Postoperative Care
Page Contents
Expectations: Hospital
- You should expect to be at the hospital for approximately 4-5 days.
- After waking up from surgery, you will notice several tubes and medical equipment. Here is a list of some of the things you may see:
- A drain in your abdomen (called a Jackson Pratt, or JP drain) that removes excess fluid from the surgical site. This is usually removed prior to discharge.
- An IV to administer medications.
- A heart monitor.
- Two stents (small plastic tubes) coming out of your stoma. These will be removed once your urologist feels it is safe, typically during your postoperative appointment.
- An ostomy bag over your stoma.
- A tube placed on your nose to administer oxygen.
- Massaging stockings to prevent blood clot formation.
- Dressing located over your incision(s)
- For females, gauze may be placed in your vagina to prevent bleeding.
- Complications can, unfortunately, occur after bladder removal. Fortunately, most of these complications are mild and may include:
- Urinary tract infection
- Small bowel obstruction or ileus (a condition in which your bowels are “asleep” and need time to “wake up”)
- Wound infection
- Heart trouble
- Lung issues such as pneumonia or shortness of breath
- Blood clots
- Nerve problems, such as numbness or weakness
- Stone formation
- Urinary leakage
- Metabolic or electrolyte issues
- Unfortunately, after going home, about a quarter of patients may have to return to the hospital for further treatment and readmission. If you are experiencing any side effects when you go home, it is important to contact your urology care team in a timely manner to make sure that any side effects are treated before they worsen
Expectations: Home
Blood Clots
Patients will be limited in their activity upon returning home. This puts them at risk for developing dangerous blood clots. To minimize this risk, patients are instructed to administer a Lovenox (a blood thinner) shot every day for approximately 28 days postoperatively. This should be taught before leaving the hospital. Some patients also have a home health nursing arranged, who would be happy to assist and teach patients. If you would like a review, watch this step-by-step instructional video here:
Learn more about the steps of proper administration and disposal of LOVENOX
If you have any additional questions, you can call the Urology Clinic at 984-974-1315 to ask for help. If you need to reach the Wound Ostomy Nurse Consultant the clinic can connect you.
Stoma/Ostomy Care
Learning how to manage an ostomy is a new skill that can feel overwhelming. Patients typically get more accustomed to their stoma with time. However, some questions or challenges, such as leaking from their bag, may persist. Here are several videos describing how to care for your ostomy.
Supply Descriptions
There is a wide variety of supplies that can be confusing and overwhelming at first. Here is a video describing some of these supplies.
Changing Your Appliance
After coming home from the hospital, patients typically need to change their ostomy bag by day 3, but this is dependent on the patient and may be earlier or later (up to 5 days). Below is a video describing how to change an ostomy bag. If you need more help, call the Urology Clinic or send them a message using MyChart. The nurse can assist you or connect you with a wound and ostomy nurse consultant.
Blood in Urine
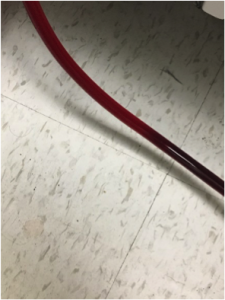
Many patients wonder if it is normal to see blood in their urine. The answer to this question is yes, this can be seen following an appliance change, gentle washing, or exercise. This type of “bleeding” is very similar to bleeding from your gums after flossing or brushing your teeth. Of course, not all types of bleeding are normal, particularly if the blood in your urine is thick or has large clots. Below are some pictures of normal urine colors and some pictures of when you may need to contact our team. If you have questions, please call our clinic at 984-974-1315.
Normal:
Abnormal: If your urine looks similar to the below image, you should contact the urology office immediately at 984-974-1315
Home Health Supplies
This video describes how to obtain monthly ostomy supplies upon returning home from the hospital.
Emptying Pouch
This video describes how to empty your pouch, as well as how often you should be doing so. This also briefly discusses a nighttime drainage bag that you may want to use while you are asleep.
