Spiromics Mucin Ancillary
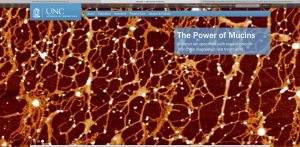
Airway mucus is a dynamic barrier, sequestering particulates, toxins, and pathogens, aiding their removal from the airway by mucociliary transport and/or cough clearance. Airway mucins, particularly MUC5AC and MUC5B, are the major constituent of the normal mucus gel and play an important role in the mucociliary clearance. Over a hundred other proteins contribute mucus structure, of which approximately half are associated with mucins in some fashion, according to recent proteomic studies done in our laboratory. The large secreted mucins, and at least some of associated proteins, contribute to the rheological properties of the mucus. Chronic lung diseases such as COPD are characterized by a hypersecretion of mucus and mucus stasis and accompanied by enhanced susceptibility to infection and inflammation which often exacerbates morbidity and hastens mortality. Beyond this gross level of ‘mucus obstruction’, we know very little. For instance, there are very few studies investigating the mucin/mucus composition in COPD, and those that have been published are based on very small populations of patients. Additionally, we do not know whether COPD mucus pathology results from a simple accumulation of “normal” mucus, or whether the mucus has an abnormal mucin composition and/or properties. Our overall hypothesis, based upon our previous and ongoing studies, is that the molecular composition of the mucus and the concentration and macromolecular organization of its mucins are altered in the COPD environment — both in baseline and during exacerbations. These alterations produce a mucus that has an aberrant rheology, that is poorly transportable by normal ciliary and cough clearance mechanisms. Our specific aims are designed to assess, [i] mucin concentration and the ratio of MUC5AC/MUC5B, [ii] the effects of COPD environment, e.g. proteolysis, on overall mucin polymeric structure, and [iii] the dynamic interplay between mucins and interacting proteins, using samples of mucus obtained through SPIROMICS, (Subpopulations and intermediate outcome measures in COPD observational study) from normal controls, healthy smokers, and COPD patients. We will use induced sputum, and mucus collected by bronchoscopy (BALF) from smoking and non-smoking COPD patients, both at baseline and during exacerbations. The overarching aim is to compare the measured parameters over a large number of normal controls and COPD patients, and within the patient population, to enable the sub-classifications of COPD patients and discovery of biomarkers that underlie the pathogenesis of COPD and its exacerbations. Such knowledge is essential for informed therapeutic intervention aimed at preventing or slowing COPD progression.
Support: R01 HL110906 Kesimer (PI)