2020 Program
2020 Award Recipients
Best Poster by an Undergraduate Student
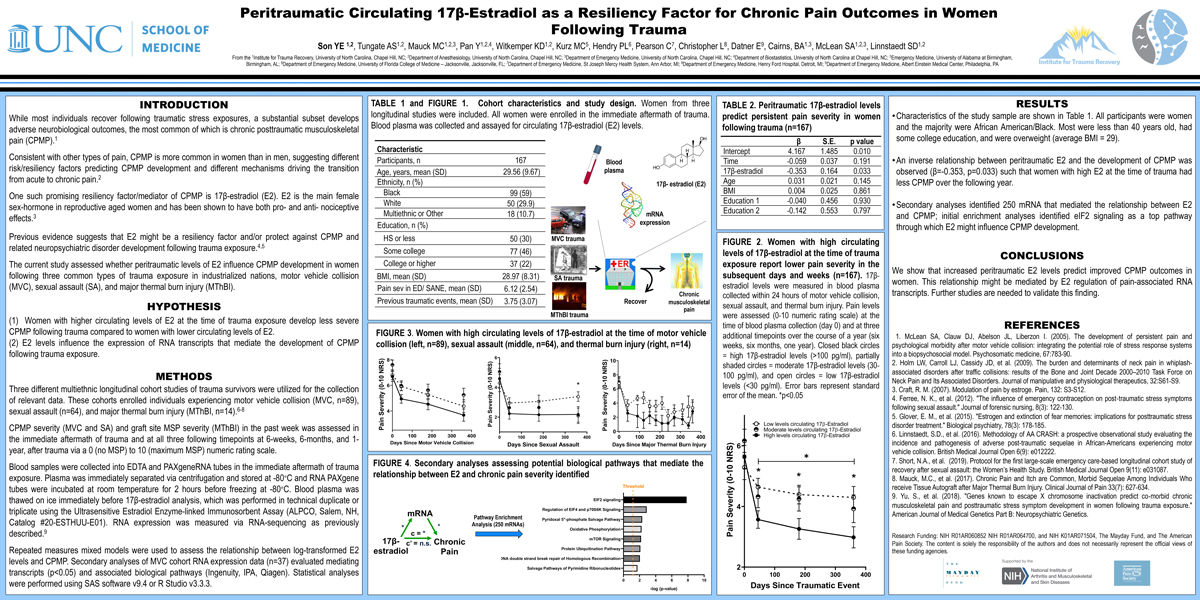
Peritraumatic Circulating 17β-Estradiol as a Resiliency Factor for Chronic Pain Outcomes in Women Following Trauma
Esther Son
 Esther Son is a sophomore Neuroscience major and medical professions Spanish minor at UNC-CH. She is an undergraduate research assistant at Dr. Linnstaedt’s lab, as part of the UNC Institute of Trauma Recovery team. Her primary and current project focuses on biomarkers that may predict post-traumatic adverse neurobiological outcomes, such as chronic pain and stress. Outside of research, she is an advocate for mental health and a leader in UNC Mental Health Ambassadors, as well as UNC Heeling in Harmony, which promotes healing through music among various communities in Chapel Hill. She hopes to continue research throughout her undergraduate career and plans to attend medical school after graduation.
Esther Son is a sophomore Neuroscience major and medical professions Spanish minor at UNC-CH. She is an undergraduate research assistant at Dr. Linnstaedt’s lab, as part of the UNC Institute of Trauma Recovery team. Her primary and current project focuses on biomarkers that may predict post-traumatic adverse neurobiological outcomes, such as chronic pain and stress. Outside of research, she is an advocate for mental health and a leader in UNC Mental Health Ambassadors, as well as UNC Heeling in Harmony, which promotes healing through music among various communities in Chapel Hill. She hopes to continue research throughout her undergraduate career and plans to attend medical school after graduation.Musculoskeletal pain is common following traumatic/stressful life events and is more common in women than men. However, resiliency factors that predict improved chronic posttraumatic musculoskeletal pain (CPMP) in women are poorly understood. In the current study, we examined whether peritraumatic circulating 17β-estradiol (E2) levels influence CPMP trajectories in women. We measured Peritraumatic E2 levels via ELISA in plasma samples (n=167) derived from three multiethnic longitudinal cohort studies of trauma survivors. These cohorts enrolled individuals experiencing motor vehicle collision (MVC, n=89), sexual assault (n=64), and major thermal burn injury (n=14). We assessed CPMP (0-10 numeric rating scale) at 6-weeks, 6-months, and 1-year following traumatic stress exposure. We used repeated measures mixed models to test the relationship between log-transformed E2 levels and CPMP. Secondary analyses of MVC cohort gene expression data (n=37) evaluated mediating transcripts and associated biological pathways (Ingenuity, IPA). We observed an inverse relationship between peritraumatic E2 and the development of CPMP (β= -0.353, p=0.033) such that women with high E2 at the time of trauma had less CPMP over the following year. Secondary analyses identified 250 mRNA that mediated the relationship between E2 and CPMP; initial enrichment analyses identified eIF2 signaling as a top pathway through which E2 might influence CPMP development. From these results, we conclude that increased peritraumatic E2 levels predict improved CPMP outcomes in women.
(Click here for large version)
Contact: eson@live.unc.edu
Best Poster by a Graduate Student, Fellow, or Resident
Metabolic Effects of High Intensity Interval Training and Essential Amino Acid Supplementation: Modulatory Effects of Sex
Katie Hirsch, PhD, EP-C, CISSN
 Katie Hirsch recently completed her PhD in Human Movement Science under the mentorship of Dr. Abbie Smith-Ryan in the Applied Physiology Lab in the Department of Exercise and Sport Science. Katie conducts research in the areas of nutrition and exercise for the improvement of body composition and metabolic health and her dissertation focused on the metabolic effects of high-intensity interval training and essential amino acid supplementation. In June, she will begin postdoctoral work at the University of Arkansas for Medical Sciences, using isotope tracer techniques for the measurement of muscle and protein metabolism. Katie completed her MA in Exercise Physiology at the University of North Carolina at Chapel Hill and her BS in Exercise Science at Truman State University in Kirksville, Missouri. Katie is an ACSM Certified Exercise Physiologist and a Certified Sports Nutritionist with the International Society of Sports Nutrition (ISSN).
Katie Hirsch recently completed her PhD in Human Movement Science under the mentorship of Dr. Abbie Smith-Ryan in the Applied Physiology Lab in the Department of Exercise and Sport Science. Katie conducts research in the areas of nutrition and exercise for the improvement of body composition and metabolic health and her dissertation focused on the metabolic effects of high-intensity interval training and essential amino acid supplementation. In June, she will begin postdoctoral work at the University of Arkansas for Medical Sciences, using isotope tracer techniques for the measurement of muscle and protein metabolism. Katie completed her MA in Exercise Physiology at the University of North Carolina at Chapel Hill and her BS in Exercise Science at Truman State University in Kirksville, Missouri. Katie is an ACSM Certified Exercise Physiologist and a Certified Sports Nutritionist with the International Society of Sports Nutrition (ISSN).Katie R. Hirsch1, Casey E. Greenwalt1, Hannah E. Saylor1, Courtney H. Harrison1, Lacey M. Gould1, Alyson G. Nelson1, Dalton W. Wheeless1, Gabrielle J. Brewer1, Malia N.M. Blue1, Abbie E. Smith-Ryan1
1Applied Physiology Laboratory, University of North Carolina, Chapel Hill, NC 27599
Paradoxical responses to exercise (i.e. gaining body fat) have previously been reported in women; high-intensity interval training (HIIT) may elicit more positive responses. This study evaluated the modulatory effects of sex on body composition and metabolism following eight weeks of HIIT and/or essential amino acid (EAA) supplementation in overweight/obese adults. Sixty-six participants (50% female; Age: 36.7±6.0 yrs; %BF: 36.0±7.8%) were randomly assigned to: 1) HIIT, cycle ergometry 2 d/wk; 2) EAA supplementation, twice daily; 3) HIIT+EAA; or 4) no intervention (CON). Body composition, resting metabolic rate (RMR), substrate metabolism (RER), and cardiorespiratory fitness (VO2) were measured at baseline, 4wks, and 8wks. There was no significant interaction effect for sex between groups or across time for any outcome variable (p>0.05). Analysis of mean change scores from weeks 0-8 showed no significant changes in body composition in men or women. HIIT increased RMR in men (Δ±SE [95% CI]: 133.92±45.51 kcal/d; [42.63,225.21]) and fat oxidation in women (RER: -0.05±0.02 a.u.; [-0.08,-0.02]). EAA increased RMR (92.15±39.01 kcal/d; [13.91; 170.40]) and fat oxidation (RER: -0.04±0.02 a.u.; [-0.08,-0.01]) in men, but not in women. HIIT and HIIT+EAA improved VO2 in men and women; significant increases in men occurred from 0-4wks with HIIT+EAA (5.98±1.84 ml/kg/min; [2.30,9.66]), while significant increases in women occurred during weeks 4-8 with HIIT (7.90±1.85 ml/kg/min; [4.20,11.61]). Despite no changes in body composition, HIIT improved RMR and fat oxidation in men and women, respectively. HIIT also improved cardiorespiratory fitness in both men and women; adaptations may occur more quickly in men, especially with EAA.

