2021 Program
2021 Award Recipients
Best Poster by a Graduate Student
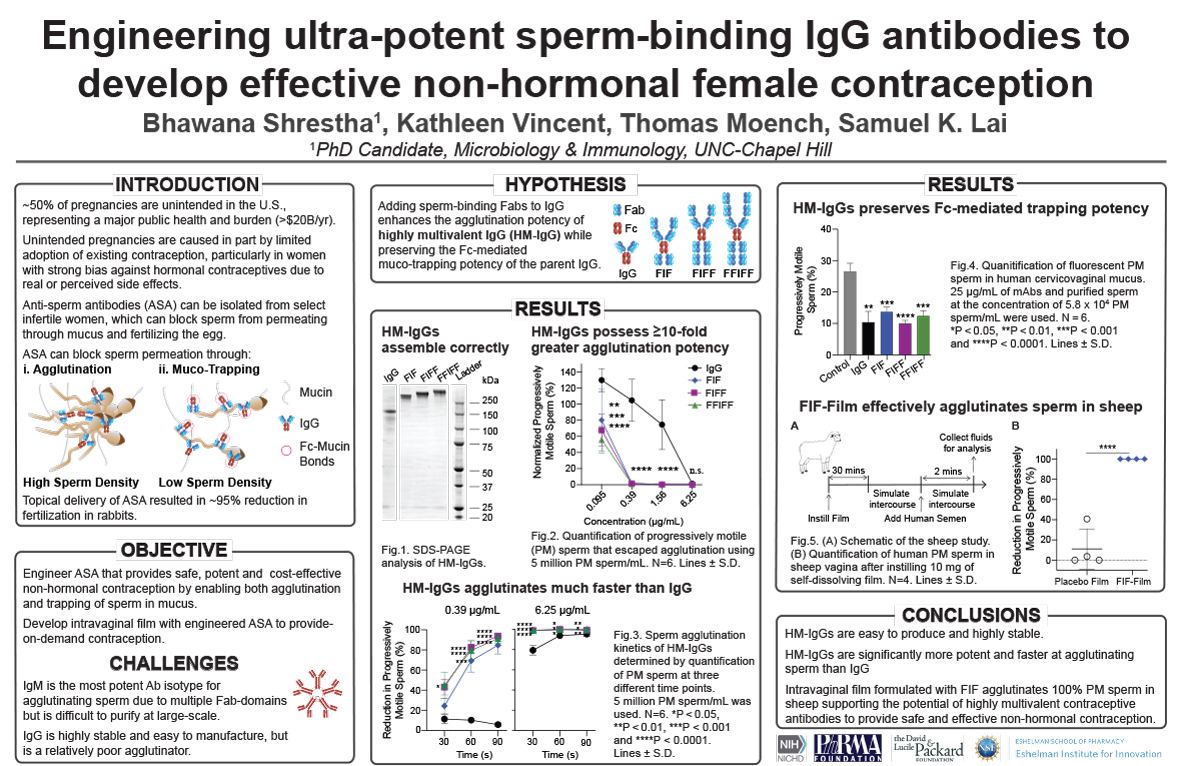
Engineering Ultra-Potent Sperm-Binding IgG Antibodies to Develop Effective Non-Hormonal Female Contraception
Bhawana Shrestha, PhD
 Dr. Bhawana “Suruchi” Shrestha recently received her Ph.D. in Microbiology and Immunology from the University of North Carolina at Chapel Hill under the mentorship of Dr. Samuel K. Lai. Her thesis work focused on engineering highly potent multivalent sperm-binding antibodies to develop much-needed non-hormonal contraceptives for women. Her panel of sperm-binding antibodies effectively agglutinated all progressively motile human sperm in the sheep-vaginal model using just tens of micrograms of antibodies. The lead multivalent sperm-binding antibody was formulated into a water-soluble contraceptive film, which resulted in the complete elimination of all progressively motile human sperm within 2 mins in the sheep vagina. Her work directly enabled a new strategy for potent, cost-effective, and safe non-hormonal contraception that is available on-demand, meeting the contraceptive needs of millions of women. Additionally, her work represents a promising platform for generating potent agglutinating antibodies for diverse medical applications such as antibacterial therapeutics. When Dr. Shrestha is not designing unique next-generation antibodies, she enjoys binge-watching TV shows and attending electronic music concerts.