Leaks
The following video describes common reasons for leaks and ways to address these problems.
Skin Breakdown
This video describes ways to address skin breakdown around your stoma, which includes the crusting technique.
Hernia
This video describes symptoms of a hernia and how you may be able to address them. If you think you may have a herniated stoma, please contact your provider immediately.
Sexuality and Clothing
The following video describes options regarding undergarments and swimwear for both men and women that allow you to discretely secure your pouch.
FAQs
This video addresses a variety of frequently asked questions that have not already been discussed in previous videos.
Support Resources
This video provides support resources for patients to turn to for educational and emotional needs.
Showering/Bathing
Showering after surgery is safe, but patients must be careful as they may be weak after the surgery. Having a loved one nearby may be helpful to prevent falls. You may shower and it is okay if your incisions have water run over them. Bathing after surgery should be done only AFTER 2 weeks. We recommend that patients avoid baths for 2 weeks after surgery because bath water can have dirt (from your body). Submerging in water can cause problems with the incision, which is not fully healed yet.
Activity/Exercise
While it may be tough, patients are strongly encouraged to begin walking early as this is one of the most important things they can do to improve recovery and prevent complications after surgery. Staying active lowers your chance of life-threatening blood clots, lung collapse, infection, and wound problems.
We recommend starting slow the first week and gradually increasing total activity daily. It may take weeks to several months before fully regaining baseline energy and stamina, but do not get discouraged. Aim to spend at least 8 hours out of bed, even if that is sitting upright in a chair. Set daily walking goals and milestones. For example, take a leisurely walk around the neighborhood each day. By week 3, patients should be walking several times a day. By week 6, patients can safely lift more than 10 pounds. We encourage patients to continue setting goals and increasing their activity level.
Nutrition
It is very important for patients to maintain a nutritious diet and stay hydrated following surgery. We recommend a diet high in protein and calories to help maintain your weight and muscle mass. However, decreased appetite and weight loss are very common. Here are some tips to help prevent this:
- Eat 5-6 smaller meals, including a snack around bedtime
- Eat snacks high in protein/fat like peanut butter crackers, nuts, and granola bars
- Increase your fat intake with foods such as avocados/guacamole, nut butters, olive oil, and butter for more calories
- Drink liquids that contain calories such as milk, soup, and protein drinks in between meals. These should be avoided during mealtime
Following surgery, it is normal for patients to have a change in taste and/or appetite. If you are experiencing this, here are some tips:
- Eat foods that look and smell good to you
- Marinate foods
- Try tart foods and drinks
- Make foods sweeter
- Add flavor
- Eat with plastic utensils instead of metal
- Patients should aim to drink at least 6-8 glasses (8oz) of water or fluid per day. A good way to judge your fluid intake is by the color of your urine (clear to light yellow urine is excellent!).
- We will make sure one of our nutritionists meets with each patient during their first clinic visit. They have a lot of experience in helping post-cystectomy patients keep healthy diets.
FAQ: What can I do for constipation?
Constipation is not uncommon and can be very frustrating. You will often be prescribed stool softeners and laxatives to take following your discharge from the hospital. Additionally, be sure to drink at least 8 cups of liquid per day. Also try hot liquids such as coffee, tea, or soup and eat high fiber foods such as nuts, seeds, and whole grains. Increasing daily activity may also help. If you continue to experience constipation, contact your urologist and they can help.
FAQ: Is it normal to feel bloated?
The answer to this is yes, this is normal. Try to eat 5-6 smaller meals per day and consider eating cooked fruits and vegetables rather than raw. You can also try sipping on tea, broth, or warm water with lemon. You should limit spicy, greasy, and foods high in fiber.
For more information like this, check out this article on nutrition and bladder cancer from a nutritionist who specialized in bladder cancer.
