Handing Off the Older Patients: Improved Documentation of Geriatrics Assessment in Transitions of Care – Maureen C. Dale, MD
Older adults, particularly frail elders, are at an increased risk for poor health outcomes and avoidable re-hospitalization during transitions of care. Nearly one of five older adults are re-hospitalized within 30 days of

hospital discharge, and studies have noted that up to 20% of older patients on medicine services have adverse events after discharge, many of which are preventable.
Maureen Dale, MD, and Benjamin Blomberg, MD, along with Geriatric Medicine Fellows Adam Moskowitz, MD, Sheri Mouw, MD, and Bianca Yoo, MD, have developed a project aimed at reducing 30-day readmissions on the inpatient geriatric service by improving communication between the inpatient team and post-acute care providers.
To do this, they trained residents to use a structured discharge summary template that incorporates documentation of functional assessment, cognitive assessment, and advanced care planning, as well as pharmacy-led discharge medication reconciliation, all of which have been shown to impact readmissions in transitional care interventions. In addition, they have performed root cause analyses on each 30-day readmission during the intervention period, including reaching out to multiple post-acute care providers for feedback on the discharge summary template as well as specific readmissions. Data analysis is ongoing for this year’s project.
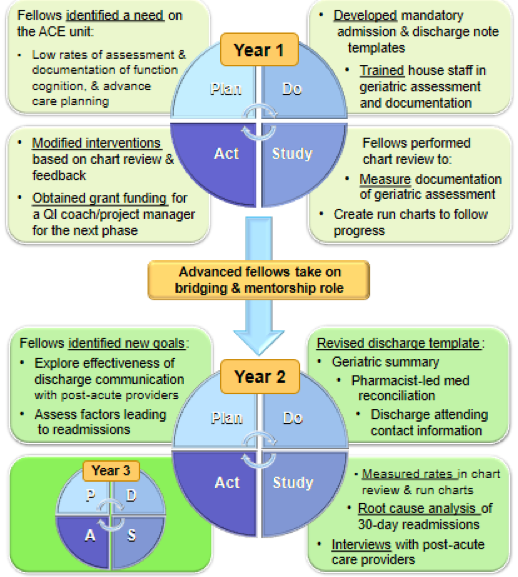
This project, supported by the IHQI Improvement Scholars Program, is year two of the new Geriatric Medicine Fellowship’s continuous quality improvement curriculum. This curriculum has allowed teams of Geriatric Medicine fellows to complete meaningful QI projects within their one year fellowship and pass the project to the next class of fellows, ensuring sustainability and continued improvement.
Fellows in the 2016-2017 academic year implemented a discharge summary template that incorporated a geriatric assessment for the inpatient geriatric service, and their work was recently published in The Journal of the American Geriatrics Society.
A Pilot Study Examining the Feasibility of Using a Pharmacogenetic Assay in Mechanically Ventilated Adults in the Medical ICU – Adrian Austin, MD
Delirium, a form of acute brain dysfunction defined by inattention and a fluctuating course, is a devastating entity that leads to negative patient outcomes. It is seen among critically ill adults: approximately 70% of mechanically ventilated ICU patients are diagnosed with delirium. Each day with delirium in the ICU increases a patient’s relative risk of in-hospital death by an estimated 10%, and continues to increase the risk of death even one year after hospitalization. Delirium also increases patient morbidity and is associated with increases in hospital length of stay, increased functional decline, and long term cognitive impairment. At this time, no pharmacological agents are proven to effectively prevent or treat delirium. Current management strategies for this devastating condition focus on prevention and mitigation of its effects.
Numerous identified risk factors predispose patients to delirium. Non-modifiable, predisposing determinants include mechanical ventilation while potentially modifiable determinants for the critically ill population include sedating medications, metabolic impairments, sepsis, and sleep disturbances. Most mechanically ventilated patients receive sedating medications known to cause delirium, such as opiates (e.g., morphine and fentanyl), as part of routine care. Genetic variation in drug metabolism of drugs used for analgesosedation may explain the variation seen in the efficacy and side effects of these medications including incidence of delirium.
