UNC Fibroid Care Clinic
Why Choose UNC?
The University of North Carolina Fibroid Care Clinic is a new treatment model designed to provide up-to-date, comprehensive medical information and care for the treatment of women with uterine fibroids. The Fibroid Care Clinic offers the benefit of close collaboration between gynecology, reproductive endocrinology, and radiology to help coordinate your care. Our team is dedicated to answering your questions and providing you with the highest quality medical care.Procedures
- Myomectomy
- Uterine Artery Embolization (UAE)
- Ultrasound Ablation
- Abdominal Hysterectomy
- Vaginal Hysterectomy
- Laparoscopic or Robot-assisted laparoscopic hysterectomy
What are uterine fibroids?
Uterine fibroids are benign (non-cancerous) tumors that grow in or around the wall of the uterus. Fibroids are the most common non-cancerous tumors in women. Fibroids are also known as myomas or leiomyomas. The size of a fibroid can vary from the size of a pea to larger than a cantaloupe. Fibroids are very responsive to the hormones estrogen and progesterone. For instance, the increase of hormones during pregnancy tends to make fibroids grow, and the decrease in hormones during menopause tends to shrink fibroids. Fibroids vary in size, shape and location and often change the shape of the uterus.
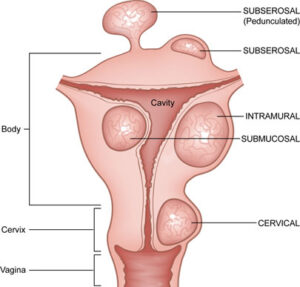
The location of a fibroid can be defined as intramural (within the muscle wall of the uterus), submucosal (underlying the lining of the uterine cavity), or subserosal (just beneath the outer covering layer of the uterus). Sometimes a fibroid grows on a stalk (pedunculated) inside or outside the uterus. Fibroids can occur on any part of the uterus, including the lower part or cervix.
What causes fibroids?
To date, we do not know what causes uterine fibroids. It is thought that each fibroid arises from a single muscle cell in the uterus that experiences a mutation allowing uncontrolled growth. Studies have shown that tumor growth is encouraged by growth signals and hormones such as estrogen and progesterone. During the childbearing years, a woman’s ovaries are producing more estrogen and progesterone, and fibroids tend to grow. After menopause, fibroids tend to shrink.
Current research is looking at links between fibroid development and genetic abnormalities. The exact triggers of these abnormalities are unknown. Most likely, many different factors interact to make fibroids develop and grow.
What are possible signs and symptoms of fibroids?
The most common symptoms include:
- Heavy, prolonged menstrual bleeding
- Severe pain or cramping during menstrual periods
- Pelvic pain or pressure
- Urinary frequency
- Back pain
- Pain during sexual intercourse
- Complications with pregnancy (infertility or miscarriage)
How are fibroids diagnosed?
Fibroids are usually found during a pelvic exam first, or suspected based on symptoms. More definitive ways to diagnose fibroids include the following:
Endometrial biopsy is a test used to look for abnormal gland cells in the lining of the uterus (the endometrium). The biopsy is done in clinic and requires a thin flexible tube that is passed through the cervix to collect a small piece of endometrium. Endometrial biopsy may be helpful in diagnosing causes of abnormal vaginal bleeding. Mild spotting or cramping may occur during or after the biopsy.
How common are fibroids and who is at risk for developing them?
Fibroids are very common and are found in more than one third of women who are child bearing age. They may effect up to 80% of all women, but are less likely to be symptomatic or diagnosed in menopausal women. African-American women are 2-3 times more likely to develop fibroids than Caucasian women. Up to one half of all hysterectomies are performed for symptoms related to fibroids.
Factors that may be associated with fibroids include:
- African-American race (compared to Caucasian)
- Obesity
- Family history of fibroids
- Having never been pregnant (nulliparity)
- Early first period (at less than 10 years of age)
- Birth control pills at an early age (13-16 years of age)
- Heavy alcohol use
What effects do fibroids have on pregnancy?
Most women with fibroids have uncomplicated pregnancies. However, some women may have trouble conceiving or may experience early pregnancy loss, vaginal bleeding, preterm delivery, breech birth (baby emerges buttocks or feet first), or other complications of pregnancy. These complications generally occur in the setting of submucosal fibroids or those fibroids that change the shape of the uterine cavity.
Large fibroids may block the opening of the uterus enough to prevent a baby from delivering head-first, leading to a cesarean delivery. Additionally, during pregnancy estrogen and progesterone hormones increase, which can cause some fibroids to grow faster. Other fibroids shrink or stay the same size. Some fibroids may outgrow their blood supply and degenerate (deteriorate), which can cause pain. Surgery for fibroids is rarely performed during pregnancy.
What effects do fibroids have on fertility?
Couples who are experiencing infertility in the setting of a woman’s fibroids may need additional workup to determine whether there are other causes of infertility besides the fibroid. This evaluation may include:
- Semen analysis
- Blood tests to determine the function of the ovaries and the levels of hormones important to pregnancy
- Tests for blockage of the fallopian tubes (Hysterosalpingogram or HSG)
If all other factors are favorable, removal of some fibroids (myomectomy) can help improve the chances of pregnancy and may be recommended. During a myomectomy, incisions are made in the wall of the uterus. These healed incisions may rupture under the stress of labor, and a cesarean delivery is often recommended for future pregnancies. Additionally, healing of the uterus after a myomectomy may result in scarring between the uterus, ovaries, fallopian tubes, and bowel. This scarring may decrease chances for pregnancy or make future surgery difficult.
Many available treatments used to manage the symptoms of fibroids either delay pregnancy, or are not recommended if a woman desires future pregnancy. Some of these medications or treatments include:
- Leuprolide or Lupron® (a gonadatropin releasing hormone agonist) is a drug used to temporarily shrink fibroids or to control bleeding, but it also prevents pregnancy when using it.
- Endometrial ablation is a technique that uses heat or electricity to destroy the lining of the uterus to reduce the amount of menstrual bleeding. It is not recommended for women who wish to get pregnant.
- Uterine artery embolization (UAE) is not recommended for women who want to become pregnant because the decreased blood supply to the uterus may interfere with normal fetal growth and development. Rarely, UAE may lead to an early menopause.
Could my fibroid be a cancer?
Fibroids are rarely malignant (cancerous). In fact, over 99% of uterine tumors that appear to be fibroids on imaging (ultrasound or MRI) are benign (not cancer). If a fibroid has a worrisome appearance on imaging, the woman may be recommended to have a hysterectomy instead of a myomectomy. Other worrisome findings include a fibroid that grows very rapidly, particularly in a woman who has experienced menopause.