Testicular Cancer
Page Contents
- The incidence of testicular cancer in the United States is 5/100,000 men resulting in approximately 8,400 cases per year
- There are several distinct types of testicular cancers, also called germ cell tumors (GCT). Seminoma, which comprises ~50% of all tumors, can be divided into classic seminoma and spermatocytic seminoma. The remaining ~50% of tumors are non-seminomatous germ cell tumors (NSGCTs) which are composed of the following categories: embryonal carcinoma (EC), yolk sac tumors or endodermal sinus tumors, choriocarcinoma, teratoma, and mixed GCT
- The most common presentation is seminoma confined to the testicle, which represents approximately 50% of the cases, and only 10-30% of men will present with metastatic disease.
- The incidence of testicular cancer is highest among non-Hispanic whites, lowest among African-Americans, while the incidence for Asian and Hispanic men falls in between.
- Risk factors for testicular cancer include: cryptorchidism (undescended testis), intratubular germ cell neoplasia (ITGCN), and family or personal history of testicular cancer.
Symptoms
Learn more about the symptoms that can be associated with testicular cancer.
(Read More)- A painless testicular mass is the most common presentation of testicular cancer.
- Other presenting symptoms can be related to metastatic disease: abdominal mass, neck mass, shortness of breath, and coughing up blood.
Diagnosis
How is testicular cancer diagnosed?
(Read More)- Men with a testicular mass, or suspected mass, should undergo a scrotal ultrasound as the initial test.
- Testicular cancer is unique because serum tumor markers (STM), which are found with a blood test, are utilized in the diagnosis, staging, and monitoring of disease therapy, and should be obtained if a testicular mass is present or suspected prior to removal of the testicle (orchiectomy).
- Alpha-fetoprotein (AFP)- Half-life 5-7 days, elevated in 50-80% of NSGCT, EC and yolk sac tumor produce AFP, seminoma and choriocarcinoma do not, can be elevated in patients with liver disease, hepatocellular carcinoma, stomach/pancreas/biliary duct/lung cancers.
- Beta-Human Chorionic Gonadotropin (bHCG)-Half-life 24-36 hours, elevated in 20-60% of NSGCT and 15% of seminomas, produced by EC/choriocarcinoma/seminoma, can be elevated in liver/biliary/pancreas/stomach as well as lung/breast/kidney/bladder cancers, can be elevated secondary to marijuana use.
- Lactate dehydrogenase (LDH)– Half-life 24 hours, a non-specific marker of GCT, a measure of disease burden, mainly utilized for staging at the time of diagnosis.
- A radical inguinal orchiectomy is the standard treatment of the primary tumor if testis cancer is suspected. This involves removal of the testicle and spermatic cord through an inguinal incision. Testicle removal or biopsy through the scrotum should not be performed. Testis sparing surgery can be considered in a small tumor in a solitary testis or when small bilateral tumors exist. Once testicular cancer has been diagnosed complete staging should be performed with computed tomography (CT) of the chest/abdomen/pelvis with oral and intravenous contrast.
Staging
The stage of a patient’s testicular cancer is based on the use of CT scans and serum tumor markers.