(Click here for large version)
Contact: ktrose23@live.unc.edu
Best Poster by a Faculty or Staff Member
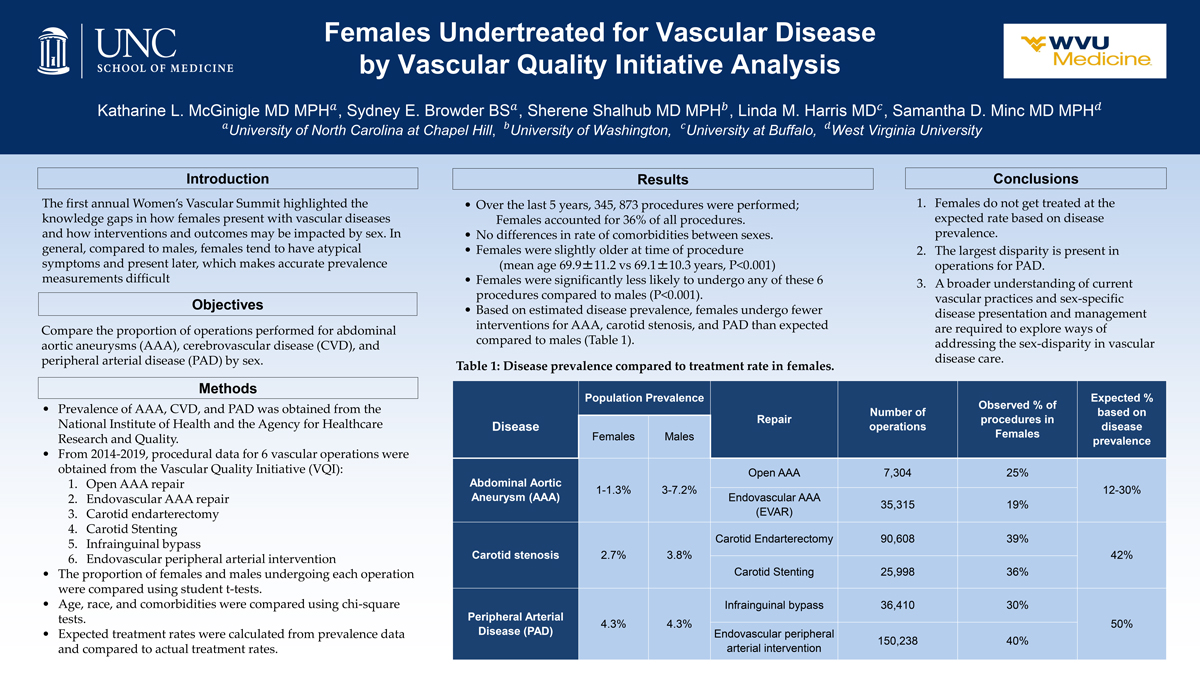
Females Undertreated for Vascular Disease by Vascular Quality Initiative Analysis
Sydney E. Browder, BS
Katharine L. McGinigle MD MPH, Sydney E. Browder BS, Sherene Shalhub MD MPH, Linda M. Harris MD, Samantha D. Minc MD MPH
The first annual Women’s Vascular Summit highlighted the knowledge gaps in how females present with vascular diseases and how interventions and outcomes may be impacted by sex. Compared to males, females tend to have atypical symptoms and present later, making accurate prevalence measurements difficult. We aim to compare the proportion of operations performed for abdominal aortic aneurysms (AAA), cerebrovascular disease (CVD), and peripheral arterial disease (PAD) by sex. Prevalence of AAA, CVD, and PAD was obtained from the National Institute of Health and the Agency for Healthcare Research and Quality data. Procedural data for 6 vascular operations were obtained from the Vascular Quality Initiative (VQI) for the period of 2014-2019: open and endovascular AAA repair, carotid endarterectomy and stenting, infrainguinal bypass, and endovascular peripheral arterial intervention. The proportion of females and males undergoing each operation were compared using student t-tests. Age, race, and comorbidities were compared using chi-square tests. Finally, the expected treatment rates were calculated from prevalence data, and compared to actual treatment rates. Over the last 5 years, a total of 345,873 vascular procedures were performed (36% Female). There were no differences in comorbidities between sexes. Females were significantly less likely to undergo any of these 6 procedures compared to males (P<0.001). Based on estimated disease prevalence, females undergo fewer interventions for AAA, carotid stenosis, and PAD than expected compared to males (Table 1). A broader understanding of current vascular practices and sex-specific disease presentation and management are required to begin addressing the sex-disparity in vascular disease care.
(Click here for large version)
Contact: sydney_browder@med.unc.edu
Poster that Best Demonstrates the Importance of Sex as a Biological Variable
E-Cigarette Exposure Delays Pregnancy and Causes Long-Term Metabolic Effects in Female Offspring
Margeaux Wetendorf, PhD
 Dr. Margeaux Wetendorf received her PhD at Baylor College of Medicine studying under the leadership of Dr. Francesco DeMayo. Her thesis work centered on the role of progesterone signaling in promoting pregnancy and maintaining the healthy uterine state. Through the development and utilization of unique mouse models, she determined how complex hormone signaling mechanisms determine the narrow time in which the embryo implants into the uterus. Dr. Wetendorf experienced the privilege of completing her thesis work at the National Institute of Environmental Health Sciences before joining the laboratory of Dr. Kathleen Caron at UNC in the fall of 2016. In continuing her strong commitment to female reproductive biology, Dr. Wetendorf’s current research focuses on the molecular factors that coordinate the beginning of pregnancy and the subsequent development of a healthy placenta. She also aims to understand how environmental effectors such as plasticizers and phytoestrogens as well as tobacco products including e-cigarettes can affect embryo attachment, placental development, and the progression of pregnancy. Results from her work can help women that experience difficulty becoming pregnant or maintaining a pregnancy. When Dr. Wetendorf is not exploring new scientific ventures above sea level, she enjoys scuba diving the underwater infinite abyss.
Dr. Margeaux Wetendorf received her PhD at Baylor College of Medicine studying under the leadership of Dr. Francesco DeMayo. Her thesis work centered on the role of progesterone signaling in promoting pregnancy and maintaining the healthy uterine state. Through the development and utilization of unique mouse models, she determined how complex hormone signaling mechanisms determine the narrow time in which the embryo implants into the uterus. Dr. Wetendorf experienced the privilege of completing her thesis work at the National Institute of Environmental Health Sciences before joining the laboratory of Dr. Kathleen Caron at UNC in the fall of 2016. In continuing her strong commitment to female reproductive biology, Dr. Wetendorf’s current research focuses on the molecular factors that coordinate the beginning of pregnancy and the subsequent development of a healthy placenta. She also aims to understand how environmental effectors such as plasticizers and phytoestrogens as well as tobacco products including e-cigarettes can affect embryo attachment, placental development, and the progression of pregnancy. Results from her work can help women that experience difficulty becoming pregnant or maintaining a pregnancy. When Dr. Wetendorf is not exploring new scientific ventures above sea level, she enjoys scuba diving the underwater infinite abyss.E-cigarette usage is rampant among reproductive-aged and pregnant women, often perceived as a safe alternative to cigarette smoking, which can impair fetal development. However, the effect of E-cigarettes on pregnancy is currently unknown. The initiation of pregnancy is a complex and highly regulated process that controls the implantation of the embryo at day 4.5 within the mouse. Due to this precision, we hypothesized that exposure to E-cigarette vapor impairs pregnancy initiation and long-term offspring health. To test this, wildtype pregnant mice were exposed to sham or E-cigarette vapor in an exposure chamber 5 times a week. After 4 months, females exposed to E-cigarette vapor exhibited a statistically significant delay in the first pregnancy. Additional mice were mated and treated with E-cigarette vapor or sham on each day of pregnancy until day 4.5 or 5.5. At day 5.5, E-cigarette exposed pregnant animals exhibited an absence of implanted embryos, while sham exposed animals exhibited successful implantation. On day 4.5, uterine tissue was harvested and submitted for transcriptome analysis. E-cigarette exposed uteri exhibited significant changes in the integrin, PI3K/AKT, and chemokine pathways. Additionally, female offspring exposed to E-cigarette vapor in utero exhibited a significant decrease in weight at 8.5 months of age. Adult male offspring exposed to E-cigarette in utero demonstrated no change in weight, but exhibited a mild reduction in reproductive fitness. Thus, E-cigarette exposure delays pregnancy, impairs embryo implantation, and causes long term weight loss in female offspring.