Pharmacogenomics is the study of genetic variation in the pharmacokinetics and pharmacodynamics of medications. Recent scientific advances in pharmacogenomics provide an avenue to investigate the impact of metabolic variations on delirium in the critically ill. Prior research has examined the genetic basis for inter-individual differences in response to opioids. As a result, the FDA has approved pharmacogenetic information in labeling for some opioids, but no current guidance exists for fentanyl and morphine. A number of genes, including the mu opioid receptor gene, OPRM1, the catchol-O-methyl transferase (COMT) gene, and the cytochrome P450 3A4 (CYP3A4) gene have been identified as important in morphine and fentanyl’s drug efficacy and adverse effect profiles, but the effect of variation of these genes in the critically ill adult population on response to these drugs has not been explored.
Researchers hypothesize that the pharmacogenomics of sedating medications accounts for some of the variability in delirium occurrence observed in mechanically ventilated patients. Delineating the impact of this variability on the incidence and duration of delirium will pave the way for precision medicine in the ICU. The purpose of our pilot feasibility is to demonstrate that pharmacogenomic data can be safely and reliably obtained and analyzed prior to embarking on a larger study. This study is currently being conducted in the Medical ICU at UNC. Researchers anticipate completing enrollment in the pilot phase this fall.
Development and Validation of a Remote, Tablet-based Delirium Assessment Tool – Adrian Austin, MD
Between 12% and 30% of elderly inpatients will suffer from delirium during their hospitalization, and it is associated with at least a two-fold increase in risk of death at one year after hospitalization. In addition to its impact on mortality, it greatly increases patient morbidity. It is associated with increased hospital length of stay, increased functional decline, and long term cognitive impairment. Between 9% and 15% of elderly medical inpatients suffer from delirium that persists to at least time of discharge. Prior research found that patients who were discharged to a post-acute care setting with active delirium had an increased risk of 30-day re-hospitalization, six-month mortality, and one-year mortality. Despite the known negative effects of delirium in the post-acute care population, little is known about the impact of persistent delirium on day-to-day function immediately after discharge to the home setting. The current ability to feasibly evaluate the impact of delirium immediately after discharge is limited by the lack of a quick, reliable delirium assessment that can be performed in the home setting after discharge.
There are no current bio-markers or laboratory-based diagnostic tests for delirium necessitating a clinical diagnosis. Current clinical diagnosis tests require a face-to-face encounter, which limits the ability to feasibly perform frequent delirium assessments in the post-discharge setting. The most commonly used delirium assessment is the Confusion Assessment Method (CAM). It consists of a series of questions and clinical observations, primarily regarding level of consciousness and fluctuations in attentiveness. Given that this screening tool requires observations, the ability to perform the CAM remotely is currently limited. One prior study examined in-home delirium assessments via telephone and found good sensitivity (100%) and specificity (94%). However, this study was limited by its positive predictive value of 50% and its small sample size (n=41). Further, the assessment which consisted of the Delirium Symptom Interview and a version of the Mini-Mental Status Exam takes over fifteen minutes to perform, which has severely limited its practical usage.
Over the past few years, devices that support videoconferencing such as smart phones, have become commonplace. As of 2015, over 50% of all American adults had smartphones. Concurrently, interest in teleneuropsychology and remote diagnoses of cognitive disorders has grown. Remote cognitive assessments have recently been demonstrated to be valid, reliable, and acceptable to patients. Remote assessments have utilized a wide range of technology ranging from traditional videoconferencing to smartphone assessments. We hypothesize that currently available videoconferencing capabilities can be easily and quickly utilized to perform reliable delirium assessments in elderly adults in the home setting. This project will develop and validate a tablet-based videoconferencing-based delirium assessment tool based on the CAM (Video-CAM).
This tool will prove invaluable for future researchers and clinicians as it will provide the ability to perform quick, valid, low-cost delirium assessments in the home setting. Information gained from usage of this tool will allow researchers to define the impact of persistent delirium on those patients discharged to the home setting. Further, it will provide a method for clinicians to perform quick, remote delirium assessments of their patients. This could be particularly useful, for example, if a patient’s caregiver has concerns about a change in mental status and wishes to avoid a potentially unnecessary clinic or emergency department visit. We are currently assessing user acceptability of a tablet based CAM in a geriatric population with plans to validate this tool once it is further refined.
Palliative and Oncology Collaborative Care for Advanced Cancer – Laura C. Hanson, MD, MPH
Early access to specialty Palliative Care improves outcomes at a lower cost for patients with Stage IV cancer. Patients with advanced cancer who receive concurrent early specialty Palliative Care and Oncology care, report better quality of life, less pain and depression, reduced use of late-life chemotherapy, earlier hospice referral, and are more likely to discuss goals of care. However, medical oncologists lack the time and sufficient skills to consistently deliver palliative care, and concurrent specialty Palliative Care is not feasible for all patients due to limited workforce. Because of these barriers, concurrent care models of early Palliative Care have not been disseminated even in well-resourced NCI Comprehensive Cancer Centers. Delays in addressing palliative care needs and goals of care discussions further limit access.