Dr. Bhawana “Suruchi” Shrestha recently received her Ph.D. in Microbiology and Immunology from the University of North Carolina at Chapel Hill under the mentorship of Dr. Samuel K. Lai. Her thesis work focused on engineering highly potent multivalent sperm-binding antibodies to develop much-needed non-hormonal contraceptives for women. Her panel of sperm-binding antibodies effectively agglutinated all progressively motile human sperm in the sheep-vaginal model using just tens of micrograms of antibodies. The lead multivalent sperm-binding antibody was formulated into a water-soluble contraceptive film, which resulted in the complete elimination of all progressively motile human sperm within 2 mins in the sheep vagina. Her work directly enabled a new strategy for potent, cost-effective, and safe non-hormonal contraception that is available on-demand, meeting the contraceptive needs of millions of women. Additionally, her work represents a promising platform for generating potent agglutinating antibodies for diverse medical applications such as antibacterial therapeutics. When Dr. Shrestha is not designing unique next-generation antibodies, she enjoys binge-watching TV shows and attending electronic music concerts.
Engineering Ultra-Potent Sperm-Binding IgG Antibodies to Develop Effective Non-Hormonal Female Contraception
Millions of women risk unintended pregnancies every year due to dissatisfaction with or medical contraindications to available hormonal contraceptive methods. Naturally occurring sperm-binding antibodies prevents fertilization in immune infertile women by trapping motile sperm in mucus through agglutination and mucin-crosslinking, thereby preventing sperm from reaching the egg. This led us to pursue direct vaginal delivery of sperm-binding monoclonal antibodies as a strategy for effective non-hormonal contraception. Here, we engineered a panel of ultra-potent sperm-binding IgGs possessing 6-10 Fabs against a unique surface antigen universally present on human sperm. These highly multivalent IgGs (HM-IgGs) are at least 10- to 16- fold more potent and faster at agglutinating sperm than the parent IgG, while preserving Fc-mediated crosslinking of individual spermatozoa in mucus. The increased potencies translate to effective (>99.9%) reduction of progressively motile sperm in the sheep vagina using just 33 micrograms of the 10-Fab HM-IgG per sheep. We created a vaginal film formulation of HM-IgGs manufactured using cGMP-compliant processes, which enabled complete agglutination of all progressively motile sperm within 2 mins in the sheep vagina. These results strongly underscore a potential first-in-class non-hormonal contraception that could be highly effective in humans, are exceptionally safe, and only costs pennies per day due to the exceptional potency.
(Click here for large version)
Contact: bhawana@email.unc.edu
Best Poster by a Resident or Fellow
Trends in Initiation and Continuation of Long-acting Reversible Contraception among Female Adolescents in North Carolina
Bianca Allison, MD, MPH
 Dr. Allison is from Syracuse, NY. She received her undergraduate degree in Social Anthropology from Harvard University and spent a service year as a tutor and mentor for middle schoolers through AmeriCorps’ City Year in Chicago, IL. She then received her medical degree from the University of Michigan, and an MPH degree from the Harvard University T.H. Chan School of Public Health. She completed her pediatric residency training here at UNC, and is now in her second and last year of the UNC NRSA Primary Care Research Fellowship. This summer she will be transitioning to an Assistant Professor position within the General Pediatrics and Adolescent Medicine division in the Department of Pediatrics.
Dr. Allison is from Syracuse, NY. She received her undergraduate degree in Social Anthropology from Harvard University and spent a service year as a tutor and mentor for middle schoolers through AmeriCorps’ City Year in Chicago, IL. She then received her medical degree from the University of Michigan, and an MPH degree from the Harvard University T.H. Chan School of Public Health. She completed her pediatric residency training here at UNC, and is now in her second and last year of the UNC NRSA Primary Care Research Fellowship. This summer she will be transitioning to an Assistant Professor position within the General Pediatrics and Adolescent Medicine division in the Department of Pediatrics.