Coping after Cystectomy
Bladder cancer is a tough disease and feelings of sadness and/or anxiety are not uncommon, particularly after surgery. Undergoing bladder cancer surgery is a major life change and it can be difficult for patients to adjust. All of these feelings can be a normal part of coping with the disease and new lifestyle. There are many free resources out there to help:
- UNC Comprehensive Cancer Support Program – this is an entire program to help patients and their loved ones with the emotional and physical challenges of a new cancer diagnosis.
- In-person support groups exist in Chapel Hill, Durham, and Charlotte. Find out more here: https://www.bcan.org/in-person-support-group
- If you prefer to talk over the phone, BCAN has two helpful services: the BCAN Connection (1-888-901-2226, ext 207) and Survivor 2 Survivor (1-888-901-2226, ext 212).
Finally, if you prefer online support, visit the BCAN patient forum at https://www.inspire.com/gropus/bladder-cancer-advocacy-network/
Living with Urinary Diversion
Urinary diversion is a life-changing procedure and finding your new normal can be challenging. It is important to know that you are not alone, and others have been exactly where you are right now. Bladder Cancer Advocacy Network (BCAN) is a great resource for patients.
Here is a link that will direct you to the BCAN website page containing videos of eight bladder cancer survivors and how they found their new normal. https://www.bcan.org/the-new-normal/
Neobladders
content coming soon
What if my cancer returns?
The risk of your cancer returning after the removal of your bladder varies per patient. The different factors that help to determine this risk include the type of cancer, the grade and stage of your cancer, and the amount of tumor successfully removed during surgery. All patients are monitored for recurrence following surgery. If your bladder cancer were to return, treatment options will depend on the type and location of the cancer, treatments you’ve already had, and your current health and willingness to undergo more treatment. Some options might include surgery, radiation therapy, chemotherapy, immunotherapy, or a combination of these. If all standard treatments fail to control the cancer, you may consider taking part in a clinical trial of a new bladder cancer treatment. You will discuss these options with your urologist and decide what may be the best option for you.
Pain Management
Pain following surgery is expected, though it should be improving day by day. If it is not, our team wants to know about it. We have many ways of managing pain, including a combination of Tylenol, ibuprofen, and narcotics. Patients should aim to take as little narcotics (such as hydrocodone (Vicodin), oxycodone (OxyContin), methadone, and fentanyl) as possible to control pain and try lowering the dose every few days until no longer needed. This will help to minimize the many side effects these can cause while also minimizing the risk for addiction. Risk factors for addiction include a combination of genetics, environment, and development, according to current research. You should discuss with your urologist any concerns you may have with these medications as soon as possible.
For additional information about managing pain, check out this list of frequently asked questions: http://www.urologyhealth.org/educational-materials/frequently-asked-questions-pain-management
Palliative Care
If pain or other postoperative symptoms persist, palliative care may be an option. Palliative medicine is a subspecialty aimed at holistic treatment of quality-of-life issues, particularly in cancer patients. Palliative care specialists may address any of the following: ongoing post-surgical pain, nausea, vomiting, nutrition, sexual side effects, emotional support, spiritual side effects, emotional support, spiritual support, and advanced care planning. Check out this brochure: https://www.bcan.org/wp-content/uploads/2017/Palliative-Care.pdf
Additionally, some patients have benefited from additional support such as massage therapy, acupuncture, alternative medicine, mindfulness, and yoga. These can be very helpful in navigating through the cancer journey. If interested, check out the resources here: http://unclineberger.org/patientcare/support/ccsp/integrative-medicine.
NOTE: Patients should ask their doctor what they might recommend.
