What are Pelvic Floor Disorders?

Pelvic health is the study and treatment of disorders that impact the pelvic floor which are the muscles, ligaments, and connective tissues that support the pelvic organs — the bladder, vagina, uterus, and rectum. Damage to or weakening of the pelvic floor can impact the normal functioning of these organs. Patients may be hesitant to discuss concerns or symptoms though it is estimated that pelvic floor disorders will impact one in three women during their lifetime.
Disorders
- Stress Urinary Incontinence – the loss of urine during the exertion of abdominal muscles, such as sneezing, coughing, laughing, and exercising.
- Urge Incontinence (OAB) – the inability to hold urine long enough to reach the restroom
Other UIs are:
- Mixed Incontinence – a combination of Stress Urinary Incontinence and OAB
- Overflow incontinence – less common among women – leakage may occur when the bladder reaches capacity
- Functional Incontinence – a form of OAB occurring due to physical conditions limiting one’s ability to reach the restroom in time (e.g., arthritis or using a walker)
- Fistula – an abnormal connection between the vagina and urinary track typically due to surgery, trauma or radiation.
- Diverticulum – urine collects in a pouch within the urethra and may leak out
There are currently several lifestyle changes, physical therapy, vaginal devices, medicines and procedures utilized in the treatment of UI.
Treatments for fecal incontinence include lifestyle changes, physical therapy, vaginal devices, medicines, and surgeries or procedures.
- Anterior Vaginal Wall Prolapse
- Posterior Wall Prolapse
- Apical Prolapse
- Rectal Prolapse
Some women may experience discomfort in the pelvic region, lower back, or when urinating or having bowel movements. This can progress and some women may even experience a bulge near the opening of the vagina.
Currently, there are lifestyle changes, physical therapy, vaginal devices, and surgical options available to treat POP.
- Voices for PFD.org
- AUGS: American Urogynecologic Society
- SUFU: Society of Urodynamics, Female Pelvic Medicine and Urogenital Reconstruction
- ICS: International Continence Society<
- IUGA: International Urogynecological Association
- SGS: Society of Gynecologic Surgeons
- AUA: American Urological Association
Women and PFD
Pelvic floor disorders (PFDs) may present for a variety of reasons. For some women there may be a genetic propensity. Lifestyle factors such as obesity, diet, smoking, or exertion may also be risk factors. Pregnancy, childbirth, menopause, and age can all lead to a weakening of the pelvic floor. Some women also develop PFDs while undergoing emotional stress. Health conditions relating to the nerves or lungs can also put undue stress on the pelvic floor muscles.
Clinical Challenges
PFDs are quite common – 50% of all women will experience symptoms throughout their lifetime. Patients may be hesitant to report symptoms due to embarrassment or a societal misunderstanding that PFDs are a normal part of aging. We, as clinicians and researchers, have limited information the biology of PFDs and a lack of preventative strategies. There are few long-term treatment options as well. This is an area of great opportunity for research that impacts a large percentage of the female population.
Prevalence
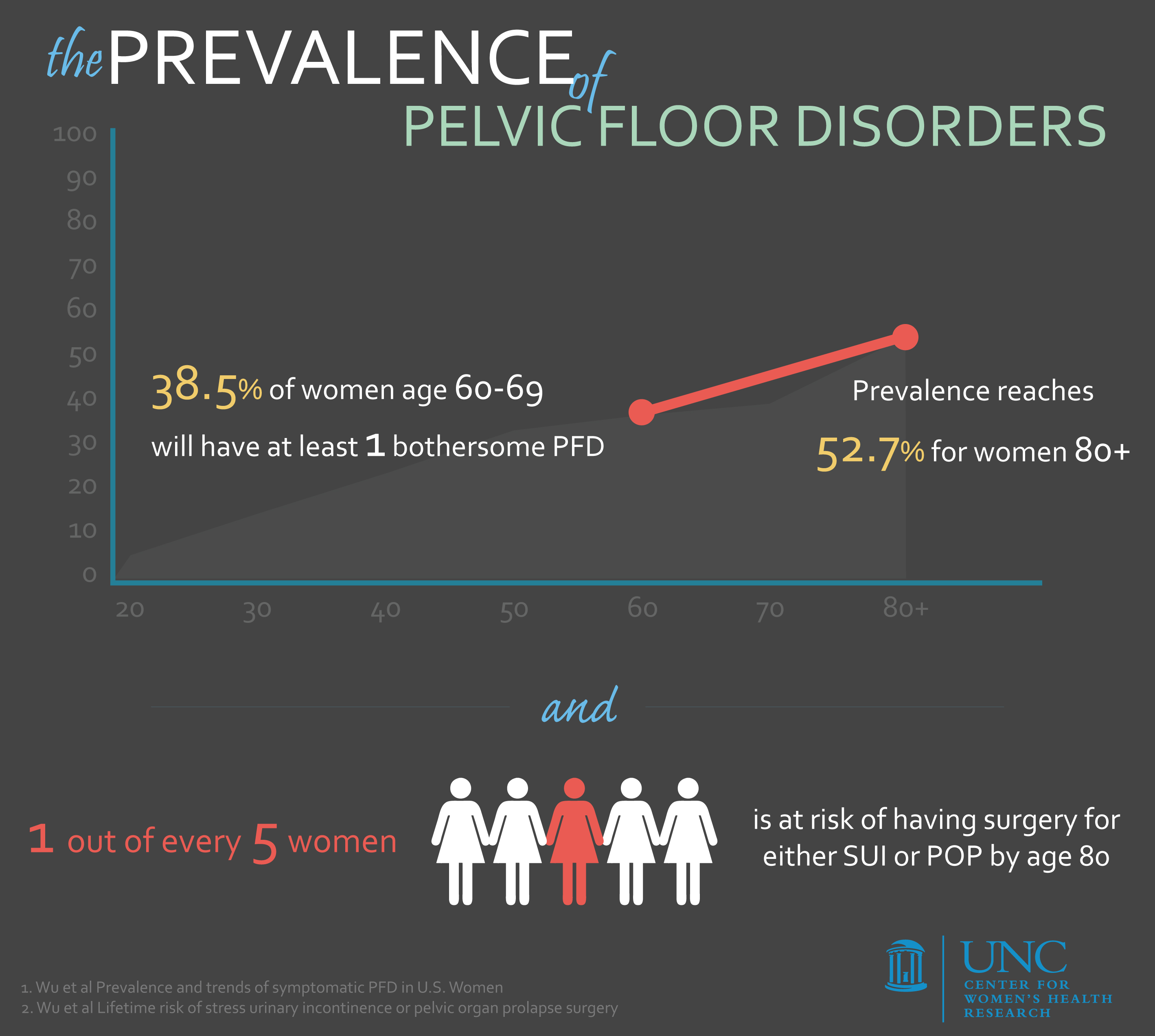
1. Wu et al Prevalence and trends of symptomatic PFD in U.S. Women
2. Wu et al Lifetime risk of stress urinary incontinence or pelvic organ prolapse surgery