Trends in initiation and continuation of long-acting reversible contraception among female adolescents in North Carolina
Despite high North Carolina (N.C.) adolescent birth rates, with persistent geographic and racial disparities, there is no literature on long-acting reversible contraception (LARC) initiation and continuation in N.C. adolescents. This study examined statewide rates, and associated patient and provider factors, of adolescent (13-18 years) LARC use. We conducted a retrospective cohort study of N.C. Medicaid data from 2013-2018. During the study period, 33,847 (9.0%) adolescents used LARC [i.e., subdermal implants or intrauterine devices (IUDs)] with a mean age of 17.4 years. LARC-using adolescents were more often non-Hispanic, non-White, and lived in rural regions (all p<0.001). LARC was frequently placed by OBGYNs (64%), providers in rural regions (40%), and in outpatient clinics (75%) (all p<0.001). When looking at continuation, younger adolescents had higher continuation of implants (HR 0.90 for 14–16-year-olds, and 0.56 for 17–19-year-olds, compared to 13–14-year-olds; p<0.001) though similar for IUDs (p=0.5 and 0.2 respectively). Black adolescents had higher continuation of IUDs (HR 0.91, p<0.001) though similar for implants (p=0.3). Rural adolescent had higher discontinuation for both IUD and implant compared to urban adolescents (HR 1.24 and HR 1.14, respectively, both p<0.001). Our study found that adolescent females at highest risk for unintended pregnancies (i.e., older adolescents, racial minorities, and those living in rural counties) more commonly initiated LARC; however older and rural adolescents were less likely to continue LARC. Black adolescents more often continued LARC; further research is needed to understand the roles of patient choice, inadequate healthcare access for removal, or reproductive coercion from providers.
(Click here for large version)
Contact: bianca.allison@unchealth.unc.edu
Best Poster by Faculty or Staff
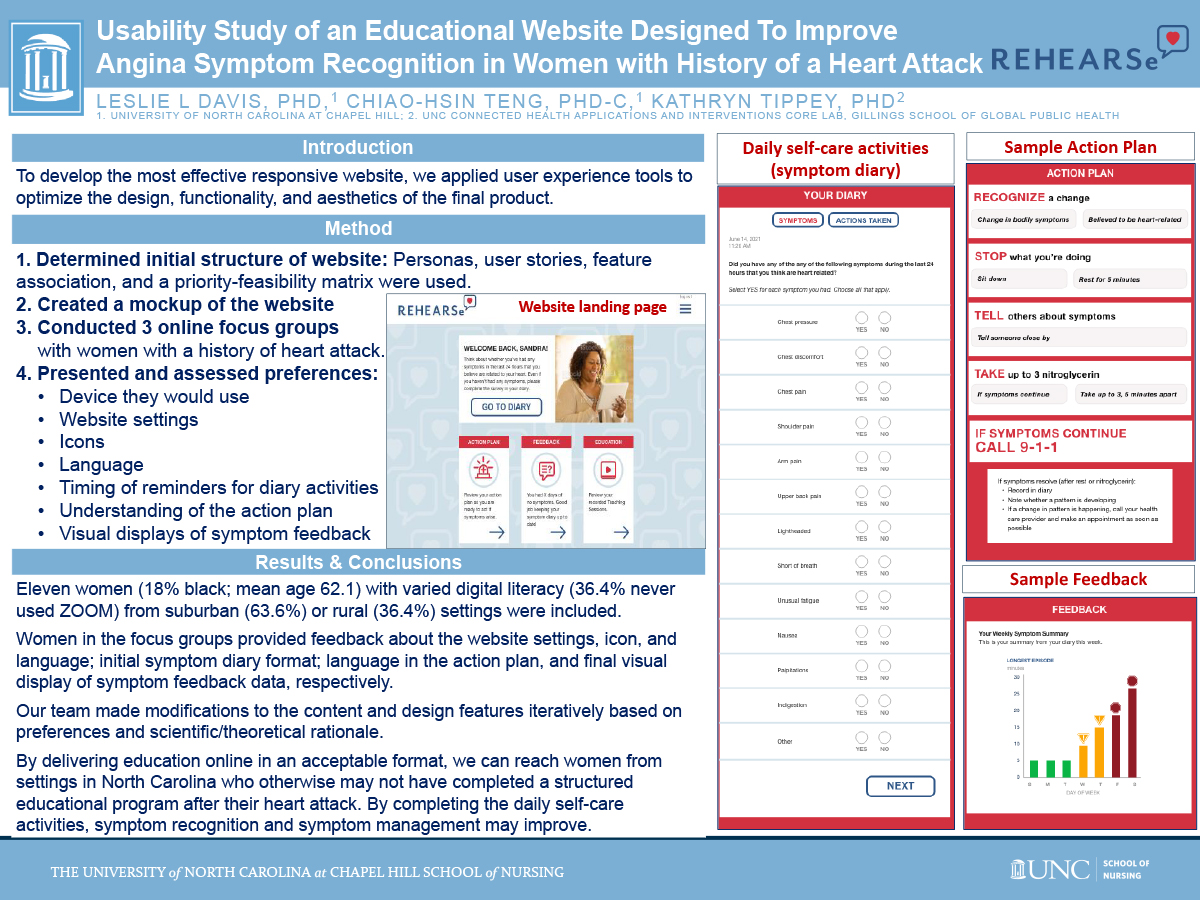
Usability Study of an Educational Website Designed to Improve Angina Symptom Recognition in Women with History of Heart Attack
Leslie L Davis, PhD
 Dr. Leslie Davis is an Associate Professor of the School of Nursing at the University of North Carolina (UNC) at Chapel Hill where in addition to conducting research she teaches in the graduate nursing program and maintains a part-time nurse practitioner practice with the Division of Cardiology. Dr. Davis is a fellow in the American College of Cardiology (ACC), the American Association of Nurse Practitioners, the American Heart Association, and the Preventive Cardiovascular Nurses Association. She is also a certified hypertension clinician through the American Society