(Click here for large version)
Contact: wetendor@med.unc.edu
2020 Submissions
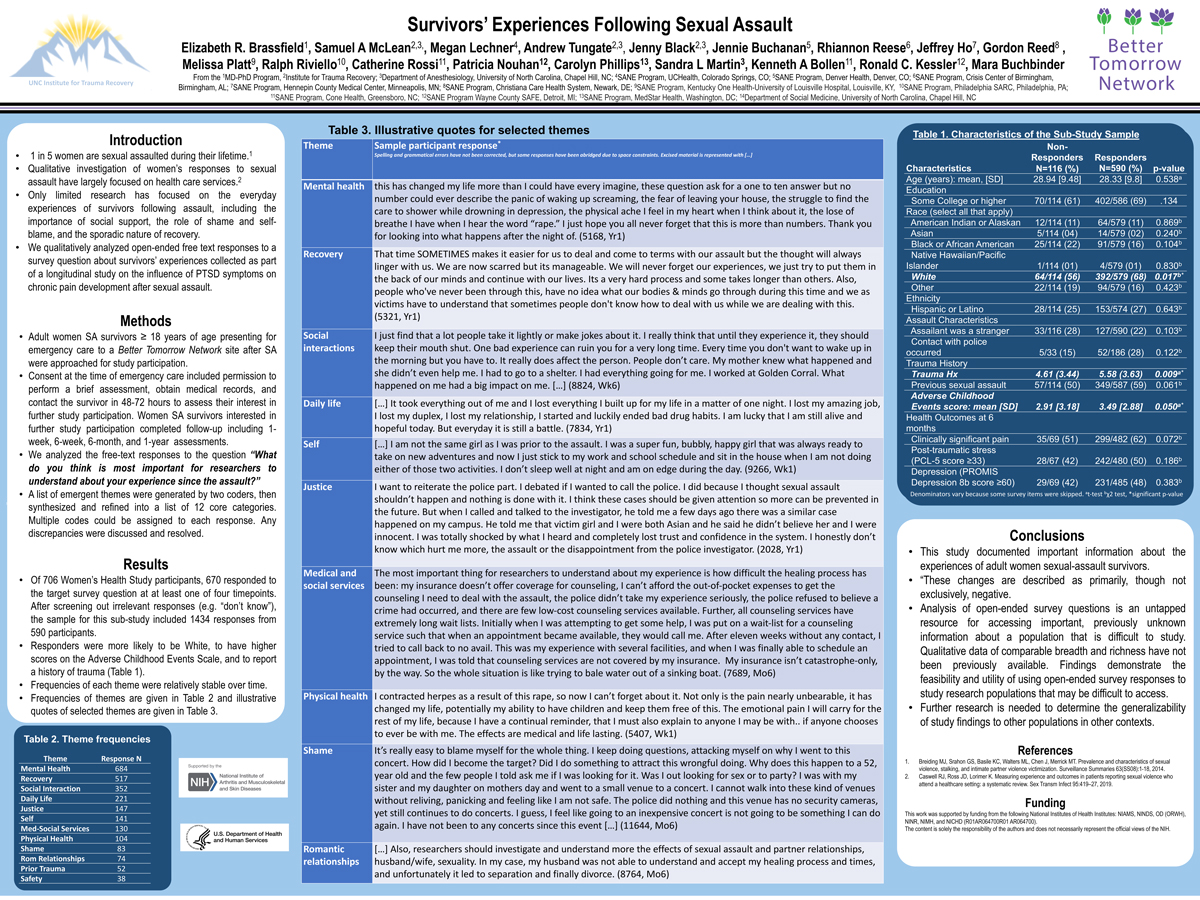
Survivors’ Experiences Following Sexual Assault
Elizabeth R. Brassfield, PhD
Sexual assault is common and has serious health consequences, yet relatively little research has documented the everyday experiences of survivors following assault. Moreover, methodological and ethical concerns about potentially retraumatizing survivors have impeded research progress. The objective of this qualitative analysis of open-ended free text responses was to characterize the issues facing sexual assault survivors in the aftermath of assault. Data were collected as part of a prospective, longitudinal multi-site observational study of the influence of PTSD symptoms on chronic pain development after sexual assault. The parent study included 706 English-speaking women at least 18 years old who presented to a participating site for emergency care within 72 hours of assault. The sub-study sample includes 590 participants who responded to the survey question to the question “What do you think is most important for researchers to understand about your experience since the assault?” at least once out of four survey timepoints. Themes from participants’ 1434 responses fell into twelve broad categories: daily life, justice, medical and social services, mental health, physical health, prior trauma, recovery, romantic relationships, safety, self, shame, and social interactions. Responses demonstrated that the assault permeates many aspects of assault survivors’ daily lives. Overall, responses were overwhelmingly negative, with a smaller number acknowledging that they had recovered or experienced positive changes following the assault. This study documented important information about the experiences of sexual assault survivors across the US. Qualitative data of comparable breadth and richness have not been previously available.
(Click here for large version)
Contact: elizabeth_brassfield@med.unc.edu
A Quality Improvement Project for Care Transitions of Incarcerated Women
Katherine M. Davis, MPH
 Katherine Davis is a fourth-year medical student at the UNC School of Medicine, and recently earned her Master in Public Health from the UNC Gillings School of Global Public Health. As part of her MPH degree, she completed a practicum and master’s paper that assessed current methods of care transitions for incarcerated pregnant women and developed a policy proposal to address gaps in care. Katherine recently matched into residency for Obstetrics and Gynecology, and plans to continue her work with women involved in the criminal justice system in her future career. Her other career interests in women’s health include policy development and advocacy work, health care leadership, and care for underserved populations.
Katherine Davis is a fourth-year medical student at the UNC School of Medicine, and recently earned her Master in Public Health from the UNC Gillings School of Global Public Health. As part of her MPH degree, she completed a practicum and master’s paper that assessed current methods of care transitions for incarcerated pregnant women and developed a policy proposal to address gaps in care. Katherine recently matched into residency for Obstetrics and Gynecology, and plans to continue her work with women involved in the criminal justice system in her future career. Her other career interests in women’s health include policy development and advocacy work, health care leadership, and care for underserved populations.Katherine M. Davis, MPH, Sue Tolleson-Rinehart, PhD, Andrea K. Knittel, MD, PhD
Currently incarcerated pregnant women face significant barriers when they seek health care services within prisons and jails, but little is known about transitions from state prison health care systems to outside hospitals. Our objective was to describe care transitions between institutions and make policy recommendations for improvement. We conducted in-depth interviews with key stakeholders at a state prison, university hospital, and local private hospital to identify the barriers and facilitators to care transitions for incarcerated pregnant women. Stakeholders included medical administrators, physicians, nurses, social workers, care coordinators, and other ancillary staff at the three institutions. We analyzed the interviews using a general inductive approach and developed a policy model based on two existing policy frameworks. Two categories of key themes emerged from the interviews. Operational challenges included transfer of medical records, communication between systems, and education of providers. Structural issues included care of marginalized populations and implicit biases. The resulting policy development model includes environmental structures, policy subsystems, and process implementation and calls for a multipronged approach, focusing on operational barriers to address this issue. Policy changes to improve transitions of care include the addition of a dedicated pregnancy care coordinator and a standardization of a clinician-to-clinician sign-out process. This work has the potential to change the policies that govern care of incarcerated pregnant women, improving care transitions and stimulating the delivery of more effective and efficient health care to this population.

(click here for large version)
Contact: katherine_davis@med.unc.edu
Implementation of Proactive Penicillin Allergy Evaluation in Pregnancy
Nerlyne Desravines, MD
Nerlyne Desravines is clinical fellow in the Department of Obstetrics and Gynecology. She attended medical school at Duke University and completed residency at UNC Chapel Hill in Obstetrics and Gynecology. Dr. Desravines is continuing on to fellowship in Gynecologic Oncology. Her research interests include infectious disease, health disparities, dysplasia and cancer.
