UNC School of Medicine researchers led by Hyejung Won, PhD, Assistant Professor of Genetics, used a new kind of computational tool to parse the complicated genetics that put some people at higher risk of becoming addicted to alcohol, cigarettes, and likely other substances of abuse.
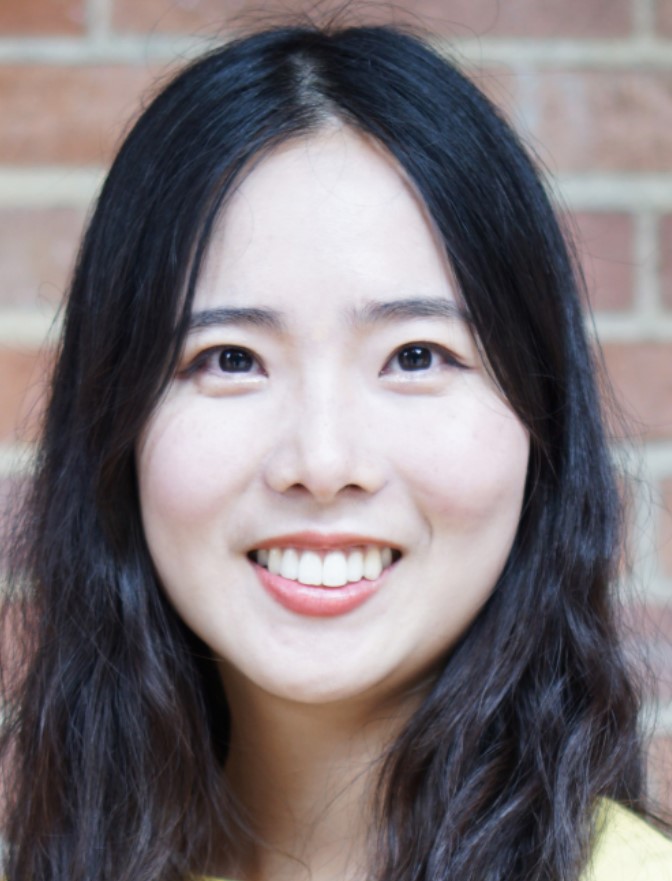
CHAPEL HILL, NC – Have you ever wondered why one person can smoke cigarettes for a year and easily quit, while another person will become addicted for life? Why can’t some people help themselves from abusing alcohol and others can take it or leave it? One reason is a person’s genetic proclivity to abuse substances. UNC School of Medicine researchers led by Hyejung Won, PhD, are beginning to understand these underlying genetic differences. The more they learn, the better chance they will be able to create therapies to help the millions of people who struggle with addiction.
Won, assistant professor of genetics and member of the UNC Neuroscience Center, and colleagues identified genes linked to cigarette smoking and drinking. The researchers found that these genes are over-represented in certain kinds of neurons – brain cells that trigger other cells to send chemical signals throughout the brain.
The researchers, who published their work in the journal Molecular Psychiatry, also found that the genes underlying cigarette smoking were linked to the perception of pain and response to food, as well as the abuse of other drugs, such as cocaine. Other genes associated with alcohol use were linked to stress and learning, as well as abuse of other drugs, such as morphine.
Given the lack of current treatment options for substance use disorder, the researchers also conducted analyses of a publicly available drug database to identify potential new treatments for substance abuse.
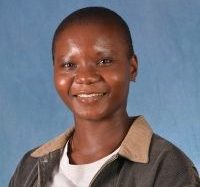
“We found that antipsychotics and other mood stabilizers could potentially provide therapeutic relief for individuals struggling with substance abuse,” said first author Nancy Sey, a graduate student in the Won lab. “And we’re confident our research provides a good foundation for research focused on creating better treatments to address drug dependency.”
Parsing the Genome
Long-term substance use and substance use disorders have been linked to many common diseases and conditions, such as lung cancer, liver disease, and mental illnesses. Yet, few treatment options are available, largely due to gaps in our understanding of the biological processes involved.
“We know from twin studies that genetics may account for why some people use and abuse substances, aside from environmental factors, such as family issues or personal trauma,” Won said. “Genetic studies such as genome-wide association studies (GWAS) provide a way to identify genes associated with complex human traits, such as nicotine addiction or drinking heavily.”
Through GWAS, Won added, researchers can identify regions in the genome that play roles in particular traits, compared to individuals who do not exhibit the trait. Yet, genome-wide studies cannot tell us much about how genes in those regions affect a trait. That’s because these regions are often in “non-coding” regions of the genome.
“Non-coding” refers to the fact that the genes in these regions do not translate – or code – their genetic information directly into the creation of proteins, which then perform a known biological function. Therefore, what actually happens biologically in these “non-coding” regions remains mostly unknown.
“We wanted to learn what’s happening in these regions,” Won said. “So we developed Hi-C coupled MAGMA (H-MAGMA), a computational tool to help us make more sense of what we’re seeing in genome-wide studies.”
In a previous publication, Won’s lab showed how applying H-MAGMA to brain disorders identifies their associated genes and described their underlying biology. And for this current paper, her lab expanded the tool to cigarette smoking and drinking.
They developed H-MAGMA frameworks from dopaminergic neurons and cortical neurons – brain cell types that researchers have long implicated in substance use. Focusing on those two cell types, Won’s team – led by Sey, an HHMI Gilliam Fellow – applied H-MAGMA to GWAS findings related to heaviness of smoking, nicotine dependence, problematic alcohol use, and heaviness of drinking to identify genes associated with each trait.
Genes associated with alcohol use and cigarette smoking were also associated with other types of substances, such as morphine and cocaine. While the opioid crisis has caused a detrimental social burden, well-powered GWAS on cocaine and opioid use are not currently available. Won’s team, therefore, sought to determine whether the genes associated with alcohol use and cigarette smoking can reveal genetics underlying general addiction behavior, genetic findings that could be extended to other substances of abuse.
“Our analyses showed that expression of genes shared between cigarette smoking and alcohol use traits can be altered by other types of substances such as cocaine,” Won said. “By characterizing the biological function of these genes, we will be able to identify the biological mechanisms underlying addiction, which could be generalized to various forms of substance use disorder.”
In addition to the various types of excitatory neurons, Won’s team also identified additional cell types, including cortical glutamatergic, midbrain dopaminergic, GABAergic, and serotonergic neurons that are associated with the risk genes.
With these findings in hand, it is now possible for the UNC researchers and others to investigate molecules that make addiction much less likely.
This research was supported through grants from the National Institute on Drug Abuse (R21DA051921, U01DA048279); the National Institute of Mental Health (R00MH113823, DP2MH122403); the NARSAD Young Investigator Award from the Brain and Behavior Research Foundation; the National Science Foundation Graduate Research Fellowship Program (DGE-1650116); the University of North Carolina at Chapel Hill; the Howard Hughes Medical Institute’s James H. Gilliam Fellowship for Advanced Study Program; and the National Institute of General Medical Sciences (5T32GM067553).
The article originally appeared in the UNC Health Newsroom.