of Hypertension. As a clinician, she cares for adults with heart failure, hypertension, and heart disease. Her research interests include self-care and symptom management with women who have cardiovascular conditions. Currently, she is testing an individualized education and skill-building intervention to improve symptom recognition, interpretation, and care-seeking behavior in those hospitalized for a heart attack. Dr. Davis is an Associate Editor for the Journal for Nurse Practitioners where she also served as guest editor for two special cardiovascular editions (2013; 2019). In addition to editing her own book, Cardiovascular Nursing Secrets (2004), she has authored/coauthored 40 papers in peer-reviewed journals including three ACC expert consensus documents, 12 book chapters, and other scholarly products. Dr. Davis has participated as an invited expert in Heart House Roundtables and served as faculty and chair of work groups and various CME events on heart-related topics. Dr. Davis will be awarded the 2021 Distinguished Associate Award by the ACC in May of this year.
Dr. Leslie Davis is an Associate Professor of the School of Nursing at the University of North Carolina (UNC) at Chapel Hill where in addition to conducting research she teaches in the graduate nursing program and maintains a part-time nurse practitioner practice with the Division of Cardiology. Dr. Davis is a fellow in the American College of Cardiology (ACC), the American Association of Nurse Practitioners, the American Heart Association, and the Preventive Cardiovascular Nurses Association. She is also a certified hypertension clinician through the American Society of Hypertension. As a clinician, she cares for adults with heart failure, hypertension, and heart disease. Her research interests include self-care and symptom management with women who have cardiovascular conditions. Currently, she is testing an individualized education and skill-building intervention to improve symptom recognition, interpretation, and care-seeking behavior in those hospitalized for a heart attack. Dr. Davis is an Associate Editor for the Journal for Nurse Practitioners where she also served as guest editor for two special cardiovascular editions (2013; 2019). In addition to editing her own book, Cardiovascular Nursing Secrets (2004), she has authored/coauthored 40 papers in peer-reviewed journals including three ACC expert consensus documents, 12 book chapters, and other scholarly products. Dr. Davis has participated as an invited expert in Heart House Roundtables and served as faculty and chair of work groups and various CME events on heart-related topics. Dr. Davis will be awarded the 2021 Distinguished Associate Award by the ACC in May of this year.