Jamie L. Waldron, MD1, Nerlyne Desravines, MD2, Mildred Kwan, MD PhD3, Scott Commins1, MD, Kim Boggess, MD2
1Allergy and Immunology, Departments of Internal Medicine and Pediatrics, University of North Carolina, Chapel Hill
2 Department of Obstetrics and Gynecology, University of North Carolina, Chapel Hill
3Division of Rheumatology, Allergy and Immunology, Department of Medicine, University of North Carolina School of Medicine, Chapel Hill, NC
Rationale
Penicillin (PCN) allergy is commonly reported, but many are erroneously labeled. Pregnancy is associated with high incidence of antibiotic administration; however, drug allergy evaluation is not commonly performed during pregnancy. Pregnant women reporting PCN allergy receive suboptimal antibiotic alternatives for perioperative prophylaxis and group B streptococcus (GBS) infection, a leading cause of neonatal sepsis. Protocols implementing PCN evaluation during prenatal care remain underutilized.
Methods
This was a prospective cohort study of pregnant women between 14-37 weeks gestation with reported PCN allergy who underwent allergy testing in an outpatient Allergy clinic. Testing outcomes were recorded in the medical record and participants continued routine obstetric care. Clinical outcomes included antibiotics administered at delivery.
Results
39 women met inclusion criteria and underwent allergy testing. 89% reported initial reactions in childhood; 71% reported isolated cutaneous symptoms, 16% unknown, 5% “anaphylaxis”. 92% of women tested passed the allergy evaluation. Among those with delivery outcomes, 36% were GBS positive and 36% delivered via Cesarean section. All women who had penicillin allergy removed received beta lactam antibiotics during peripartum course (including perioperative prophylaxis).
Conclusions
Our results suggest that only 6% of pregnant women with reported PNC allergy exhibit true sensitivity. The majority of women tested required antibiotics during peripartum course, suggesting a role for testing antepartum. This pilot study has demonstrated safety of outpatient allergy testing in pregnancy. Implementation of an allergy testing protocol has the potential to improve antibiotic stewardship, decrease exposure to broad spectrum antibiotics and antibiotic resistance, and impact maternal and neonatal outcomes.

(Click here for large version)
Contact: ndesravi@live.unc.edu
Hiding in Plain Sight: An Analysis of Gesture Use in Autistic Females
Jessica E. Goldblum
 Jessie is a second-year graduate student pursing a Ph.D. in Developmental Psychology from the University of North Carolina at Chapel Hill. She is a graduate student research assistant in the Brain and Early Experience Lab and in the Harrop Lab: Early Development in Neurodevelopmental Disorders. Originally from Albuquerque, NM, she completed BAs in Psychology, Art History, and Italian at Emory University. Jessie’s research examines play and social communication in normative and clinical populations. In particular, she is interested in using novel methods like eye tracking to study the development of joint attention and play behaviors. In her spare time, Jessie enjoys spending time with her loved ones and playing with her two pups, Junior and Tallulah.
Jessie is a second-year graduate student pursing a Ph.D. in Developmental Psychology from the University of North Carolina at Chapel Hill. She is a graduate student research assistant in the Brain and Early Experience Lab and in the Harrop Lab: Early Development in Neurodevelopmental Disorders. Originally from Albuquerque, NM, she completed BAs in Psychology, Art History, and Italian at Emory University. Jessie’s research examines play and social communication in normative and clinical populations. In particular, she is interested in using novel methods like eye tracking to study the development of joint attention and play behaviors. In her spare time, Jessie enjoys spending time with her loved ones and playing with her two pups, Junior and Tallulah.A predominantly male syndrome, Autism Spectrum Disorder (ASD) affects one female for every three-to-four males. Autistic girls remain largely understudied; are thought to be underdiagnosed; and are, on average, diagnosed almost a full year later than boys, delaying vital early intervention services. Biological sex differences– such as fewer restricted and repetitive behaviors and more advanced social behaviors exhibited in girls – may serve to “camouflage” girls’ ASD symptomatology, likely contributing to later and underdiagnosis. Camouflaging, or the use of strategies to compensate for and mask autistic characteristics during social interactions, is used by autistic females more often than autistic males. Although this compensatory social strategy may yield short term benefits, it is exhausting and associated with elevated distress and psychopathology. Gesture use – a key form of social and behavioral communication and a core deficit in ASD – has been hypothesized to be another form of behavioral camouflage used by autistic females. In a large sample of autistic females (N=40) and autistic males (N=40) matched on chronological and mental age, we will examine potential sex differences in gesture use and whether gesture use serves as a form of camouflage in autistic females. Utilizing secondary data analysis of the Early Social Communication Scales, we hypothesize that autistic girls will engage in more frequent and higher-skilled gesture use than autistic boys. This study serves to strengthen our understanding of autistic females and the adaptive skills they may use to mitigate some of their challenges, potentially aiding in earlier detection and treatment of the disorder.

(Click here for large version)
Contact: jessgold@unc.edu
Effects of Adiposity Grade and Body Composition on Adjusted Resting Energy Expenditure in Women
Lacey M. Gould
 Lacey is from Clemmons, North Carolina and is currently a master’s student in the Applied Physiology Laboratory under the direction of Dr. Smith-Ryan in the department of Exercise and Sport Science. She completed her undergraduate degree in Exercise Science and Biology at High Point University and hopes to pursue a PhD in exercise physiology following the completion of her master’s degree. Her research interests encompass exercise, nutrition, and the impact of these interventions on metabolism and body composition in both clinical and athletic populations. Optimizing exercise and nutrition can help individuals live healthier and happier lives, which is why Lacey is passionate about this field of research.
Lacey is from Clemmons, North Carolina and is currently a master’s student in the Applied Physiology Laboratory under the direction of Dr. Smith-Ryan in the department of Exercise and Sport Science. She completed her undergraduate degree in Exercise Science and Biology at High Point University and hopes to pursue a PhD in exercise physiology following the completion of her master’s degree. Her research interests encompass exercise, nutrition, and the impact of these interventions on metabolism and body composition in both clinical and athletic populations. Optimizing exercise and nutrition can help individuals live healthier and happier lives, which is why Lacey is passionate about this field of research.Lacey M. Gould1, Gabrielle J. Brewer1, Katie R. Hirsch1, Malia N.M. Blue1, Hannah E. Saylor1, Abbie E. Smith-Ryan1
1Applied Physiology Laboratory, University of North Carolina at Chapel Hill, Chapel Hill, NC 27599
This project aimed to adjust and compare resting energy expenditure (REEa) and contributions of skeletal lean mass (SM) and fat mass (FM) to REEa in women of varying adiposity levels. In 182 women (Mean±SD: Age 24.2±9.1 yrs, Ht 164.6±6.0 cm, Wt 69.0±22.5 kg), REE was measured via indirect calorimetry (REEm); body composition data was obtained from dual-energy X-ray absorptiometry. Tertiles were derived from body fat percent (%fat); Tertile 1 (T1): %fat= 18.5-28.4%; Tertile 2 (T2): %fat= 28.5-33.8%; Tertile 3 (T3): %fat= 34.0-61.0%. To normalize and compare groups, REE was predicted (REEp) to account for differences in FFM and age. REEa was then calculated from REEm, REEp, and mean REEm per tertile. Contributions (mass × metabolic rate, kcal/kg/day) of FM and SM were calculated as percentages of REEa. One-way ANOVAs were conducted. T1 had lower REEa than T2 (mean difference (MD)±SE: -92.5±30.0 kcal/day, p=0.007) and T3 (-318.9±29.5 kcal/day, p=0.001); REEa in T2 was lower than T3 (-226.4±30.0 kcal/day, p=0.001). Energy expenditure attributed to SM in T1 was higher than T3 (MD±SE: 3.2±0.8%, p=0.001). T1 had a lower FM contribution than T3 (MD±SE: -5.1±0.6%, p=0.001); T2 had a lower FM contribution than T3 (MD±SE: -3.9±0.6%, p=0.001). Despite similarities in SM, women with elevated %fat experienced lower SM contribution and higher FM contribution to REEa. As adiposity increases, REE increases; FM may explain more of the variance in REE between women of different levels of adiposity and may need to be accounted for when evaluating metabolic rate, particularly when working with overweight/obese women.

