specialized operations and has a depth of experience in patient-centered care for this rare condition.
“I’m just super grateful for Dr. McGinigle and her team. They made this entire thing a lot easier to process. Once they finally got into the picture, they made me feel like I wasn’t a burden, and I wasn’t asking stupid questions. They were really awesome to work with and have on my side.”