Usability Study of an Educational Website Designed To Improve Angina Symptom Recognition in Women with History of Heart Attack
Leslie L Davis, PhD,1 Chiao-Hsin Teng, PhD student,1 Kathryn Tippey, PhD2
1. UNC-CH School of Nursing; 2. Digital Project Manager, UNC Connected Health Applications and Interventions Core Lab, Gillings School of Global Public Health
A previously tested in-person educational intervention designed to improve cardiac symptom recognition in women is being converted to a digital format to make the intervention accessible to more women. To develop the most effective form of a responsive website we applied user experience tools to optimize the design, functionality, and aesthetics of the final product. We used personas, user stories, feature association, and a priority-feasibility matrix to determine the initial website structure and created a mockup of the website that applied this structure. We iterated on the design of the mockups by conducting online focus groups with women with a history of heart attack. We presented women with the mockups and assessed preferences for the device they would use; website settings, icons, and language; timing of reminders to complete daily symptom diaries; and understanding of the action plan and visual displays of symptom feedback to share with their provider. Eleven women (18% black; mean age 62.1) with varied digital literacy (36.4% never used ZOOM) from suburban (63.6%) or rural (36.4%) settings were included. Women from three focus groups determined the website settings, icon, and language; initial symptom survey format; and language in the action plan and final visual display of symptom feedback data, respectively. Our team made modifications to the content and design features iteratively based on preferences and scientific rationale. By delivering the intervention online in an acceptable format, we can reach women from settings in NC who otherwise may not have completed a structured educational program post-heart attack.
(Click here for large version)
Contact: lldavis@email.unc.edu
2021 Submissions
CD73 Predicts Disease Recurrence in Patients with CTNNB1 Mutant Endometrial Tumors
Jessica Bowser, PhD
CD73 PREDICTS DISEASE RECURRENCE IN PATIENTS WITH CTNNB1 MUTANT ENDOMETRIAL TUMORS
Katherine C. Kurnit1, Rebecca Hirsch2*, Jocelyn Alvarado2*, Pierre D. McCrea3, Russell R. Broaddus4,5, Jessica L. Bowser4,5,6
1. Department of Obstetrics and Gynecology, Section of Gynecologic Oncology, University of Chicago, Chicago, IL; 2. Biological & Biomedical Sciences Program, University of North Carolina School of Medicine, Chapel Hill, NC; 3. Department of Genetics, University of Texas MD Anderson Cancer Center, Houston, TX; 4. Department of Pathology and Laboratory Medicine, University of North Carolina School of Medicine, Chapel Hill, NC; 5. Lineberger Comprehensive Cancer Center, University of North Carolina, Chapel Hill, NC; 6. Corresponding Author; *Authors contributed equally
Of the 70% of women diagnosed with endometrial cancer (EC) that is surgically ‘curable’, being low grade, early stage endometrioid-type tumors, 10-15% of these women will recur and do poorly. CTNNB1 (β-catenin) mutation identifies patients at high risk for recurrence, however, its clinical utility is limited. Of patients with CTNNB1 mutant tumors, >50% do not recur. In this study, we assessed the clinical implications of CD73, a cell surface enzyme that regulates wild-type β-catenin, in CTNNB1 mutant tumors. qRT-PCR for CD73 was performed on n=29 EC tissues and immunohistochemistry for CD73 and β-catenin on n=11 tumors validated to have CTNNB1 mutation by next generation sequencing. Genetic studies were performed in HEC-1-A cells to determine mechanism. Patients with CTNNB1 mutant tumors with CD73Low expression showed an increased incidence of recurrence. CD73 levels were not different with clinical stage or lymphatic and vascular space invasion, indicating CD73 expression independently predicts recurrence. CD73 and β-catenin localization was strongly associated in CTNNB1 mutant tumors. Tumors expressing high CD73 expressed membrane β-catenin, whereas tumors with CD73 loss, β-catenin nuclear staining was increased. In The Cancer Genome Atlas (TCGA) data set for uterine cancer, ~85% of CTNNB1 mutations in endometrioid-type tumors occur in exon 3, which is outside the domain necessary for β-catenin membrane localization. Mechanistically, we show CD73 serves as a molecular sponge in CTNNB1 mutant tumors by localizing mutant β-catenin to the membrane, limiting its nuclear translocation and subsequent aggressiveness. These data reveal CD73 as a biomarker identifying women at high risk of recurrence.