(Click here for large version)
Contact: lmgould@live.unc.edu
Sexual Assault Morbidity in Adult College Women
Lauren R. Gullett
The high risk of sexual assault (SA) faced by female college students is the subject of increasing national attention, but few prospective studies have enrolled college women sexual assault survivors in the immediate aftermath of SA and assessed adverse mental and physical health outcomes over time. Adult women students <25 years old (M=20.8) presenting for emergency care in the immediate aftermath of SA were enrolled. Outcome assessments included evaluation for substantial posttraumatic stress (PCL-5 scores >33), anxious and depressive symptoms (PROMIS >60) and clinically significant new or worsening pain (CSNWP; Δ>2 on an 0-10 NRS) six-weeks and six-months after SA. Study participants (n=151, 71% White, 14% Black, 27% Latina) experienced a high burden of adverse mental and physical health outcomes after SA. Clinically significant PTS symptoms six weeks (79/151(52.3%)) and six months (61/151(40.4%)) after SA were common, as were moderate to severe depressive symptoms at six weeks and six months (68/126(45.0%) and 53/115(46.1%), respectively), and anxiety symptoms at six weeks (80/125(53.0%)) and six months (74/116(49.0%)). It was also found that CSNWP was common at six weeks (88/151(58.3%)) and six months (68/151(45.0%)) post SA. In sum, adverse physical and mental health outcomes are common among women students who are sexually assaulted. Further studies are needed which evaluate longitudinal health, academic, and career outcomes of women students experiencing sexual assault.

(Click here for large version)
Contact: lgullett@live.unc.edu
Impact of Obesity on the Uterine Microbiome in Pre- and Postmenopausal Mice with Endometrial Cancer
Gabrielle Hawkins, MD
Gabrielle Hawkins MD1, Amber N McCoy BS2, Wenchuan Sun MD1, Temitope Keku PhD2, Chunxiao Zhou, MD, PhD1,3, Wendy R Brewster MD PhD1,3, Victoria L Bae-Jump MD PhD1,3
1University of North Carolina at Chapel Hill, Gynecologic Oncology
2University of North Carolina at Chapel Hill, Department of Medicine, Center for Gastrointestinal Biology and Disease;
3University of North Carolina at Chapel Hill, Lineberger Comprehensive Cancer Center
Introduction: Endometrial cancer (EC) is the 4th most common cancer in US women. The rise of EC frequency and mortality is due in part to the obesity epidemic. Obesity is associated with both higher risk of developing and dying from EC. The microbiome is known to play a complex role in the regulation of obesity and cancer, yet the inter-relationship of obesity, the uterine tumor microbiota and EC pathogenesis is unknown, including the potential influence of menopausal status. Thus, we characterized the microbiota of the malignant uterus using pre- and postmenopausal, obese and lean genetically engineered mouse models of endometrioid EC.
Methods: The Lkb1fl/flp53fl/fl mouse is a genetically engineered, pre-clinical model of endometrioid EC. At 3 wks of age, Lkb1fl/flp53fl/fl mice were fed a low fat diet (LFD, 10% calories from fat) versus a high fat diet (HFD, 60% calories from fat) to mimic diet-induced obesity. At 6 wks of age, the right uterine horn was injected with AdenoCre virus to delete Lkb1 and p53 and induce EC. Concurrently, mice either underwent bilateral oophorectomy to induce the postmenopausal state or retained their ovaries to maintain a pre-menopausal status. EC tumors were collected from all mice 12 wks after tumor induction. The microbiota profiles were characterized by bacterial 16S rRNA high throughput sequencing, and the data was analyzed using Qiime2 and MicrobiomeAnalyst.
Results: When analyzed by obesity and menopausal status, we observed significant differences in the EC microbiota composition of Lkb1fl/flp53fl/fl mice at the phylum and genus level. OD1 and TM7 phyla abundance was higher among obese post- versus premenopausal mice (p<0.05). At the genus level, there was a significant increase in the abundance of Delftia (p<0.01) in obese premenopausal mice whereas the abundance of Helicobacter (p=0.01), Oscillospira (p<0.01), Ruminococcus (p<0.01) were increased in obese postmenopausal mice. In lean mice, the phylum level abundance of Proteobacteria (p<0.01) was increased in pre- versus postmenopausal mice. There was also a higher abundance of Delftia (p<0.01) in lean pre- versus postmenopausal mice at the genus level. In postmenopausal mice, the relative abundance of Helicobacter (p=0.02) was increased in obese versus lean mice.
Conclusion: There were distinct differences in the bacterial composition of the ECs in Lkb1fl/flp53fl/fl mice according to obesity and menopausal status, suggesting that the microbiome may play a role in the pathogenesis of obesity-driven EC.

(Click here for large version)
Contact: gabrielle.hawkins@unchealth.unc.edu
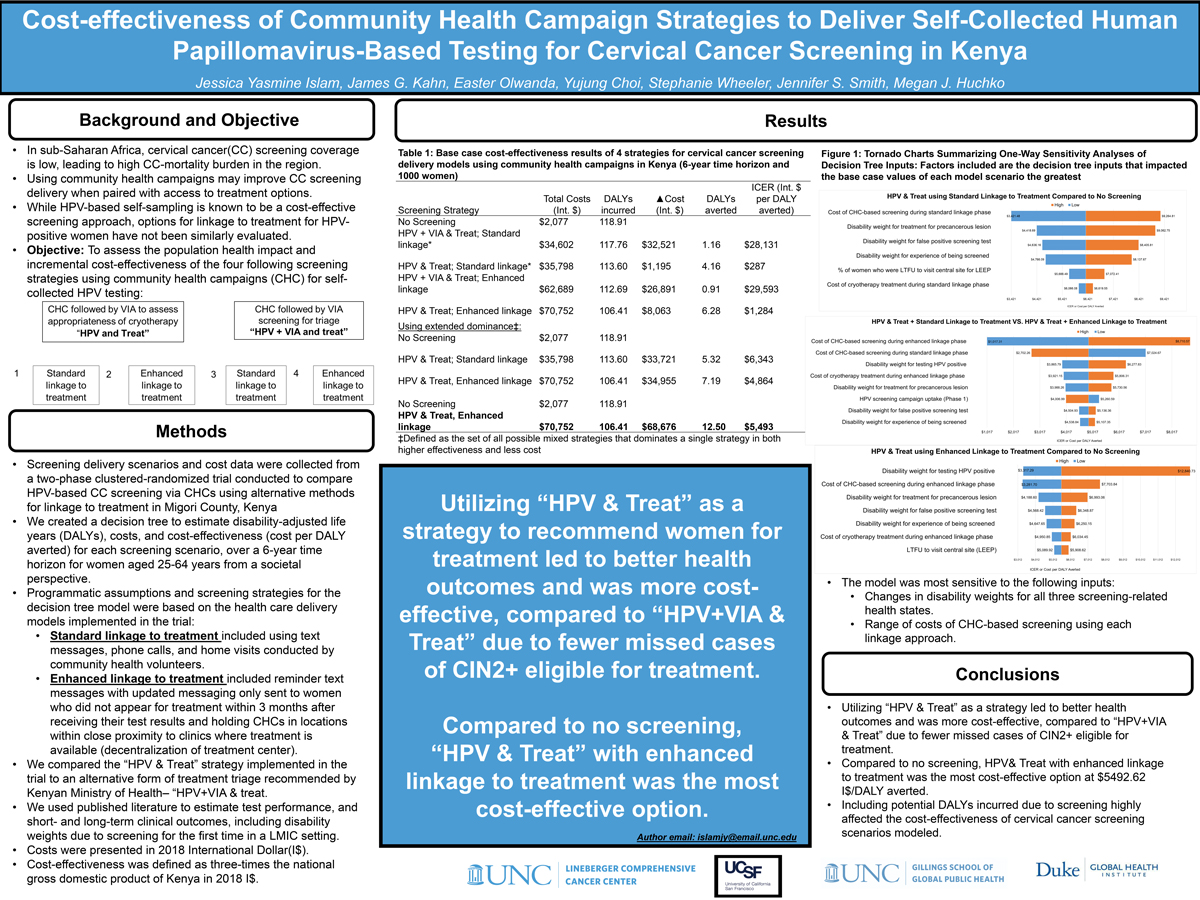
Cost-Effectiveness of Community Health Campaign Strategies to Deliver Self-Collected Human Papillomavirus-Based Testing for Cervical Cancer Screening in Kenya
Jessica Yasmine Islam, PhD, MPH
 Jessica Islam, PhD, MPH is a Post-doctoral fellow on the NIH-funded Cancer Care Quality Training Fellowship through the UNC Lineberger Comprehensive Cancer Center. She is trained in cancer epidemiology and completed her doctoral work at UNC Gillings School of Global Public Health in August 2019. Her research interests include the disparities in the epidemiology of cancer in the US, the prevention of cancers caused by infections globally, and cancer treatment disparities among people living with HIV.
