An adult who faithfully visits his PCP for annual well-checks shows no signs of mid-life worsening vision and falls short of scheduling a first-time comprehensive eye exam in his 40s. At age 50, he is diagnosed with glaucoma at an overdue screening, 10 years past the recommended age. The asymptomatic patient is shocked to learn that glaucoma has caused irreparable damage to his optic nerve. If no treatment is sought to slow progression of this devastating disease, his gradually worsening vision will lead to complete loss of eyesight. 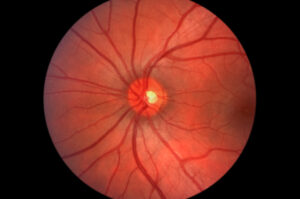
Had this health-conscious patient heeded ophthalmology field guidelines to visit an eye specialist in his 40s, his glaucoma could have been detected early on via a series of eye pressure, drainage angle, optic nerve and corneal tests. To draw attention to the alarming incidence of glaucoma in aging populations that goes widely undiagnosed in early stages, the American Academy of Ophthalmology (AAO) has designated January as “Glaucoma Awareness Month.” This month, the AAO is arming prevention-minded mid-lifers with a wealth of information on symptoms, causes and medical and procedural management of a multi-faceted ocular disease that is thankfully treatable once diagnosed.
- Recognize the severity of glaucoma. Cataracts and open-angle glaucoma are the leading causes of blindness worldwide, yet a stark difference sets these diseases apart. Procedural treatment for cataracts can restore vision. Medication and procedural treatment can only slow or prevent progression of the irreversible loss of eyesight caused by glaucoma.
- Stay attuned to any changes in vision. Some individuals eventually diagnosed with glaucoma suffer from diminished peripheral vision, yet they fail to get screened when these warning signs appear. From peripheral vision blind spots (open-angle glaucoma) to an “attack” of blurred vision, halos, mild headaches or eye pain (angle-closure glaucoma), the indicators of glaucoma are wide-ranging. Higher-than-normal eye pressure (ocular hypertension) places “glaucoma suspect” patients at greater risk. Glaucoma suspects can range from asymptomatic individuals to those whose optic nerve shows gradual change.
- Recognize higher risk. Asymptomatic adults who delay visiting an eye specialist in mid-life for a first-time comprehensive eye exam are perhaps at greatest risk of having glaucoma go undetected. Other groups of adults whose medical histories and backgrounds place them at heightened risk for glaucoma include: 1) Glaucoma family history; 2) African, Hispanic, or Asian heritage; 3) Ocular hypertension; 4) Farsightedness (hyperopia) and nearsightedness (myopia); 5) Previous eye injury; 6) Long-term medical steroid use; 7) Thin corneas; 8) Thinning optic nerve; and 9) Diabetes, migraines and high blood pressure.
- Discuss medication options that can slow or halt progression of glaucoma. Caught early, glaucoma can be treated with medicated, daily eye drops that lower eye pressure and prevent glaucoma from advancing. Patients taking a prescribed regimen can expect to visit their glaucoma specialist every 3 – 6 months to monitor glaucoma for any signs of progression.
- Discuss procedural treatment options with your glaucoma specialist. The laser surgery options available for treating two types of glaucoma — open-angle and angle-closure — improve drainage of aqueous humor and decrease alarming intraocular pressure (IOP) levels that cause progressive optic nerve damage. Two types of laser surgery relieve IOP damage to the optic nerve through correcting the intraocular drainage channel so that aqueous humor can exit the eye more efficiently.
- Trabeculoplasty: For open-angle glaucoma patients, laser trabeculoplasty surgery lowers the IOP by increasing the drainage through the trabecular meshwork.
- Iridotomy: For angle-closure glaucoma patients, iridotomy laser surgery cuts a small hole in the iris that improves the drainage angle and flow of aqueous humor.
Glaucoma presents a hurdle to clear and a homestretch to run in achieving a diagnosis that is followed by effective management of this damaging ocular disease. When elevated IOP and optic nerve abnormalities are detected in early-stage glaucoma, a diagnosis paves the way for patient and eye specialist to team up and jointly bear the responsibility of monitoring this condition to prevent its advancement.
UNC Department of Ophthalmology staffs world-renowned, board-certified glaucoma experts who specialize in state-of-the-art treatment for all types of glaucoma. Call UNC Kittner Eye Center at 984-974-2020 today to schedule a comprehensive eye exam that includes a replete panel of tests to screen for and diagnose glaucoma. To learn more about symptoms, causes, diagnosis and treatment of glaucoma, visit the AAO’s “What is Glaucoma?” page.
#glaucoma #eyehealth #ophthalmology #GlaucomaAwarenessMonth