(Click here for large version)
Contact: jessica_bowser@med.unc.edu
Ipatasertib, an Oral AKT Inhibitor, Effectively Inhibits Cell Proliferation and Migration, and Induces Apoptosis in Serous Endometrial Cancer Cell Lines in Vitro: Endometrial Cancer Molecularly Targeted Therapy Consortium
Lindsey Buckingham, MD
 Lindsey Buckingham is was raised in Pittsboro, NC and attended UNC for undergraduate and medical school. She trained in Obstetrics and Gynecology at Pennsylvania Hospital in Philadelphia and has been fortunate to return to UNC for Gynecologic Oncology fellowship. During her second year of fellowship training , Lindsey worked in Dr. Victoria Bae-Jump’s lab studying a novel, targeted therapy in endometrial cancer cell lines. During this year, she was also supported by the Geriatric Oncology T32 and is completing multiple projects, both prospective and retrospective, which focus on the impact of body composition on treatment tolerance and outcomes for women with gynecologic malignancies. She has a particular interest in frailty and patient reported outcomes measures. Following training, Lindsey plans to remain in academia as a surgeon-researcher.
Lindsey Buckingham is was raised in Pittsboro, NC and attended UNC for undergraduate and medical school. She trained in Obstetrics and Gynecology at Pennsylvania Hospital in Philadelphia and has been fortunate to return to UNC for Gynecologic Oncology fellowship. During her second year of fellowship training , Lindsey worked in Dr. Victoria Bae-Jump’s lab studying a novel, targeted therapy in endometrial cancer cell lines. During this year, she was also supported by the Geriatric Oncology T32 and is completing multiple projects, both prospective and retrospective, which focus on the impact of body composition on treatment tolerance and outcomes for women with gynecologic malignancies. She has a particular interest in frailty and patient reported outcomes measures. Following training, Lindsey plans to remain in academia as a surgeon-researcher.
Ipatasertib, an oral AKT inhibitor, effectively inhibits cell proliferation and migration, and induces apoptosis in serous endometrial cancer cell lines in vitro: Endometrial Cancer Molecularly Targeted Therapy Consortium
Lindsey Buckingham MD, Jillian O’Donnell MD, Tianran Hao BS, Angeles Alvarez Secord MD, Chunxiao Zhou MD, Victoria Bae-Jump MD, PhD
Objectives: Ipatasertib (IPAT) is a selective protein kinase B (AKT) inhibitor with promising data in solid tumors in both pre-clinical studies and clinical trials. IPAT targets the PI3K/AKT/mTOR pathway, making endometrial cancer (EC) an apt candidate for investigation. Our study evaluated the anti-proliferative efficacy of IPAT in human serous EC cell lines.
Methods: Two human serous EC cell lines, ARK-1 (PTEN wild type), and SPEC-2 (PTEN mutant), were used. Cells were exposed to varying concentrations of IPAT (Genentech). Cell proliferation was assessed by MTT and colony assays. Cell cycle progression was measured by Cellometer. Apoptosis was assessed by cleaved caspase-3 assay. Cell adhesion and wound healing assays were used to evaluate cell migration and invasion. Western immunoblotting performed for CDK4, CDK6, BCL-1, MCL-1, and snail and slug proteins.
Results: After 72 hours of treatment, the median IC50 was 0.97µM and 10.8µM in SPEC-2 and ARK-1 lines, respectively. IPAT induced cell cycle arrest in both SPEC-2 and ARK-1 lines. After treatment with 25µM concentration of IPAT, cleaved caspase 3 activity increased 2.9 fold in SPEC-2 and 1.75 fold in ARK-1, respectively (p<0.01). Cell adhesion was reduced by 15% and 17% (p<0.01) in SPEC-2 and ARK-1 cell lines, respectively. Treatment of cells with IPAT at 10µM increased phosphorylated-AKT (pAKT) expression and decreased phosphorylated-S6 (p-S6) expression in a time-dependent manner in both cell lines.
Conclusions: IPAT significantly suppressed cell proliferation through cell cycle arrest and apoptosis as well as inhibiting adhesion and migration in human serous EC cell lines. IPAT may be a promising targeted agent in the treatment of serous EC.
(Click here for large version)
Contact: lindsey.buckingham@unchealth.unc.edu
Does Deep Phenotyping Combined with Prenatal Exome Sequencing for Fetal Brain Abnormalities Increase Diagnostic Yield?