Jessica Islam, PhD, MPH is a Post-doctoral fellow on the NIH-funded Cancer Care Quality Training Fellowship through the UNC Lineberger Comprehensive Cancer Center. She is trained in cancer epidemiology and completed her doctoral work at UNC Gillings School of Global Public Health in August 2019. Her research interests include the disparities in the epidemiology of cancer in the US, the prevention of cancers caused by infections globally, and cancer treatment disparities among people living with HIV.Jessica Yasmine Islam1,2, James G. Kahn3,4, Easter Olwanda5, Yujung Choi6,7, Stephanie Wheeler2,8, Jennifer S. Smith1,2, Megan J. Huchko6,7
1Department of Epidemiology, Gillings School of Global Public Health, University of North Carolina at Chapel Hill, Chapel Hill, NC USA
2Lineberer Comprehensive Cancer Center, University of North Carolina at Chapel Hill, Chapel Hill, NC USA
3Department of Epidemiology and Biostatistics, University of California, San Francisco, CA, USA;
4Philip R. Lee Institute for Health Policy Studies, University of California, San Francisco, San Francisco, CA USA
5Center for Microbiology Research, Kenya Medical Research Institute, Nairobi, Kenya
6Duke Global Health Institute, Duke University, Durham, NC, USA
7Department of Obstetrics and Gynecology, Duke University, Durham, NC, USA
8Department of Health Policy and Management, Gillings
Introduction: In sub-Saharan Africa, cervical cancer(CC) screening coverage is low, leading to high CC-mortality burden in the region. Using community health campaigns(CHCs) may improve CC screening delivery when paired with access to treatment options. While HPV-based self-sampling is known to be a cost-effective screening approach, options for linkage to treatment for HPV-positive women have not been similarly evaluated. Our objective was to evaluate the cost-effectiveness of four CC screening scenarios compared to no screening, each using CHC-based HPV self-sampling: (1) followed by referral for visual assessment and cryotherapy(“HPV-and-treat”), with standard-linkage to treatment and (2)“HPV-and-treat” with enhanced-linkage; and (3) followed by Visual Inspection with Acetic Acid(VIA) triage to cryotherapy(“HPV+VIA-and-treat”), with standard-linkage and (4)“HPV+VIA-and-treat” with enhanced-linkage.
Methods: Screening delivery scenarios and cost data were collected from a two-phase clustered-randomized trial of the scenarios conducted in Migori County, Kenya (2016-2018). We created a decision tree to estimate disability-adjusted life years (DALYs), costs, and cost-effectiveness (cost per DALY averted) for each screening scenario, over a 6-year time horizon for women aged 25-64 years from a societal perspective. We used published literature to estimate test performance, and short- and long-term clinical outcomes. Costs were presented in 2018 International Dollar(I$). Cost-effectiveness was defined as three-times the national gross domestic product of Kenya in 2018 I$.
Results: Compared to no screening, “HPV-and-treat” with enhanced-linkage was the most cost-effective option at $5,492.62 I$/DALY averted. Compared to strategies that used “HPV+VIA-and-treat”, “HPV-and-treat” strategies led to better health outcomes, as measured in DALYs, and were more cost-effective due to fewer missed cases of CIN2+ eligible for treatment. Deterministic sensitivity analyses showed that the proportion of women successfully linked to treatment most impacted the cost-effectiveness of “HPV& treat” options.
Conclusion: CHCs using HPV-based self-collection followed by “HPV-and-treat” with enhanced linkage to treatment appears to be a cost-effective option for Kenya.
(Click here for large version)
Contact: islamjy@email.unc.edu
Optimizing Family Education on the Postpartum Unit
Jennifer Jensen
 Jenny Jensen is a registered nurse and board-certified lactation consultant working at the UNC Women’s Hospital Maternity Care Center. She is also a clinical instructor for the Duke University School of Nursing and Chair of the North Carolina Lactation Consultant’s Association. Prior to her nursing career she was a Foreign Service Officer in the U.S. Department of State, and she served at the U.S. Consulate in Shanghai and the U.S. Embassy in Accra. Jenny has a BSN from Johns Hopkins University and a B.A. in East Asian Studies and Economics from Wellesley College. She completed her research for this poster as part of her studies in a dual Master of Public Health and Master of Science in Nursing program at Johns Hopkins University.
Jenny Jensen is a registered nurse and board-certified lactation consultant working at the UNC Women’s Hospital Maternity Care Center. She is also a clinical instructor for the Duke University School of Nursing and Chair of the North Carolina Lactation Consultant’s Association. Prior to her nursing career she was a Foreign Service Officer in the U.S. Department of State, and she served at the U.S. Consulate in Shanghai and the U.S. Embassy in Accra. Jenny has a BSN from Johns Hopkins University and a B.A. in East Asian Studies and Economics from Wellesley College. She completed her research for this poster as part of her studies in a dual Master of Public Health and Master of Science in Nursing program at Johns Hopkins University.Jensen, J., Tully, K.P., Sweeney, A., Stuebe, A.M., and the Postnatal Patient Safety Learning Laboratory
The United States experiences higher maternal and infant mortality rates than most other OECD nations. Rates of pregnancy-related deaths and morbidity disproportionately impact black mothers and infants, who are three and two times as likely to die as white mothers and infants, respectively. One strategy for reducing postnatal risk for new mothers and their infants is to ensure that new families leave the hospital able to distinguish between typical, concerning, and emergency symptoms so that they can seek appropriate medical care when needed. Inpatient clinicians face a difficult challenge: a family that is presented with too much information during the exhaustion of their hospital stay will not retain it, but a family that receives too little information about this critical transition period could suffer life-threatening consequences. Partners such as fathers or grandmothers are also not nearly as engaged by the healthcare system or utilized as a part of a care team around postpartum health warning signs and supports as they may like. As part of an ongoing Agency for Healthcare Research and Quality funded Patient Safety Learning Laboratory to understand and advance postpartum care, a literature review was conducted of clinical guidelines, including recommendations for in-patient teaching. Those recommendations were prioritized based on prevalence and impact in the postpartum patient population to assist clinicians in identifying the topics to prioritize. Lastly, recommendations were made regarding best practices in discharge teaching, assessment of comprehension, and resource connection including teach-back, handouts, and utilization of interpreters and technology as needed.

(Click here for large version)
Contact: jennyjensenrn@gmail.com
Diet-induced Obesity Aggravates Preeclampsia-like Phenotypes in ASB4-null Mice
Feng Li
Feng Li1, Neeta Vora2, Kim Boggess2, Nobuyo Maeda-Smithies1
1Department of Pathology and Laboratory Medicine 2Department of Obstetrics and Gynecology, Division of Maternal Fetal Medicine University of North Carolina – Chapel Hill
In the past three decades, the incidence of preeclampsia, pregnancy related hypertension, proteinuria and end organ damage, has significantly increased in the U.S., in association with an increase in maternal weight. There is a gap in our understanding regarding how obesity influences preeclampsia. The effects of high fat diets on preeclampsia in animal studies are inconsistent among different research groups. Ankiryn-repeat-and-SOCS-box-containing-protein 4 (ASB4) contributes to the differentiation of trophoblast stem cells into the giant trophoblast cells necessary for embryo implantation in mice. ASB4-null females develop preeclampsia-like phenotypes during pregnancy. We hypothesized that obesity induced by a high-fat diet would worsen the preeclampsia-like phenotypes in ASB4-null pregnant mice. ASB4-null females were assigned to either a high-fat diet (HF) or normal chow (NC) group at age of 3-4 weeks. At age of 8-9 weeks they were mated with ASB4-null males and the outcomes of pregnancy were determined at 18.5 day post coitus (dpc). Compared to ASB4-null pregnant mice on NC, the mice fed HF have more visceral fat, higher plasma lipid, decreased number of surviving fetuses, higher blood pressure, and more severely impaired kidney function and structure.
The impaired lipid metabolism resulting from a HF diet may lead to the aggravated maternal and fetal phenotypes of preeclampsia in ASB4-null pregnant mice. Interrogation of maternal lipid metabolism in preeclampsia may reveal novel pathways to target for prevention.

