Complex Care Committee Develops Individualized Care Plans – Beth Ann Brubaker, MD
Individualized care plans (ICPs) have been created for patients who are high utilizers of inpatient resources. In some cases this high utilization has been due to fractioned/inefficient medical care and in other cases due to social/addiction issues. Most of these patients have chronic medical illnesses, chronic pain issues, and may lack understanding of appropriate utilization of resources. For some patients, it is clear that opioid dependence and addiction issues drive the majority of the frequent hospitalizations.
Care for these patients is often flawed and ineffective, and providing this type of medical care can be demoralizing for providers and contribute to physician burnout. Additionally, patients who are provided dramatically different management for the same issue from one hospitalization to the next become frustrated and are at high risk of readmission, substance abuse (including overdoses and IVDU related infections), medication errors, and distrust of the medical system.
Hospitalists are in a unique position to address the issues that contribute to high utilization of the medical system. As a team, they are already familiar with many of these patients, their medical issues, and their social situations. This gives them a strategic advantage, in attempting to help patients overcome destructive, unhealthful, unproductive habits. Hospitalists can have genuine conversations with patients about the actual medical and psychosocial issues. In many instances, these conversations have revealed more focused or detailed problem lists which can then be addressed in the care plan. Sometimes the patients are open to this and sometimes not, but this focus on the real issues at play is the basis of the ICP creation.
The ICPs seek to identify the real issues driving frequent hospitalizations, and provide the most safe, effective, and high quality care for these patients. This helps providers to be transparent and consistent in communication and approach to management, and allows patients to know what to expect when they come into the hospital. Hopefully, this also improves therapeutic relationships with patients, and reduces burnout in providers.
Overutilization of hospital resources by this population is not a challenge that is specific to UNC. Many of these patients also frequent Duke, WakeMed, Rex, and other local community hospitals, and this is yet another component of the disjointed and variable care that they receive. Duke and WakeMed have similar complex care committees working in parallel, and UNC has coordinated efforts with these institutions in order to merge patient care into a single, more directed and rational pathway.
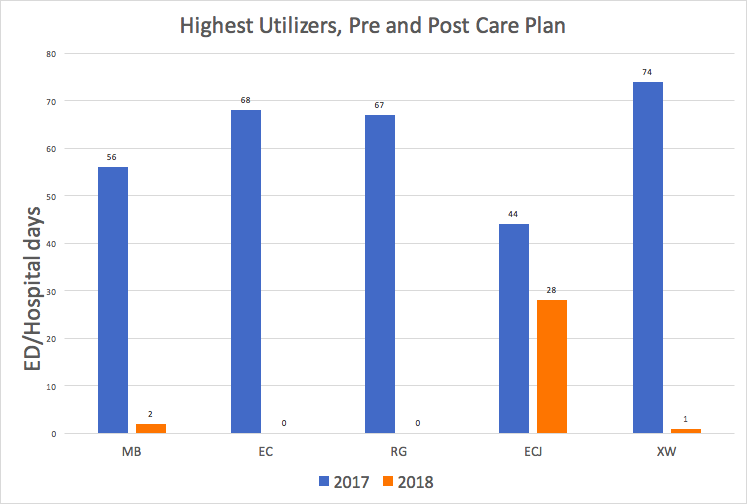
The graph above compares five of the highest utilizing patients in 2017 and 2018. Corresponding values for each patient, pre and post plan, showed a dramatic reduction in ED and hospital days (including partial days). (Care Plans were in place 12/20/2017)
UNC Medical Center’s Complex Care Committee was started by Beth Ann Brubaker, MD, Andy Donohoe, MD, and Kelly Stepanek, NP. To date, nearly 50 ICPs have been created.
Using EMR technology to improve VTE risk assessment and prophylaxis – Jamison Chang, MD, MS
Venous thromboembolism (VTE) remains an important and preventable cause of morbidity and mortality in the United States. It is estimated that 600,000 people per year in the US are diagnosed with VTE and close to 100,000 die as a result (1). One underappreciated fact is that over half of VTEs occur while patients are hospitalized despite the availability of effective prophylaxis (2). In addition to the morbidity and mortality associated with VTE, there are also significant costs associated with these events in terms of penalties or withheld payments to hospitals. Previous efforts to reduce hospital acquired VTE (HA-VTE) at UNC have used retrospective chart review to try to identify the root causes of HA-VTE at UNC, leading to inconsistent effects.