Kathleen Drexler, MD
 Kallie Drexler is a first year Maternal-Fetal Medicine fellow in the Department of OBGYN. She received a B.S. (Biochemistry, Spanish) from the University of Notre Dame, and subsequently obtained her MD from Baylor College of Medicine in Houston, Texas. She completed her residency training in Obstetrics and Gynecology at McGaw Medical Center of Northwestern. Her research interests include telehealth, remote patient monitoring and wearable devices, obesity and gestational diabetes.
Kallie Drexler is a first year Maternal-Fetal Medicine fellow in the Department of OBGYN. She received a B.S. (Biochemistry, Spanish) from the University of Notre Dame, and subsequently obtained her MD from Baylor College of Medicine in Houston, Texas. She completed her residency training in Obstetrics and Gynecology at McGaw Medical Center of Northwestern. Her research interests include telehealth, remote patient monitoring and wearable devices, obesity and gestational diabetes.
Does deep phenotyping combined with prenatal exome sequencing for fetal brain abnormalities increase diagnostic yield?
The objective of our study was to evaluate whether deep phenotyping of fetal brain abnormalities (FBA) increases diagnostic yield of trio-exome sequencing (ES) compared to standard prenatal phenotyping. This was a prospective prenatal ES study recruiting from multiple sites. Participants were eligible if a fetal anomaly was diagnosed and subsequently found to have a normal microarray. We defined deep phenotyping as prenatal phenotype based on fetal MRI, autopsy (when available), and known phenotypes of other affected family members. Standard phenotyping was defined as phenotype based on targeted ultrasound alone. Cases with diagnostic ES results were compared to those with non-diagnostic results by available phenotyping. Data were analyzed using t-test, chi-square, and pairwise comparisons as appropriate with p<0.05 considered significant. A total of 115 trios were sequenced, of which 41 (35.6%) had FBA. Of the 41 trios with FBA, 14 (34.1%) cases had a diagnostic ES result and 27 (65.9%) had a non-diagnostic result. There was no difference in the number of cases with multisystem organ abnormalities between groups (100% vs 77.8%, p=0.08). Among those with a positive ES result, there were more cases with deep phenotyping (MRI, autopsy, similar FBA phenotype in prior pregnancy), though this was not statistically significant. MRI was not significantly different between the two groups (28.6% vs 22.2%, p=0.7), but autopsies were significantly higher in those with diagnostic ES results (42.9% vs 11.1%, p=0.04). In conclusion, additional phenotypic information, particularly autopsy, may increase diagnostic yield of prenatal ES for FBA.