(Click here for large version)
Contact: lif@med.unc.edu
Changes in Monocyte Function in Response to Acute Exercise in Breast Cancer Survivors
Kaileigh M. Moertl
 Kaileigh Moertl is originally from Palatine, Illinois, but comes to UNC-CH from Chicago, Illinois. She is a graduate of North Park University where she played softball and earned her B.S. in Exercise Science. She is thrilled to be pursuing her Masters in Exercise Physiology here at Carolina and plans to earn her Ph.D. as well. Kaileigh hopes to pursue a career in clinical research, working and advocating within the field of exercise oncology and immunology. She is passionate about helping people dealing with chronic illness and how exercise can play a vital role in the immune system. She is spending her two years here under the mentorship of Dr. Erik Hanson in the Exercise Oncology Research Lab. Kaileigh is glad to have the opportunity to be a part of the research community and is especially happy to live in a state full of trees, mountains, sunshine, and tolerable winters.
Kaileigh Moertl is originally from Palatine, Illinois, but comes to UNC-CH from Chicago, Illinois. She is a graduate of North Park University where she played softball and earned her B.S. in Exercise Science. She is thrilled to be pursuing her Masters in Exercise Physiology here at Carolina and plans to earn her Ph.D. as well. Kaileigh hopes to pursue a career in clinical research, working and advocating within the field of exercise oncology and immunology. She is passionate about helping people dealing with chronic illness and how exercise can play a vital role in the immune system. She is spending her two years here under the mentorship of Dr. Erik Hanson in the Exercise Oncology Research Lab. Kaileigh is glad to have the opportunity to be a part of the research community and is especially happy to live in a state full of trees, mountains, sunshine, and tolerable winters.Kaileigh M. Moertl1, David B. Bartlett2, William S. Evans1, Jordan T. Lee1, Eli Danson1, Chad W. Wagoner1, Elizabeth P. Harrell1, Stephanie A. Sullivan1, Lauren C. Bates1, Brian C. Jensen1, Kirsten A. Nyrop1, Hyman B. Muss1, Claudio L. Battaglini, FACSM1, Erik D. Hanson1.
1University of North Carolina at Chapel Hill, Chapel Hill, NC. 2Duke University, Durham, NCB.
BACKGROUND: The effects of acute exercise on immunity following breast cancer therapy are not well understood. PURPOSE: To determine the response of monocyte function following acute exercise in breast cancer survivors.
METHODS: 9 breast cancer survivors [Age: 58±8y, BMI: 27.9±6.7] completed a cardiopulmonary exercise test (CPET). In a subsequent trial, 45 minutes of intermittent cycling at 60% of CPET peak wattage was performed. Blood was taken at rest, immediately post (0h), and 1h post-exercise. Phagocytosis and oxidative burst were assessed following E.coli exposure. Toll-like receptor 2 (TLR2) and 4 (TLR4) expression was determined on CD14+CD16– and CD14+CD16+ monocytes. All assays were analyzed using flow cytometry and are presented as mean fluorescence intensity (MFI) ± SD.
RESULTS: Phagocytosis increased by 13.4% 1 hour after completion of exercise (0h: 3257±772, 1h: 3692±824, p=0.035), while oxidative burst was unchanged. TLR2 expression progressively decreased from rest on both subsets of monocytes (rest: 345±48, 0h: 317±69, 1h: 283±41, all p<0.01). TLR4 expression on CD16– monocytes decreased by 12.5% from rest to 1 hour post-exercise (rest: 98±14, 1h: 86±11, p=0.009), while TLR4 expression on CD16+ monocytes decreased across all time points (rest: 142±20, 0h: 134±16, 1h: 125±17, all p<0.05).
CONCLUSIONS: In breast cancer survivors, monocyte phagocytic capacity of bacteria increased following acute exercise, while expression of TLR2 and TLR4 was progressively reduced. The reduction of TLR2 and TLR4 on monocytes may represent an anti-inflammatory response of acute exercise which promotes enhanced elimination of bacteria. Supported by the Breast Cancer Research Foundation of New York.

(Click here for large version)
Contact: kmoertl@live.unc.edu
Central Pulse Wave Velocity in Neonates: Feasibility and Comparison to Normative Data
Patricia Pagan Lassalle
 Patricia Pagan Lassalle is a native of Guaynabo, Puerto Rico. She completed her B.S. and M.S. in Exercise Science at Syracuse University and is currently a first year PhD student in the Human Movement Science curriculum at UNC Chapel Hill. Her research interests include evaluating cardiometabolic health and the influence of racial/ethnic differences and lifestyle behaviors on onset and prevalence of cardiometabolic disease across the lifespan with a particular focus in young adults. Her current professional goals include understanding the disproportionate burden of disease in specific minority groups and improving female and minority representation in higher education through mentoring. Her future professional goals involve pursuing an M.D./Ph.D. in Exercise Physiology.
Patricia Pagan Lassalle is a native of Guaynabo, Puerto Rico. She completed her B.S. and M.S. in Exercise Science at Syracuse University and is currently a first year PhD student in the Human Movement Science curriculum at UNC Chapel Hill. Her research interests include evaluating cardiometabolic health and the influence of racial/ethnic differences and lifestyle behaviors on onset and prevalence of cardiometabolic disease across the lifespan with a particular focus in young adults. Her current professional goals include understanding the disproportionate burden of disease in specific minority groups and improving female and minority representation in higher education through mentoring. Her future professional goals involve pursuing an M.D./Ph.D. in Exercise Physiology.Patricia Pagan Lassalle1, Michelle L. Meyer1, Kim A. Boggess1, and Lee Stoner1
1University of North Carolina at Chapel Hill, Chapel Hill, NC
BACKGROUND: Carotid-femoral pulse wave velocity (cfPWV) is used for noninvasively assessing vascular aging and cardiovascular disease (CVD) risk trajectories. However, no normative cfPWV data in children exist, and cfPWV is unsuitable for tracking CVD risk in neonates.
PURPOSE: (a) Use meta-regression to determine normal progression of cfPWV in children, and (b) determine the feasibility of assessing brachial-femoral PWV (bfPWV) in neonates. We hypothesized that (a) cfPWV will increase with age, starting at birth, and (b) mean bfPWV values in neonates will overlap with the intercept (year 0) from the normative data generated from the meta-regression.
METHODS: Electronic databases were searched from inception to May 2018 for all studies that reported cfPWV in children (<19 y). Random effects meta-regression was used to quantify the association between time (years) and cfPWV. bfPWV in 5 neonates (1-2 days old; mean weight 3.65 kg [SD: 0.52]) was assessed using oscillometric cuffs, attached to the upper right arm and thigh, via the VICORDER™.
RESULTS: (a) Meta-regression findings (9 studies): cfPWV increase per year (age) was 0.12 (95%CI: 0.07, 0.16) m/s. The cfPWV intercept (0 y) was 3.61 (95%CI: 3.07, 4.16) m/s. (b) bfPWV was successfully collected in all neonates with a mean of 3.64 (95%CI: 3.31, 3.97) m/s.
CONCLUSION: PWV increases from birth at a rate of 0.12 m/s. Mean bfPWV from the neonates overlapped with the intercept from the cfPWV meta-regression analysis, and may be a suitable technique for tracking CVD risk beginning in the neonatal period.
FUNDING: NIH Building Interdisciplinary Research Careers in Women’s Health (5K12HD001441).