Collaborative care is a model of outpatient care for patients with complex illness that was originally developed to better manage patients with depression. In the collaborative care approach, outpatient care is made more effective, by systematically tracking high-risk patients and facilitating collaborative care between primary physicians and specialists. It improves outcomes both in solo efforts by a primary physician to manage complex illness, and referral to multiple specialists who may see the patient in parallel with a primary physician but with little care coordination.
With funding from a Tier 2 Clinical/Translational Award from UNC Lineberger Comprehensive Cancer Center, Laura Hanson, MD, MPH and the project team have developed, and are currently implementing and testing, a collaborative palliative care model for patients with Stage IV cancer. The Palliative and Oncology Collaborative Care for Advanced Cancer model offers an innovative approach to support continuity of care between inpatient and outpatient providers and facilitate efficient and targeted use of specialty Palliative Care.
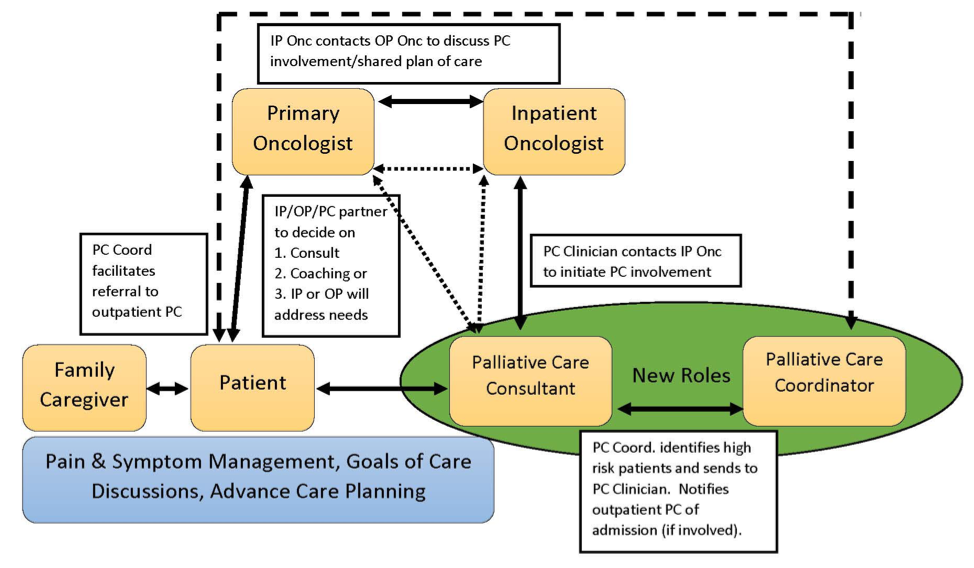
In the Palliative and Oncology Collaborative Care for Advanced Cancer model, the outpatient Medical Oncology and Primary Care physicians are both identified as providing continuity of care, basic management of pain and symptoms, psychiatric distress, communication of prognosis and treatment options, and discussions of goals of care. Specialists in Palliative Care will provide inpatient and outpatient consultation, triggered by complex pain and symptom needs, severe psychiatric distress, or challenging goals of care communication. A nurse navigator with oncology and palliative care training will act as Palliative Care Coordinator, and the Study Coordinator will collect data and maintain the tracking database. (Figure 1)
Phase I of the project involved the creation of a high-risk oncology population tracking database, collection of observational data on the quality of palliative care received during usual care for patients with Stage IV cancer and at least one acute illness admission to E2, and the development of the collaborative palliative care model for patients with Stage IV cancer.
Phase II of the project is comprised of 4 main components: 1) primary palliative care skills training for Medical Oncology; 2) continued systematic tracking and data collection of high risk Stage IV cancer patients; 3) palliative care needs assessment and care plans created by specialty Palliative Care providers and shared with the outpatient Medical Oncologist and Primary Care physician when applicable; and 4) outpatient care coordination to meet ongoing palliative care needs.
Project team members include Laura C. Hanson, MD, MPH, Katherine Aragon, MD, Frances A. Collichio, MD, Darren DeWalt, MD, MPH, Jenny Hanspal, BSN, ONC, Kyle Lavin, MD, MPH, Jennifer McEntee, MD, MPH, Matthew Milowsky, MD, Donald Rosenstein, MD, Gary Winzelberg, MD, MPH, and William Wood, MD.
