Treatment Options
Choose from nearly a dozen treatment options.
More than half of cancer patients receive radiation therapy as part of their cancer treatment. Radiotherapy involves the precise medical application of ionizing radiation in order to destroy cancerous tumors.
Why are there so many different treatment options?
It’s confusing!
Each type of radiotherapy has its own indications, advantages and disadvantages. Your UNC radiation oncologist will help you choose the treatment that best suits your particular needs.
Generally speaking, there are three types of radiotherapy treatment:
- External beam radiotherapy: The radiation beam enters the patient through the skin and is focused on the tumor in order to kill it.
- Brachytherapy: Small radioactive “seeds” or wires are inserted into the patient’s body inside or next to the tumor in order to treat it.
- Special procedures: highly specialized equipment is sometimes required for ultra-precise control, for sterile conditions during surgery, or to treat a larger amount of tissue than more traditional external beam or brachytherapy techniques can handle.
External Beam Radiotherapy
UNC offers state of the art external beam radiotherapy treatment options, including 3-dimensional conformal radiation therapy, intensity-modulated radiation therapy, image guided radiation therapy and tomotherapy.
 Three-Dimensional Conformal Radiation Therapy (3D-CRT)
Three-Dimensional Conformal Radiation Therapy (3D-CRT)
This is the most common technique used to treat cancers in many parts of the body. A set of CT images is used to identify both the tumor and the critical normal tissue structures that need to be avoided. Then, radiation beams of varying shapes are designed to enter the patient from multiple angles, and “hit” the tumor while avoiding nearby healthy tissues. Patients usually receive their treatment once per weekday for a total of two to seven weeks.
Intensity-Modulated Radiation Therapy (IMRT)
IMRT is a specialized form of 3D-CRT treatment in which not only the shapes of the radiation beams are varied, but their “strengths” or intensities as well. This further guarantees that the tumor receives the maximum amount of radiation, while the surrounding normal tissues receive the least possible.
 Image Guided Radiation Therapy (IGRT)
Image Guided Radiation Therapy (IGRT)
A new, cutting-edge technique that combines X-ray imaging and radiation therapy, and allows daily tracking of changes in both the location and shape of the tumor and healthy surrounding tissues during the course of treatment. IGRT promises to further improve the accuracy of radiation therapy.
Tomotherapy
A sophisticated type of external beam radiation therapy in which the radiation is delivered to the tumor slice- by-slice across its entire volume, rather than irradiating the whole volume at once, improving tumor targeting while minimizing the irradiation of surrounding normal tissues.
by-slice across its entire volume, rather than irradiating the whole volume at once, improving tumor targeting while minimizing the irradiation of surrounding normal tissues.
Brachytherapy
UNC offers several options for delivery of radiation through the use of radioactive sources. These include:
High Dose Rate Brachytherapy
Brachytherapy involves the use of radioactive sources that are either implanted into the tumor (interstitial brachytherapy) or placed near it, generally in a body cavity (intracavitary brachytherapy). For example, uterine and cervical cancers are often treated with intracavitary brachytherapy, and prostate cancers (see below) can be treated using interstitial brachytherapy. Often, HDR is combined with one of the types of external beam radiotherapy described above.
Prostate Seed Implant
This interstitial brachytherapy technique is only used to treat prostate cancer. Radioactive  seeds (Iodine-125 or Palladium-103 sources are commonly used) are surgically implanted into the prostate in such a way that the entire tumor is irradiated to a high total dose.
seeds (Iodine-125 or Palladium-103 sources are commonly used) are surgically implanted into the prostate in such a way that the entire tumor is irradiated to a high total dose.
The implant is generally performed as an outpatient procedure. The seeds remain in the prostate permanently, however the radioactivity itself decays away in a matter of a month or two.
Eye Plaques
Certain tumors of the eye (choroidal melanomas, for example) are often treated with the temporary placement of radioactive sources (Iodine-125) on the back of the eye, immediately next to the tumor. These radioactive “plaques” are left in place for four days after which they are removed.
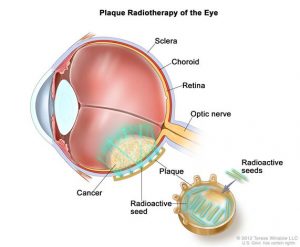
For properly selected patients this treatment, which involves two small surgical procedures, is as effective in controlling the tumor as removing the eye altogether, a major surgical procedure.
Special Procedures
 CyberKnife
CyberKnife
The CyberKnife is a robotically-controlled linear accelerator that precisely and accurately tracks the tumor during treatment (for example, to monitor bodily motion due to breathing) and makes on-the-fly corrections to keep the beam tightly focused on the tumor.
Intraoperative Radiotherapy (IORT)
 IORT is a specialized radiotherapy treatment procedure that is performed in the operating room.
IORT is a specialized radiotherapy treatment procedure that is performed in the operating room.
In general, IORT delivers localized single-dose radiation treatment directly through the surgical incision to the tissue region surrounding where the tumor has been surgically removed (i.e., the “tumor bed”). IORT allows radiation oncologists to deliver a high dose of radiation to the target volume while effectively minimizing the irradiation of the nearby sensitive normal structures. The single IORT treatment can increase the total dose of radiation to a tumor or treatment target (in the hopes of improving cure rates), and at the same time reduces the need for daily outpatient radiation therapy lasting several weeks.
UNC was only the fourth medical center in the United States to use a mobile, electron-based radiation therapy system for IORT. The Mobetron is a self-shielded electron linear accelerator that can be wheeled into the operating room to deliver concentrated beams of electrons directly to the tumor site during surgery. The accelerator was developed by Intraop Medical Corporation of Sunnyvale, CA.
The primary use of IORT at UNC has been for the treatment of patients with locally advanced rectal and colon tumors, retroperitoneal soft tissue sarcomas, and early stage breast cancers, as well as for some patients with head and neck and gynecological malignancies.
Total Body Irradiation (TBI)
TBI is often used to prepare a patient for bone marrow or blood stem cell transplants. The aim of this therapy is to prevent the rejection of the transplanted cells and to kill residual tumor cells throughout the body. The radiation treatment is delivered to the whole body and may take thirty minutes per side, front and back. Treatments may be repeated one to three times a day for a total of two to four days.