(Read More)This allows for the evaluation of lymph node involvement and presence of metastatic disease (i.e. spread to the lung). Using this information patients are staged in groups I-III. The factors which dictate what stage a patient is in are: the presence or absence of enlarged retroperitoneal lymph nodes (located behind the intestines), the size of involved lymph nodes, the presence or absence of metastatic disease, and the presence and level of serum tumor markers after orchiectomy. The below tables summarizes the American Joint Committee on Cancer staging for testicular cancer.1
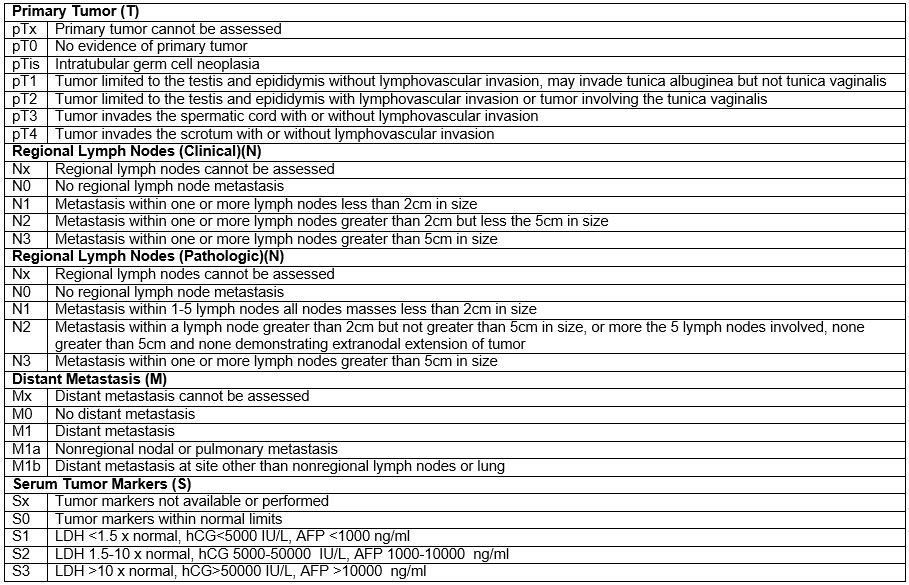
AFP-alpha-fetoprotein, hCG-human chorionic gonadotropin, LDH-lactate dehydrogenase
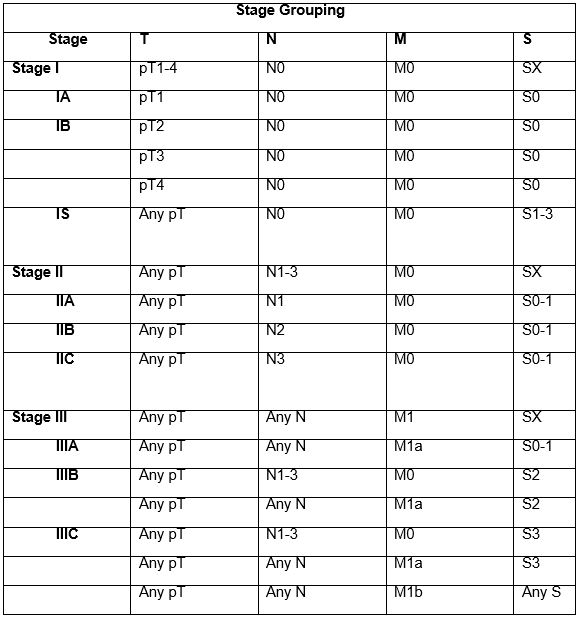
AFP-alpha-fetoprotein, hCG-human chorionic gonadotropin, LDH-lactate dehydrogenase
Treatment
Learn more about testicular cancer treatment
(Read More)- The treatment of testicular cancer depends on the stage of cancer as well as if the primary tumor within the testicle is a seminoma or non-seminomatous.
- Stage I Seminoma: For patients with pure seminoma stages IA and IB, treatment options following orchiectomy include (i) Surveillance (ii) Radiotherapy (iii) Chemotherapy with carboplatin (1 or 2 cycles). More than 80 percent of patients with stage I seminoma are cured with orchiectomy alone, so surveillance is generally recommended for these patients. Survival for stage I seminoma is 99% irrespective of the management strategy used.
- Stage IIA and IIB seminoma: Radiation to the retroperitoneal lymph nodes.
- Stage IIC and III seminoma: Chemotherapy with 3 cycles of bleomycin, etoposide, and cisplatin (BEP) or 4 cycles of etoposide and cisplatin (EP).
- Stage I non-seminoma: For men with stage I NSGCTs approximately 70% will be cured with orchiectomy alone. The management options for these patients include (i) Surveillance (ii) retroperitoneal lymph node dissection (RPNLD) (iii) Cisplatin-based chemotherapy. Additional treatment following orchiectomy can reduce the risk of disease recurrence, but will overtreat many patients. In addition, although the risk of recurrence is approximately 30% for men undergoing surveillance, treatment at the time of recurrence is almost always curative.
- Stage IIA and IIB non-seminoma: Can both be treated with primary chemotherapy consisting of 4 cycles of EP or 3 cycles of BEP; however, in cases of Stage IIA with normal serum markers, primary RPLND is an appropriate treatment option
- Stage IIC and III non-seminoma: Primary chemotherapy with either 3 cycles BEP or 4 cycles EP versus 4 cycles of BEP depending on the severity of the disease.
Retroperitoneal lymph node dissection (RPNLD)
- RPLND is a surgical procedure to remove lymph nodes surrounding the inferior vena cava and aorta. These lymph nodes are usually the first location testicular cancer will spread to the outside of the testicle and the removal of these lymph nodes can play an important role the treatment of testis cancer both before and after chemotherapy. The standard approach to this procedure is with open surgical techniques which use an incision from the sternum to below the belly button. Patients generally stay in the hospital 3-5 days and return to full activities between 6-8 weeks. Some patients may be appropriate candidates for minimally invasive approaches (laparoscopic or robotic) that can reduce hospital stays and time to full recovery.
- Edge SE, Byrd DR, Compton CC.: AJCC Cancer Staging Manuel. 7th ed., 469-73, 2010
Resources
Here are additional resources for learning more about testicular cancer.