The Carolina Geriatric Workforce Enhancement Program (CGWEP) – Jan Busby-Whitehead, MD

The UNC Center for Aging and Health’s Carolina Geriatric Workforce Enhancement Program (CGWEP) is a four-year $3,457,045 grant-funded research and training program whose goals are to:
- integrate geriatrics into rural and underserved primary care settings and leverage interprofessional geriatrics teams to improve health outcomes in older populations;
- collaborate with community partners to increase family and caregiver access to geriatric training, education, and resources;
- provide education and training in Alzheimer’s disease and related dementias; and
- support primary care providers in opioids-related outreach and education.
Providers and Partners Served
CGWEP initiatives from 2015 through 2018 continue to expand training, serving almost 20,000 healthcare providers and 31 rural and underserved partner sites — nearly triple the 12 sites originally proposed. North Carolina’s nine Area Health Education Center (AHEC) partners developed and delivered 209 geriatric continuing education courses, reaching all 100 NC counties with courses on advanced care planning, falls prevention, dementia care, diabetes, opioid management, and more.
Sites reported increased frequency of geriatric assessments and interventions and more prevalent use of interprofessional (IPE) geriatrics-trained teams. Participating primary care providers selected an area of “practice change” geriatrics to focus on. They primarily chose to implement falls risk screening or advance care planning (ACP) programs. After training, falls risk screening rates and interventions increased significantly, and care providers made a solid start in charting ACP in medical records.
Interprofessional Training
The CGWEP allows the Center for Aging and Health to supplement our Chapel Hill-based Geriatric Fellowship Program with Interprofessional Geriatric Fellowship training. Our nine IPE Fellows (over an original goal of five) include three dentists, three nurses, and three physicians who delivered geriatrics training for participating clinics’ practice change projects. IPE Fellows led ACP training for clinic staff at rural family practice clinics in Roxboro and Conetoe. In 2017, IPE Geriatric Fellows produced a toolkit on unexplained weight loss, along with role-play-based ACP training. The weight loss toolkit was published on MedEdPORTAL for easy access by all.
Providing interprofessional graduate school training in the care of the older adult patient is a CGWEP core component. In 2018, our IPE Geriatrics pre-professional program expanded from 6 to 10 disciplines and trained 687 IPE health profession students.
ADRD in American Indians / Opioid Addiction in Older Adults
Through the original grant, along with supplemental funding in 2015 for Alzheimer’s and related dementias (ADRD), CGWEP and our AHEC partners continue a strong emphasis on ADRD training for all levels of health professionals. In total, the CGWEP developed and implemented 31 continuing education events to provide ADRD education and training.
A 2017 supplemental grant enables our partnership with the North Carolina American Indian Health Board, East Carolina University, and Wake Forest University to produce culturally appropriate content for in-state tribes, who have higher rates of diabetes and other risk factors for dementia. Rising rates of dementia and a shortage of culturally competent paid caregivers highlight the strong need for increased outreach. Recent CGWEP-funded resources for this population include a best practices list for clinics and caregivers serving American Indian Elders, and a documentary on the impact of dementia and Alzheimer’s in American Indian communities, “Still Here.”
Finally, a July 2018 supplemental grant on Opioid Addiction in Older Adults allowed three Area Health Education Centers to present continuing education events on opioids, reaching 500 health care providers across the state.
Geriatrics Workforce Enhancement Program (GWEP) – Coordinating Center: Interprofessional training in geriatrics to promote high quality healthcare services to American Indians and Alaska Natives (AI/AN) – Cristine (Clarke) Henage, MPS, EdD
Summary
The UNC Center for Aging and Health was awarded a GWEP Coordinating Center Collaborative extension grant in an effort to provide interprofessional training in geriatrics to

promote high quality healthcare services to American Indians and Alaska Natives (AI/AN). Through a partnership with GWEPS in Alaska, Arizona, California and Wyoming and other regional agencies, the AI/AN Coordinating Center has the continued potential to serve 149 recognized federal tribes with a population of over 503,345 rural and underserved older adults. The five AI/AN Coordinating Center GWEPS collaborated at a distance; comparing research, promoting strategies to enhance interprofessional practice, sharing resources, sourcing new grant opportunities and bringing new interested partners to the collaboration.