Jamison Chang, MD, and colleagues have developed a system that identifies HA-VTE in near real time so that the quality and safety teams at UNC are able to better identify the causes underlying these events and intervene in a timely fashion. A seed grant from the Institute for Health Quality Improvement (IHQI) at UNC has allowed his team to begin to tackle this problem using various forms of health information technology, including the novel natural language processing engine, EMERSE, that is being deployed across the UNC healthcare system. This program is able to read free text documents in EPIC including providers notes and radiology reports and accurately identify HA-VTE at UNC.
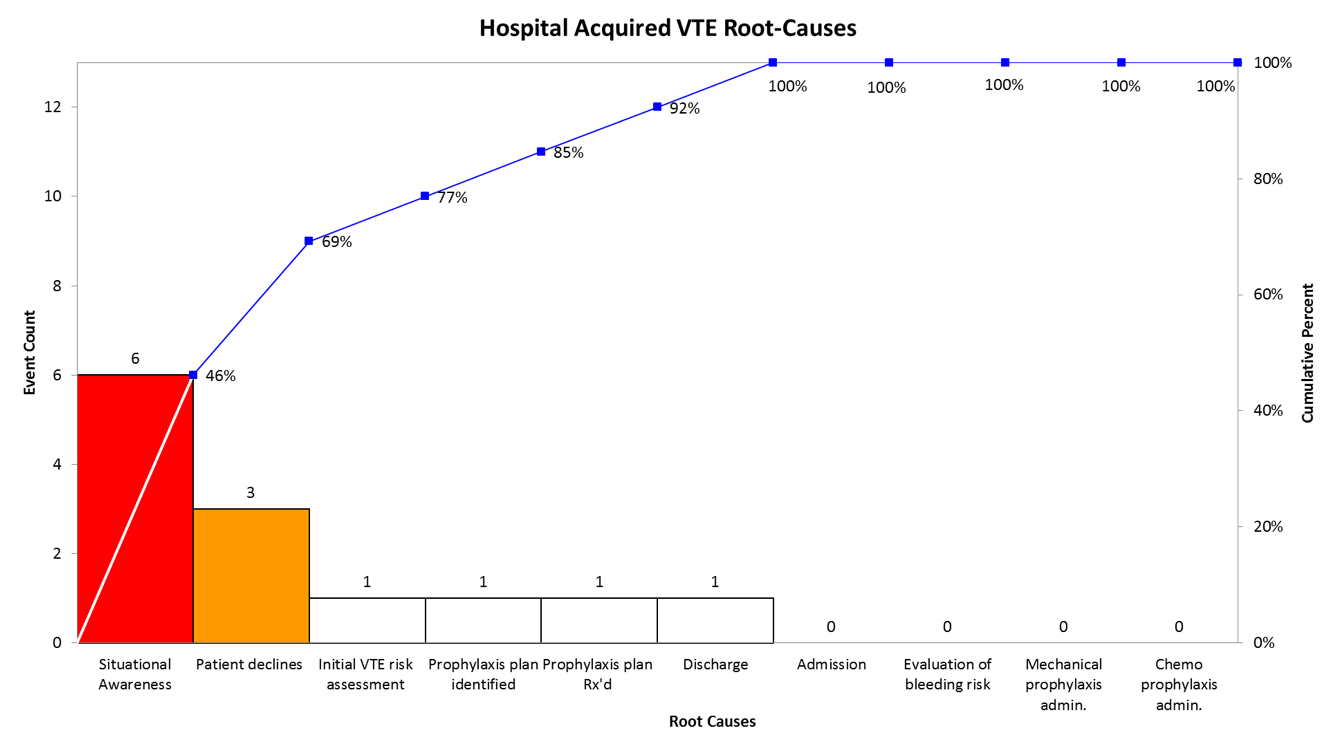
Their initial data using these tools revealed three common root-causes of HA-VTE at UNC: (1) incorrect VTE risk stratification at admission (2) a lack of situational awareness ( i.e. a patient’s VTE risk changes during their hospitalization and the treating clinicians do not adjust the prophylaxis–after an unplanned surgery for example) and (3) patients not adhering to the prescribed VTE prophylaxis. Efforts are underway to target all of these causes including the trialing of an evidence-based VTE risk stratification tool (Padua) in EPIC, partnerships with pharmacy to maintain a real-time awareness of a patient’s risk of VTE, and nursing scripting/patient education efforts to increase understanding and compliance with ordered VTE prophylaxis.
