

Benjamin Cobb
Associate Professor of Anesthesiology
Assistant Residency Program Director
Our program meets all the requirements of the American Board of Anesthesiology (ABA) and is fully accredited by the American Medical Association’s Accreditation Council for Graduate Medical Education (ACGME).
The mission of our residency is to train outstanding consultant anesthesiologists by providing a diverse, rigorous clinical experience combined with a carefully planned didactic curriculum. Our residents gain exposure to a wide array of patient populations and cases, including Level 1 trauma and solid organ transplants. Additionally, our program is unique in its focus on professional development, advocacy and wellness.
Thank you for your interest in UNC Anesthesiology!


Associate Professor of Anesthesiology
Assistant Residency Program Director


Professor of Anesthesiology
Vice Chair of Education


Edward A. Norfleet, MD ’70 Distinguished Professor of Anesthesiology
Residency Program Director


Interim Chair of Anesthesiology
Professor of Anesthesiology


Assistant Professor of Anesthesiology
Assistant Residency Program Director


Professor of Anesthesiology
Associate Residency Program Director
Residency Recruitment Chair


Professor
Immediate Past Chair
UNC Hospitals CMO
Learn about what makes our residency program a unique place to train!
View All
The Academic Medicine Rotation is a month-long non-clinical rotation where the interns are exposed to aspects of medicine not easily taught in the OR. The focus is on professionalism, teaching, leadership, business of medicine, public speaking, and quality improvement. During the month each intern will design, implement, and present a quality improvement project.

A Wellness Committee was formed in 2015 composed of faculty members, residents, and CRNAs. The purpose of the Department of Anesthesiology Wellness Committee is to promote the physical and emotional health and well-being of all faculty and staff.

Each resident spends a total of 2-4 weeks dedicated solely to learning TEE (an additional 4 weeks of elective time is possible during CA-3 year). During these 2-4 weeks, the resident performs all TEE exams for cardiac cases, in addition to all exams requested for non-cardiac cases. Residents are one-on-one with a Cardiac Anesthesiology attending for each exam.
We offer departmental educational sessions throughout the week. Our residents regularly participate in preparatory sessions for the ABA written and oral boards as well as the OSCE exam. Additionally, our residents play an active role in Morbidity and Mortality Conference, Chair’s Conference, and others. Regular subspecialty conferences help provide additional exposure to topics such as point-of-care ultrasound (POCUS), pediatric anesthesiology and transesophageal echocardiography (TEE). We utilize the expertise of our education specialist and renowned faculty to incorporate active learning techniques.
Our quarterly Journal Club program is geared toward exploring the critical aspects of research study design and manuscript preparation.
Introductory sessions are geared towards new residents and concentrate on research methodology and manuscript preparation. Advanced sessions are geared toward discussing landmark articles in anesthesiology as well as research studies conducted by members of our department.
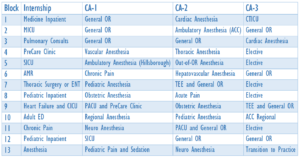
Residents who match into the categorical positions will complete a clinical base year where they will rotate through various medicine, surgical, and pediatric specialties. Additionally, we include anesthesia-related rotations such as chronic pain, academic medicine rotation, and transition to anesthesia. At the end of the clinical base year, residents have the opportunity to be paired with more senior residents to smoothly transition into the anesthesia years of residency.
 Our Departmental Wellness Committee was founded in 2015 and is composed of faculty, residents, CRNAs, and support staff. The purpose of the committee is to promote the physical and emotional health and well-being of all departmental members. Activities include:
Our Departmental Wellness Committee was founded in 2015 and is composed of faculty, residents, CRNAs, and support staff. The purpose of the committee is to promote the physical and emotional health and well-being of all departmental members. Activities include: