
Darren DeWalt Investigates Aspirin Dosing for People with Coronary Heart Disease
Darren DeWalt, MD, MPH, is the site PI for Aspirin Dosing: A Patient-centric Trial Assessing Benefits and Long-Term Effectiveness (ADAPTABLE). In addition to Dr. DeWalt, others in the Department of Medicine that are participating include Joe Rossi in Cardiology and Tim Carey in General Medicine. ADAPTABLE is a novel research study aiming to answer the question “what is the right dose of aspirin for secondary prevention of coronary heart disease: baby aspirin or full dose?” Although some doctors may regularly recommend a baby aspirin or an adult aspirin to their patients, current research evidence does not definitively address whether 81mg or 325mg a day are equivalently safe or efficacious. Given the high prevalence of coronary disease, identifying a superior dose could substantially improve health outcomes.
ADAPTABLE is a randomized controlled trial of 20,000 patients conducted across the country, but it is no regular study. ADAPTABLE is taking advantage of new infrastructure built at UNC and around the country called PCORnet (funded by PCORI). PCORnet has created several networks of health systems using a common data model pulled from EHRs and clinical data warehouses. This common data model can be used to assess clinical outcomes over the course of a study at lower cost than traditional studies that create a completely separate data collection system. For ADAPTABLE, eligible patients do not need any clinical assessments. Other than an online survey, all clinical data is collected through the EHR as part of routine clinical care. This strategy is often called a pragmatic trial that reflects ‘real-world’ medical care in the usual health care setting and using broad inclusion criteria. In addition, recruitment takes place mostly remotely by identifying potentially eligible patients through diagnoses in the data warehouse and inviting patients to participate through letter or MyChart invitations. Lastly, ADAPTABLE represents the new paradigm of patient engaged research by including patient partners at every step of trial design and operations.
Dan Jonas and Arlene Chung are Testing an Integrated Informatics Strategy to Improve Screening and Counseling for Unhealthy Alcohol Use
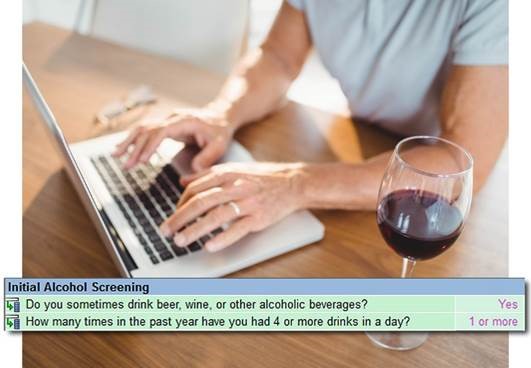 Alcohol is the 3rd leading cause of preventable death in the U.S. Over 20% of primary care patients in the U.S. drink more than the recommended amounts of alcohol. This behavior, defined as risky drinking, is associated with many adverse health outcomes. But national data show that less than a third of patients are asked about alcohol use by their primary care providers, and less than 20% of adults report ever discussing it with a health care professional. Competing priorities, provider discomfort or insufficient training, and lack of needed infrastructure or protocols are key barriers to screening and counseling for risky drinking.
Alcohol is the 3rd leading cause of preventable death in the U.S. Over 20% of primary care patients in the U.S. drink more than the recommended amounts of alcohol. This behavior, defined as risky drinking, is associated with many adverse health outcomes. But national data show that less than a third of patients are asked about alcohol use by their primary care providers, and less than 20% of adults report ever discussing it with a health care professional. Competing priorities, provider discomfort or insufficient training, and lack of needed infrastructure or protocols are key barriers to screening and counseling for risky drinking.
Dan Jonas, MD, MPH, and Arlene Chung, MD, MHA, MMCi are leading a research study to evaluate an integrated informatics strategy designed to overcome these barriers. The intervention uses the patient portal (My UNC Chart) to screen patients for unhealthy alcohol use with validated questionnaires. Through a collaboration with Healthwise, Inc. (a health education content vendor), patients who screen positive are offered coaching through an online, interactive decision aid called “Drinking and Your Health.” An automated summary of patient responses about behavior change and goals will then be securely transmitted to the patient’s primary care provider via the electronic health record system. Electronic screening and online coaching tools could reduce the time required for screening and counseling in the clinic, as well as facilitate and inform provision of appropriate interventions at upcoming appointments. The research team will evaluate the feasibility and acceptability of screening via the patient portal and of using the virtual coaching tool, as well as its effect on intent to change drinking behavior. If successful, this approach could be used for broader population health efforts.
Crystal Wiley Cené leads research to bring social context into patient- and family-centered care
 Crystal Wiley Cené, MD, MPH, FAHA is a health services and health disparities researcher and implementation scientist. The overarching goal of her research, which is interdisciplinary and uses mixed methods, is to bring social context into care through research in community and clinical settings. A major focus of her research is on developing, testing, and implementing clinic and community-based interventions to enhance patient and family engagement in care. She recently published a narrative review article in Medical Care focused on patient and family engagement in the Patient Centered Medical Home. She has a particular interest in understanding how family member involvement in care influences health behaviors and outcomes for adults with and at risk for cardiovascular disease. Dr. Cené recently received funding from the NC TraCS Institute to develop and pilot test, in a randomized clinical trial, a pre-visit prompt list for use with heart failure patient-family member dyads. A prompt list is a structured list of questions or topics related to illness, symptoms, treatment, and support that is developed from interviews with patients and family members. They can facilitate engagement by encouraging patients and family members to ask relevant questions and discuss sensitive topics with health care providers. Dr. Cené is recognized nationally for her expertise in patient- and family-centered care. She served as an expert panelist for the Ambulatory Practice Assessment Project—a collaborative effort between four national organizations (American College of Physicians, Institute for Patient- and Family- Centered Care, National Partnership for Women and Families, and Group Health) designed to develop, implement, and disseminate a validated provider/staff survey assessing the degree of patient and family‐centeredness and engagement in primary care practices.