Purpose & focus
The AI/AN CoordinatingCenter (AI/AN Collaborative) advanced knowledge, best practices and innovations for engaging AI/AN elders and their families. They created and deployed culturally appropriate training to healthcare practitioners at primary care clinics utilized by Native peoples will ultimately improve health outcomes. AI/AN’s health is affected by social determinants such as poverty, unemployment, inadequate formal education, etc. Higher rates of diabetes are found across all tribes with higher rates of specific disproportionately illnesses being found regionally for example, dementia mortality rates are 50% higher in North Carolina. This collaboration provided an opportunity to learn about and evaluate existing resources, and share lessons learnedfrom one GWEP to another.
GWEP Organizations
Each AI/AN Coordinating Center GWEP was engaged in providing continuing education and practice change projects in primary care clinics focusing on the special needs of AI/AN peoples. Some of the GWEPS designed special projects for their service area and some integrated principles of care respectful of AI/AN culture into their activities. Community based partners ranged from think tanks interested in policy around Native American issues in North Carolina to frontline providers in rural Alaska to long term care facilities in Arizona. One example of the kind of best practice that could be replicated as a result of this collaboration is the NUKA system of care developed by Southcentral Foundation in Alaska. This system emphasizes customer ownership, relationship based care and whole system transformation. Similarly, UCLA works in partnership with the Veteran’s Administration (VA) Geriatric Scholars Program making VA Indian Health Service Rural Interprofessional Team Training (IHS-RITT) available to Indian Health Service clinics for all federally recognized Tribes. The VA RITT and VA IHS-RITT programs have been delivered to >100 rural clinics.
The AI/AN Collaborative met in person twice during 2017. The established CGWEPs also participated in several planning conferences and telecommunication sessions. The first meeting was held in July in San Francisco following the International Association for Gerontology and Geriatrics meeting. The second meeting was held on October 27, 2017 in Tucson Arizona. In addition to the five GWEPs, four experts on AI/AN health and interprofessional training, representing the Banner Alzheimer’s Institute, the National Indian Council on Aging, the Indian Health Service and the Veterans Administration, attended the October meeting in Tucson. The group reviewed the literature on health issues for older AI/AN peoples, explored models of IPE care for these populations, and shared educational products.
Objectives & Outcomes
The AI/AN Collaborative reviewed and discussed existing best and promising practices used by GWEPs and our consultant experts in healthcare and education to engage American Indian/Alaska Native elders and their families, and improve their care in a culturally relevant manner. This resulted in improved knowledge, access, and intent to utilize educational products and strategies that are culturally appropriate beyond each individual GWEP’s local area. The AI/AN Collaborative developed a list of 48 best practices that was reviewed by the experts in the Collaborative.
The AI/AN Collaborative examine effective strategies for training American Indian/Alaska Native-serving primary care providers in culturally informed care of elders, such as the VA Indian Health Service Rural Interdisciplinary Team Training (VA IHS RITT), NUKA System of Care and other models. They increased knowledge and intent to use culturally relevant and respectful tools and approaches for preparing primary care providers in meeting the health care needs of American Indian/Alaska Native elders. Two models of culturally appropriate care were presented and discussed at the meetings, the NUKA System of Care and the Veteran’s Administration IHS Rural Interdisciplinary Team Training model. Two AI/AN Collaborative members currently use models, Alaska and UCLA and the others expressed interest in using them in addition to contacts external to the AI/AN Collaborative GWEPs who expressed interest in exploring the models and receiving additional training.
The AI/AN Collaborative evaluated new and innovative projects targeting American Indian/Alaska Native populations that were currently are being piloted by GWEPs. They evaluated how innovative projects were adapted, implemented, and outcomes evaluated to improve the services of the local population, to build generalizable evidence for these innovations. The AI/AN Collaborative is exploring the feasibility of being included into a national database and listserv of professionals who work on elder and/or palliative care issues in Indian Country being developed by the Indian Health Service.
Continued Collaboration
These five GWEPs and their Native American consultants continue to collaborate at a distance through comparing research, promoting strategies to enhance interprofessional practice, sharing resources, sourcing new grant opportunities and bringing new interested partners to the collaboration. The AI/AN Collaborative also continues to share information more widely with other interested GWEPs (Montana and Utah) who are not part of the Collaborative and who did not participate in our face-to-face meetings. The Health Resources and Services Administration has recognized the value of this work and will fund an expansion of the project in 2018 adding Hawaii to the Collaborative.