Sleep Management
Getting restful sleep following surgery can be challenging for some patients. However, sleep is an important factor in recovery. Here are some symptoms that may indicate you are not getting a restful night sleep:
- Fatigue
- Difficulty with attention, concentration, or memory
- Daytime sleepiness
- Impulsiveness or aggression
- Lack of energy or motivation
- Errors or accidents
Here are some simple recommendations that may help establish better sleep habits:
- Maintain a consistent sleep schedule by waking up at the same time every day
- Set a time to go to bed that is early enough to allow you at least 7 hours of sleep
- Do not go to bed unless you are sleepy
- If you don’t fall asleep within 20 minutes of going to bed, get out of bed
- Establish a relaxing bedtime routine
- Use your bed only for sleep
- Make your bedroom quiet and relaxing
- Keep the room at a cool, but comfortable, temperature
- Limit exposure to bright light in the evenings
- Turn off electronic devices at least 30 minutes before bedtime
- Don’t eat a large meal before bedtime
- Exercise regularly and maintain a healthy diet
- Avoid consuming caffeine in the late afternoon or evening
- Avoid consuming alcohol before bedtime
- Reduce your fluid intake before bedtime
If you are waking up at night to empty your pouch and this is interfering with your ability to get a restful sleep, you may want to consider a nighttime drainage bag, or leg bag, to collect the urine while you sleep. A video on how to use this is located in the Ostomy/Stoma Care section of this page, listed as the “Emptying Pouch” video.
If you continue to experience symptoms after trying these recommendations, please discuss this with your doctor.
You may also check out the link for more information about sleep. https://www.cdc.gov/sleep/resources.html
Follow-Up Care
Postoperative Visit
Patients are scheduled to see their urologist about 5-10 days after discharge. During this visit, your urologist will assess your functional status, remove your stents, and review your pathology. This would be a great time to discuss any concerns you may have. However, if you have any concerns prior to this office visit, please don’t hesitate to contact us. Your urologist may check some blood work and may also order an ultrasound of your kidneys to make sure that they are draining well/properly.
Continued Monitoring
Many patients find themselves wondering if their cancer is going to return. This is a very common question and a good one. After surgery, you will need to continue following up with your healthcare provider for assessments. These assessments may include the following:
- Imaging (e.g. CT scan or MRI) about every 6-12 months for 2-3 years, then annually thereafter.
- Lab tests (including kidney and liver function tests) every 3-6 months for 2-3 years, then once per year thereafter.
- Assessment of the quality of life issues such as urinary symptoms and sexual dysfunction.
These assessments will help us determine if your cancer has returned. These visits will also allow you the opportunity to ask any questions you may have in person, so please do not hesitate to do so.
We recommend that you keep records of your bladder cancer treatment plan, particularly any lab work or imaging studies that may have been completed during outside hospitalizations or evaluations. This outside information is not always accessible between different hospital systems and this allows your urology team to monitor how you are doing.
We also recommend that you share these records with your primary care provider so that they can work with you to optimize your health and medications postoperatively.
Caregiver Information
Some patients have caregivers who help them through surgery. Their constant devotion can cause them to feel stressed and overwhelmed. Some red flags to watch out for in your caregiver include the following:
- Fatigue
- Poor immune function
- Missing work or being emotionally absent while at work
- Isolation
- Anxiety
- Depression
- Guilt
If your caregiver is showing any of these signs, he/she may not be taking care of themselves. However, they must take care of themselves first to be able to help others. If you are concerned for your caregiver, let them know that their feelings are not uncommon. You should then direct them to the following link that discusses ways to recognize red flags and how to get the care and find the resources they may need. Some of the resources mentioned in the video includes the American Cancer Society, Cancer Care, Caregiver Action Network, Family Caregiver Alliance, National Alliance for Caregiving, Strength for Caring. https://www.bcan.org/caregiver/
This journey is certainly not easy and everyone has different setbacks and accomplishments at different times. Sharing your story can help others who are going through the same experiences. This can be accomplished in various ways, whether that be in support groups or creating your own webpage or fundraiser.
Check out this link to learn more: http://support.bcan.org/site/TR/Events/General?fr_id=1520&pg=entry