As a result of their efforts, Chang and Carlton Moore, MD, (also in the Division of Hospital Medicine) have been appointed the physician champions for VTE reduction at UNC-CH.
Decreasing the usage of low-value diagnostic testing and interventions in hospitalized patients – Michael Craig, MD, MPH, FHM
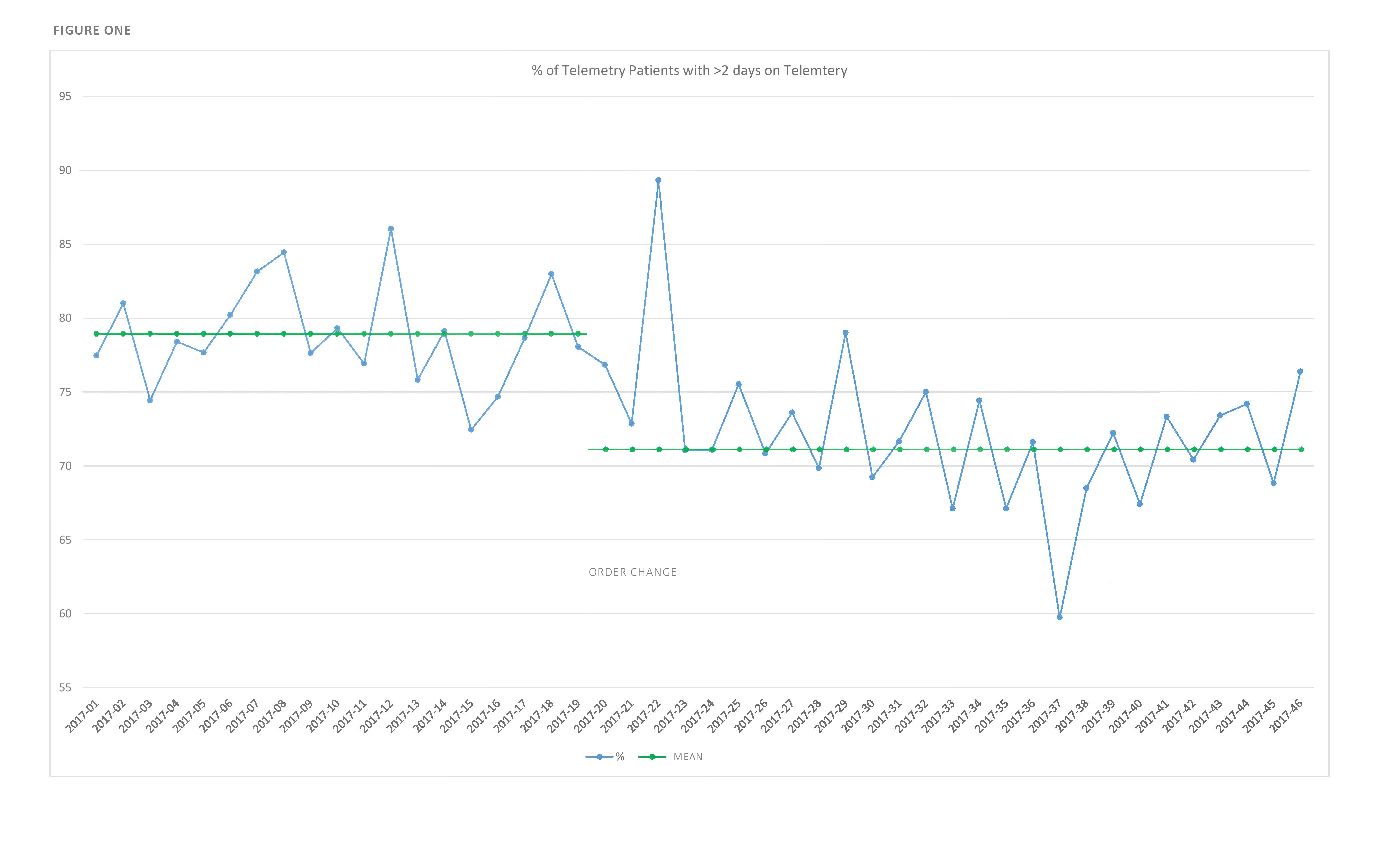
Cardiac telemetry in hospitalized patients is an often-overused resource. That overuse is driven both by use outside of accepted clinical indications and by continuing telemetry longer than is clinically indicated. In June of 2017, Michael Craig, MD, worked with the Value Care Action Group and other interested stakeholders across the UNC system to change cardiac telemetry orders within the Epic EMR. Telemetry orders now require both a clinical indication and duration. At UNC Medical Center, this change was associated with a decrease in the daily number of patients on telemetry monitoring by a mean of 11.4 patients (a 12% drop) and the proportion of patients getting more than two days of daily telemetry monitoring by 7.3%. This data was presented at the national Society of Hospital Medicine meeting in April. Dr., Craig is currently examining how this change impacted telemetry usage at other UNC facilities.
Along with co-authors John Stephens, MD, and Andrew Donohoe, MD, (also in the Division of Hospital Medicine), he published the article “Things we do for no reason: Echocardiogram in unselected patients with syncope” in the Journal of Hospital Medicine. This article discussed the low-yield of echocardiogram in syncope patients without pre-existing cardiac disease and a normal EKG.
