Antimicrobial resistance is on the rise worldwide, notably among gram-negative bacteria, known for their propensity to resist multiple antibiotic agents which threatens the likelihood of treatment success. As rising resistance rates limit antimicrobial options, dose optimization is key to clinical success. For β-lactam antibiotics, the best predictor of bacterial killing is the proportion of the dosing interval in which free drug concentrations exceed the minimal inhibitory concentration (MIC) of the organism (fT>MIC). One method to maximize time-dependent bactericidal activity of β-lactam antibiotics is the administration of prolonged infusions given over three to four hours. This approach, in comparison to conventional 30-minute infusions, results in lower peak concentrations and longer durations of free drug concentrations above the MIC.
The UNC Hospitals’ Clinical Microbiology Lab recently changed the way it reports cefepime and piperacillin-tazobactam susceptibilities for Enterobacterales with the addition of “Susceptible Dose Dependent” (SDD) category instead of “Intermediate”, in accordance with Clinical and Laboratory Standards Institute (CLSI) interpretive criteria. Commonly encountered Enterobacterales organisms include E. coli, Klebsiella spp., Enterobacter spp., Proteus spp. and Serratia marcescens. At UNC Hospitals, pathogens reported as SDD to cefepime or piperacillin-tazobactam should be treated with the following dosing regimens:
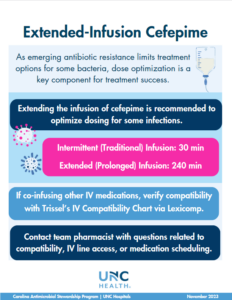
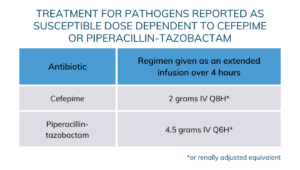 Extended infusions are now orderable in Epic for both piperacillin-tazobactam and cefepime. In addition to the treatment of SDD organisms, extended infusion may be preferred in patients with difficult-to-treat infections and those with special pharmacokinetic considerations such as critical illness. If starting a patient on extended infusion therapy, the initial loading dose should be administered over 30 minutes followed by an extended infusion regimen according to renal function. Contact your team pharmacist if IV-line access is limited or if patients are receiving other medications concurrently to verify medication compatibility.
Extended infusions are now orderable in Epic for both piperacillin-tazobactam and cefepime. In addition to the treatment of SDD organisms, extended infusion may be preferred in patients with difficult-to-treat infections and those with special pharmacokinetic considerations such as critical illness. If starting a patient on extended infusion therapy, the initial loading dose should be administered over 30 minutes followed by an extended infusion regimen according to renal function. Contact your team pharmacist if IV-line access is limited or if patients are receiving other medications concurrently to verify medication compatibility.
Stephanie Hill, PharmD, is a PGY2 at UNC Hospitals.