(Click here for large version)
Contact: ppagan@unc.edu
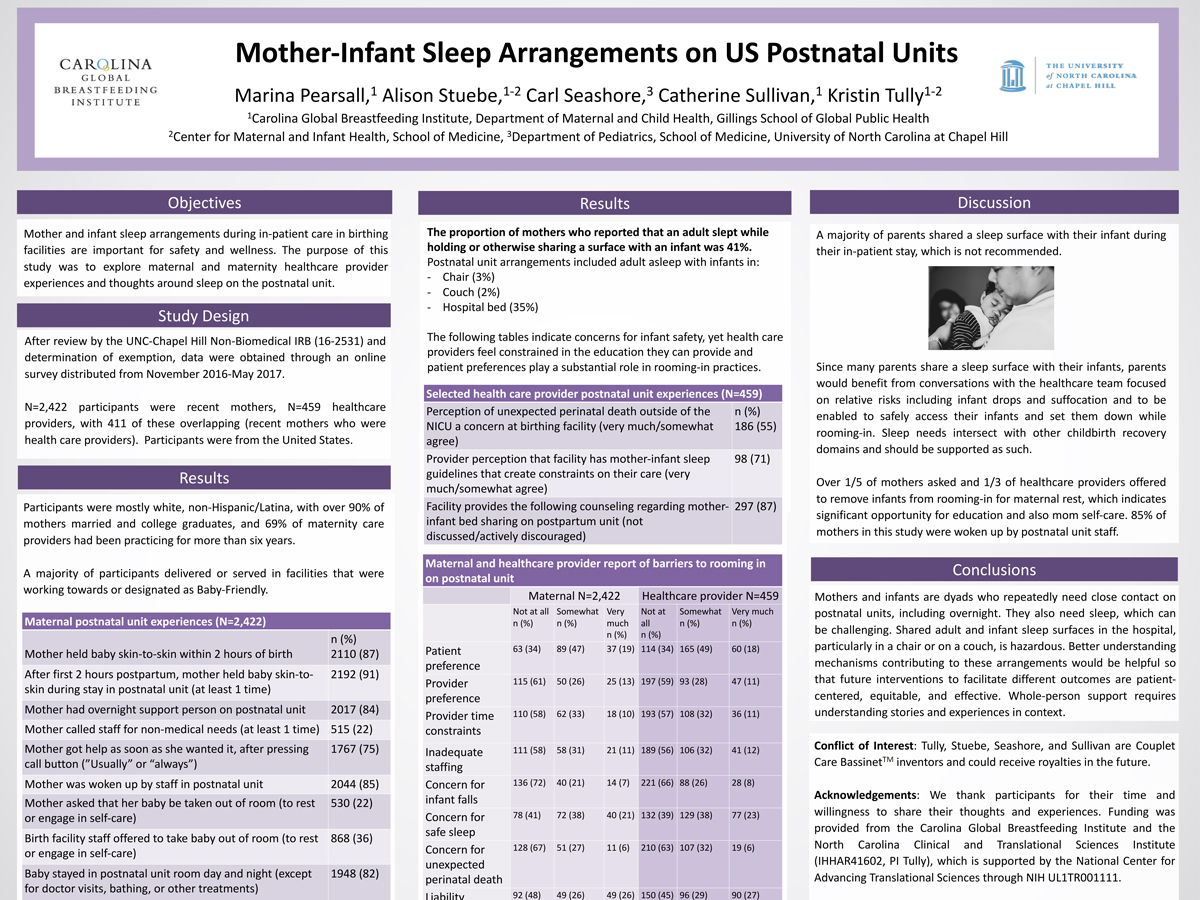
Mother-Infant Sleep Arrangements on US Postnatal Units
Marina Pearsall, MPH, RDN, LDN
Marina Pearsall, Alison Stuebe, Carl Seashore, Catherine Sullivan, Kristin Tully
Mother and infant sleep arrangements during in-patient care in birthing facilities are important for safety and wellness. The purpose of this study was to explore maternal and maternity health care provider experiences and thoughts around sleep on the postnatal unit. Of the total sample of 3,610 collected during 2016-2017, two sub-groups of mothers (n=2,422) and providers (n=459) were included in this analysis. Participants were mostly white, non-Hispanic/Latina, with over 90% of mothers married and college graduates, and 69% of maternity care providers had been practicing for more than six years (69%). A majority of participants delivered or served in facilities that were working towards or designated as Baby-Friendly. The rate of continuous rooming-in in this sample was 82%, as reported by mothers, except for doctor visits, bathing, or other treatments. Shared sleep surface among caregivers and their newborns at some point during in-patient care was common (41%), and the arrangements included the adult asleep with infants in a chair (3%) or on a couch (2%), or in the bed (35%). A majority intended to sleep in the reported arrangement (53%). Additionally, both mothers and health care providers reported on barriers to rooming-in on the postnatal unit, including liability, safe sleep concerns, and provider or patient preference. Most (70%) providers in our sample indicated that they “somewhat agree” or “very much agree” that they feel constrained by recommendations on the care they would like to offer. The mechanisms through which parent-infant sleep arrangements on the postnatal unit are planned and experienced warrant further investigation and support.
(Click here for large version)
Contact: mpear@live.unc.edu
Increased Posttraumatic Stress Symptoms are Associated with Increased Substance Abuse in Sexual Assault Survivors During the Year After Sexual Assault
Heather Swain, BS
 Heather obtained her B.S. in Psychology from UNC in 2019, and is an incoming medical student at UNC School of Medicine for Fall 2020. She has worked with the Institute for Trauma Recovery, a research branch of UNC Department of Anesthesiology, for almost 4 years. During her time as an undergraduate, she worked as a volunteer and student employee for the Women’s Health Study, a recently concluded multi-site study for women following sexual assault. It is this study from which her work on this poster comes. As a full-time employee with the Institute, Heather now works on the AURORA Study. She is grateful to have worked on such important work with the Institute for Trauma Recovery with trauma survivors, and excited to share the initial results of these important data.
Heather obtained her B.S. in Psychology from UNC in 2019, and is an incoming medical student at UNC School of Medicine for Fall 2020. She has worked with the Institute for Trauma Recovery, a research branch of UNC Department of Anesthesiology, for almost 4 years. During her time as an undergraduate, she worked as a volunteer and student employee for the Women’s Health Study, a recently concluded multi-site study for women following sexual assault. It is this study from which her work on this poster comes. As a full-time employee with the Institute, Heather now works on the AURORA Study. She is grateful to have worked on such important work with the Institute for Trauma Recovery with trauma survivors, and excited to share the initial results of these important data.Adult women who present for emergency care after sexual assault (SA) are often socioeconomically disadvantaged, with limited access to mental health services. Posttraumatic stress (PTS) symptoms are common in SA survivors, and in community-based studies of SA survivors have been associated with chemical coping and substance use. Women SA survivors ≥ 18 years of age who presented for emergency care within 72 hours of SA were enrolled into a large multisite study. Follow-up evaluations six weeks, six months, and one year after SA included assessment of PTS symptoms (PCL-5) and alcohol, cannabis, and prescription pain reliever (Rx_Pain) using CIDI-SC. Regression analyses evaluated cross-sectional relationships between PTS and substance use after SA. Among SA survivors (n = 706, mean age (SD) = 29 (10)), PTS symptoms were associated with cannabis and Rx_Pain use at six weeks, and alcohol, cannabis, and Rx_Pain at six months and one year. Many associations between PTS and substance use persisted after adjustment for age, income, and education (e.g., cannabis at six months and one year (ß = 7.2, p < 0.001) and ß = 5.4, p = 0.009, respectively, Rx_Pain one year ß = 16.8, p < 0.001). Complete and updated bivariate and multivariate associations, and cross-lagged analyses evaluating causal relationships using the final study dataset (follow-up completed March 2020) will be presented at the conference. These findings indicate that among women presenting for emergency care after SA, PTS symptoms during the year after SA are associated with increased substance use.

(Click here for large version)
Contact: heather_swain@med.unc.edu
Social Determinants of Health in Maternity Care
Kristin Tully, PhD
Dr. Tully is a Research Associate with the Center for Maternal and Infant Health at the UNC School of Medicine. Additionally, she is a research partner and collaborator with the Carolina Global Breastfeeding Institute in the Department of Maternal and Child Health in the UNC Gillings School of Global Public Health. She is part of the “4th Trimester Project” which is transforming care for new mothers and their families.
Pregnancy, birth, and new family life is a time of immense change and impact. This part of the life course is especially complex for those in conditions of poverty, situated in health deserts, experiencing racism, and for non-English speakers. Social Determinants of Health (SDoH) is defined by the WHO as “the conditions in which people are born, grow, work, live, and age, and the wider set of forces and systems shaping the conditions of daily life.” SDoH are the primary drivers of health outcomes, including sources of strengths. Although called for, SDoH screening and resource provision have not been systematically incorporated into maternity care. The purpose of this research was to provide more understanding of and offer potential solutions for these unmet needs. During 2019-20, we engaged patients and those serving them in a human-centered design project that involved clinical shadowing, interviews, and workshops to determine priorities and we conducted PDSA cycles to test implementation of new recommendations. We heard the need to lead with resources. Transparency in the purpose of the questions and what truthful responses might mean are foundational for honest engagement. SDoH is agreed as within scope and desired as part of routine, periodic screening for everyone as a part of other health assessments. Patients decide how much they want to share and what resources they chose to utilize. Screening cannot be – or be perceived to be – about surveillance. Further, use of interpreters is not always employed when indicated and some discussed experiencing racism in their care.

(Click here for large version)
Contact: kristin.tully@unc.edu