Dr. Craig’s current project is exploring ways to reduce the use of IV antihypertensive medications in hospitalized patients.
End-stage liver disease project, IHQI funded 2017-18 – Escher Howard-Williams, MD
End-stage liver disease (ESLD) patients have complex and highly symptomatic disease, and suffer a high rate of morbidity and mortality. Those who are not transplant candidates often have uncontrolled symptoms and frequent readmissions. In fact, this group has the highest readmission rate at UNC. Care typically focuses on short term symptom management while in the hospital, but lacks anticipatory guidance and long term goals of care.
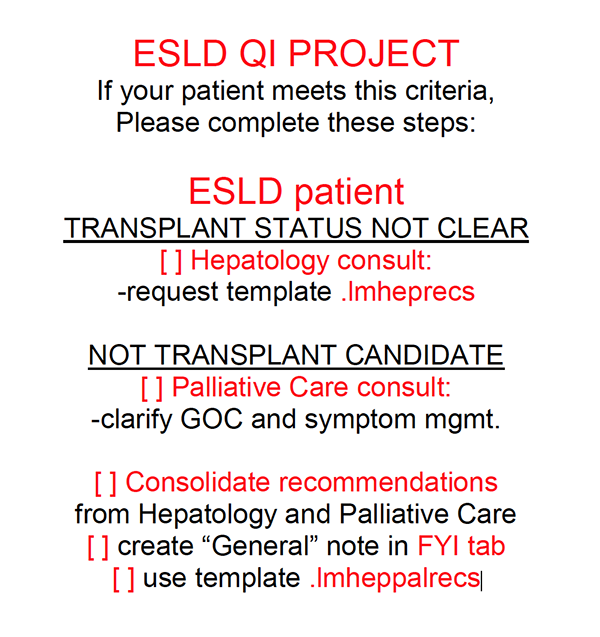
The ESLD QI project aims to create a standardized flow of care for decompensated ESLD patients who are not transplant candidates. The goal is to provide thoughtful and comprehensive care and guidance for these patients, while reducing overutilization of inpatient resources and readmission to the hospital. The flow of care includes creation of a living ACP/ICP note documented in their chart, with specific recommendations detailing goals of care by both Hepatology and Palliative Care consulting services.
Project collaborators include Escher Howard-Williams, MD, Ria Dancel, MD, Allen Liles, MD, Beth Ann Brubaker, MD, Eric Allman, NP, Martha Bausch, NP, and Heather Boykin, NP.