Crystal Wiley Cené, MD, MPH, FAHA is a health services and health disparities researcher and implementation scientist. The overarching goal of her research, which is interdisciplinary and uses mixed methods, is to bring social context into care through research in community and clinical settings. A major focus of her research is on developing, testing, and implementing clinic and community-based interventions to enhance patient and family engagement in care. She recently published a narrative review article in Medical Care focused on patient and family engagement in the Patient Centered Medical Home. She has a particular interest in understanding how family member involvement in care influences health behaviors and outcomes for adults with and at risk for cardiovascular disease. Dr. Cené recently received funding from the NC TraCS Institute to develop and pilot test, in a randomized clinical trial, a pre-visit prompt list for use with heart failure patient-family member dyads. A prompt list is a structured list of questions or topics related to illness, symptoms, treatment, and support that is developed from interviews with patients and family members. They can facilitate engagement by encouraging patients and family members to ask relevant questions and discuss sensitive topics with health care providers. Dr. Cené is recognized nationally for her expertise in patient- and family-centered care. She served as an expert panelist for the Ambulatory Practice Assessment Project—a collaborative effort between four national organizations (American College of Physicians, Institute for Patient- and Family- Centered Care, National Partnership for Women and Families, and Group Health) designed to develop, implement, and disseminate a validated provider/staff survey assessing the degree of patient and family‐centeredness and engagement in primary care practices.
Dr. Cené also conducts research to examine how the structure (e.g. size, composition) and function (e.g. provision of social support, access to care) of social networks influence health and health care. She has received several pilot awards from the University and from the Women’s Health Initiative Study to collect network data to examine associations between network characteristics and health behaviors and outcomes. She, along with Dr. Brian Southwell from RTI International, will serve as guest editors for a special section in the journal Translational Behavioral Medicine focused on Networks and Health Care Outcomes that will be published in 2018.
Dr. Cené is a co-investigator in the Carolinas Collaborative, a collaborative data research network (CDRN) that includes UNC, Duke, Wake Forest, and Health Systems of South Carolina. Within this project, Dr. Cené leads the health disparities workgroup. The objective of this workgroup is to assess the potential to leverage CDRN electronic health record data to conduct health disparities/health equity research. The workgroup will achieve this objective by assessing the quality of data collection on race, ethnicity, and other disparity indicators, as well as the perspectives of health system administrators and frontline staff at each institution on collection of race, ethnicity, and other sociodemographic data. She is also leading a project for the Disparities Task Force of the Society of General Internal Medicine to compile a database of existing measures of social determinants of health and health care disparities. This database will serve as a tool to facilitate health disparities research. Dr. Cené is also very active nationally with the American Heart Association’s Council on Epidemiology and Prevention. She is currently serving her second two-year term on the Committee to Advance Minority Health, Equity, and Diversity (ADVANCE) and is the Vice-Chair of the committee. She is also a member of the membership and the publications committees. She is a co-author on a forthcoming scientific statement from the American Heart Association Health Literacy in Cardiovascular Disease.
Dan Reuland, Alison Brenner, and Group Pursuing Research to Improve Cancer Screening
 Dr. Dan Reuland’s research program aims to narrow the gap between what evidence suggests health care should do and what happens in the real world. This includes identifying ways to improve health in vulnerable populations, such as those with language, cultural, and literacy barriers. In recent years, his research has focused on making cancer screening more appropriate, patient-centered, and effective through better communication, shared decision making, and patient support. He is currently principal investigator of a multi-site, clinical trial testing the effects of patient decision support and navigation on colorectal cancer screening in community health centers in North Carolina and New Mexico. His current research also includes multi-disciplinary projects aimed at implementing new lung cancer screening guidelines in ways that promote informed and shared decision making and that optimize net benefit (benefits minus harms) at the population level.
Dr. Dan Reuland’s research program aims to narrow the gap between what evidence suggests health care should do and what happens in the real world. This includes identifying ways to improve health in vulnerable populations, such as those with language, cultural, and literacy barriers. In recent years, his research has focused on making cancer screening more appropriate, patient-centered, and effective through better communication, shared decision making, and patient support. He is currently principal investigator of a multi-site, clinical trial testing the effects of patient decision support and navigation on colorectal cancer screening in community health centers in North Carolina and New Mexico. His current research also includes multi-disciplinary projects aimed at implementing new lung cancer screening guidelines in ways that promote informed and shared decision making and that optimize net benefit (benefits minus harms) at the population level.
Dr. Reuland was recently tapped to lead the Carolina Cancer Screening Initiative (CCSI), a new UNC Lineberger program supported by the University Cancer Research Fund. In this role he works closely with Dr. Alison Brenner, Associate Program Director, and other CCSI core members to leverage UNC’s expertise in development, testing, and implementation of data-driven interventions to improve cancer screening in practice. An initial focus of CCSI will be improving colorectal cancer screening in North Carolina, particularly in the northeastern part of the state where there is evidence of high colorectal cancer mortality. To tackle this issue, a number of simultaneous projects are underway including 1) geospatial analysis and modeling of data from UNC’s Integrated Cancer Information and Surveillance System to describe patterns and drivers of colorectal cancer and estimate the potential effects of screening interventions; 2) systematic review and synthesis of emerging evidence regarding colorectal cancer screening interventions; 3) trials of practice and community-based interventions to improve screening; and 4) stakeholder engagement at local, state, and national levels in order to understand the contexts and challenges related to screening and to inform partnerships, policies, and resource allocation for screening implementation.