PGY2 Infectious Diseases Pharmacy Resident Ethan Rausch snags award at Making a Difference in Infectious Diseases Conference
Ethan Rausch, PharmD, was recognized with the Top Trainee Research award during the 25th Annual Making a Difference in Infectious Diseases Antimicrobial Stewardship Meeting in Orlando, Florida earlier this week. His research explored the efficacy of non-carbapenem antibiotics for treating resistant Enterobacterales. Rausch is a post-grad year two pharmacy resident at UNC Main Campus working alongside the Carolina Antimicrobial Stewardship Program, with the Residency Program Director and CASP Pediatric Infectious Diseases Pharmacist Bill Wilson, PharmD. Wilson is a study co-author.

“Patients with infections caused by ceftriaxone-resistant Enterobacterales infection are very sick. Carbapenems have been the go-to treatment for this fairly common condition,” Rausch explained. “But with resistance to carbapenems growing, it’s important to take a closer look at how well patients have recovered using other treatment options that may present less resistance risk.”
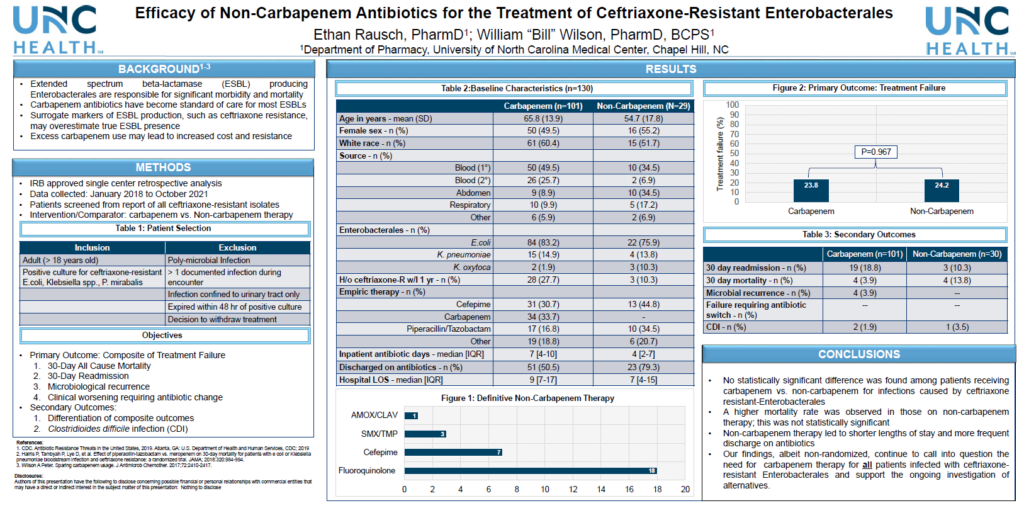
Rausch analyzed nearly four years of UNC Medical Center patient data to compare those treated for ceftriaxone-resistant Enterbacterales. Of the 130 adult inpatients identified with a ceftriaxone-resistant isolate outside of the urinary tract, 29 (29%) received a non-carbapenem treatment for E. coli, K. pneumonia, or K. oxytoca infections. The rest received a carbapenem. As this was a retrospective study, all treatment decisions were made by healthcare providers based on the complete clinical details of their patients.
For both patient groups, treatment was effective. Rausch found no differences in a composite outcome of treatment failure (30- day patient readmissions, 30-day mortality, microbiological recurrence, and failure to respond to systemic therapy necessitating antibiotic change) for carbapenems versus non-carbapenems (24/101 [24%] and 7/29 [24%], respectively; p=0.967). When considering each component of the composite outcome, there were potential clinical differences between the two groups: more infectious diseases-related readmissions in the carbapenem group (18.8% vs. 10.3%) and higher mortality (3.9 % vs. 13.8%) in the non-carbapenem group. Rausch reported that most deaths in the non-carbapenem group were unrelated to the infection. Additionally, no difference between the groups in onset of C. difficile infection, a risk of antibiotic treatment. Notably, non-carbapenem therapy led to hospital stays that were, on average, two days shorter than patients treated with carbapenems, and these patients were more frequently sent home from the hospital with antibiotics.
“These findings are encouraging, although limited by effect size and indication bias for which we were unable to control,” Rausch reflected. “However, I am optimistic that patients did well with non-carbapenem treatment and believe future research will assist in unpacking when and where a non-carbapenem may be utilized for certain ceftriaxone-resistant Enterobacterales.”