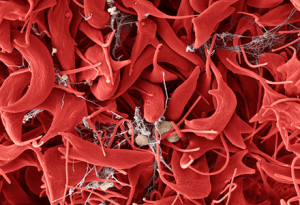
Sickle cell disease affects over 6,000 North Carolinians. Approximately 80 to 100 infants are diagnosed with the disease every year. The inherited disorder causes red blood cells, which transport oxygen throughout the body, to form a sickle or crescent moon shape. These sickle-shaped cells become hard and sticky, clogging the blood vessels. As a result, the tissues in the body are deprived of oxygen. Poor oxygen delivery can cause organ damage and significant pain and edema throughout the body.
Treatment for the disease is often difficult. It requires frequent blood transfusions, chemotherapy, and medication. Although a few new drugs for sickle cell have popped up over the years, they all come with a hefty price tag.

Tara Alin, ANP-BC, a nurse practitioner within the Division of Hematology in the Department of Medicine and provider in UNC’s Sickle Cell Program, has been appointed to the Governor’s NC Appointed Council on Sickle Cell Disease and Other Blood Disorders. In this role, Alin will be working with North Carolina legislators to assist sickle cell patients in obtaining the drugs they need to live well with sickle cell.
“Sickle cell disease is a chronic illness”, said Alin. “We’re in it for the long haul. Once patients transition from pediatrics to adult hematology, we’re still taking care of them. And we do so until the end of their lives. It is our hope that with newer therapeutics that they’re going to live for a really long time, which hasn’t always been the case.” She first visited the Governor’s Council in 2019 as a new North Carolinian. What she discovered seated around a large conference table was a diverse array of people who all were all aimed towards the same goal: to make sickle cell disease more manageable for patients and families in North Carolina.
The 15-member advisory group is comprised of persons and families affected by sickle cell disease, community-based organization representatives, hematologists, social workers, doctors, and public health officials.
“Every member of the council, from the chairperson to the junior members, was incredibly thoughtful, incredibly kind, and very welcoming,” said Alin. “I am just honored to be a part of a group like that. I know that we are going to work incredibly hard to try to bring better sickle cell care to North Carolina and to reinforce the excellent care that we already have.”
Alin is the council’s only Advanced Practice Provider. Her physician partners are usually honored, thus her appointment is even more special. Alin adds that as an Advanced Practice Provider, she may bring a fresh perspective that is slightly different from the norm. Alin is also establishing a precedent, as UNC has been absent from the council in recent years.
“As the state health organization in North Carolina, I think it’s really important that that our voice is heard as well as our other colleagues. We serve patients throughout the state of North Carolina, not just here in Chapel Hill. We have patients from the coast to the mountains.”
Alin’s first order of business on the council pertains to genotyping.
A number of patients that receive lifesaving and life changing blood transfusions for their care can sometimes develop antibodies to the blood transfusion. In more severe cases, patients can develop a delayed hemolytic transfusion reaction. The patient’s immune system recognizes the transfused blood as a foreign invader so it breaks down the transfused blood, while taking out the patient’s healthy red blood cells with it.
When this occurs, hematologists cannot give any more blood to the patient, otherwise the reaction will happen again. To mitigate the occurrence of these type of reactions, hematologists can do genotyping on the patient’s blood to make sure that they have the best possible blood transfusion match for sickle cell patients.
“Genotyping would really help tremendously,” said Alin. “It’s not that expensive. It’s about $900 to do genotyping – and it’s a once in a lifetime test. Somebody’s got to invest in it, so that we can show how this can improve care for this patient population.”
And although Alin has moved up to the big leagues, she will still be enjoying her grassroots efforts in caring for patients hands-on in UNC’s Sickle Cell Program.
“Historically, sickle cell programs have had to struggle to even get basic needs met,” said Alin. “But UNC has really been invested in our program. Dr. Ronald Falk, MD, the Chair of the Department of Medicine, has been incredibly supportive of our program and we’re very appreciative of that.”
Support for the UNC Adult Sickle Cell Program has enabled Dr. Jane Little, MD, the program’s director, to expand the program outside Chapel Hill, according to Alin. They currently offer clinics in both Sanford and Raleigh. They will also have a presence in Wilmington as of October 24th.
– Written by Kendall Daniels