(Click here for large version)
Contact: kathleen.drexler@unchealth.unc.edu
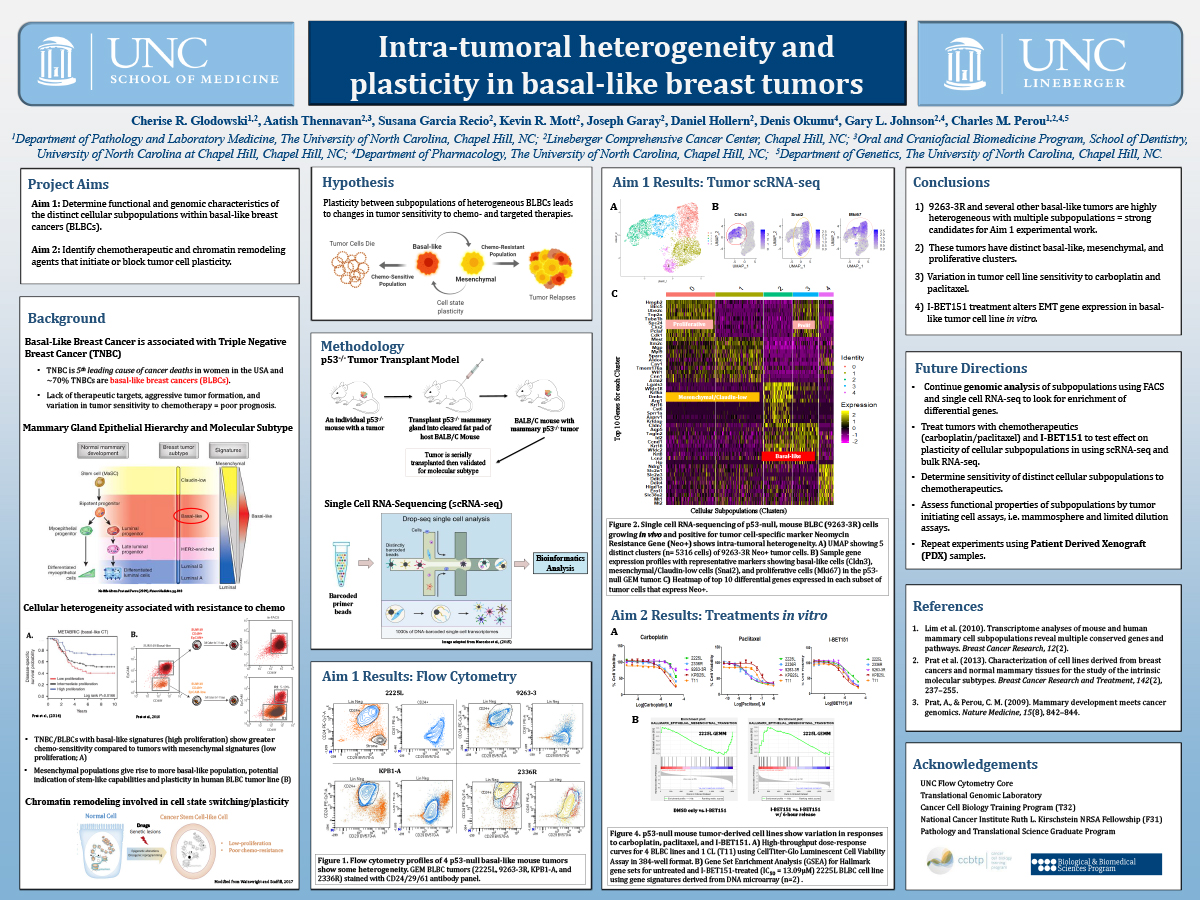
Intra-tumoral Heterogeneity in Basal-like Breast Cancers
Cherise Glodowski, MPhil
 Cherise is a PhD candidate and Ruth L. Kirschstein NCI Predoctoral Fellow in the Perou Lab studying intratumoral heterogeneity and plasticity in Triple Negative Breast Cancers at UNC’s Lineberger Comprehensive Cancer Center. Cherise received her undergraduate degrees in Nutritional Biochemistry and Classics at University of California, Davis, and her master’s degree in Biological Sciences at the University of Cambridge, UK. In between her master’s degree and starting at UNC, she worked simultaneously as a Clinical Embryologist at Northern California Fertility Medical Center and as an Adjunct Professor of Nutrition at Los Rios Community College. Cherise is passionate about women’s health, health disparities, and precision medicine, and is a member of the Lineberger Equity Council and a co-founder of UNC’s Women’s Health Multidisciplinary Consortium (WHMC), which aims to unite researchers for the advancement of women’s health research and early career training. Additionally, Cherise is an avid dancer and playwright, and loves theatre arts, teaching, traveling, and spending time with her friends and family.
Cherise is a PhD candidate and Ruth L. Kirschstein NCI Predoctoral Fellow in the Perou Lab studying intratumoral heterogeneity and plasticity in Triple Negative Breast Cancers at UNC’s Lineberger Comprehensive Cancer Center. Cherise received her undergraduate degrees in Nutritional Biochemistry and Classics at University of California, Davis, and her master’s degree in Biological Sciences at the University of Cambridge, UK. In between her master’s degree and starting at UNC, she worked simultaneously as a Clinical Embryologist at Northern California Fertility Medical Center and as an Adjunct Professor of Nutrition at Los Rios Community College. Cherise is passionate about women’s health, health disparities, and precision medicine, and is a member of the Lineberger Equity Council and a co-founder of UNC’s Women’s Health Multidisciplinary Consortium (WHMC), which aims to unite researchers for the advancement of women’s health research and early career training. Additionally, Cherise is an avid dancer and playwright, and loves theatre arts, teaching, traveling, and spending time with her friends and family.
INTRA-TUMORAL HETEROGENEITY IN BASAL-LIKE BREAST CANCERS
Triple Negative Breast Cancer (TNBC) is an aggressive malignancy with a poor prognosis that accounts for 10-20% of breast cancer cases worldwide. Tumor resistance to chemotherapy is a major obstacle facing patients with TNBCs, as TNBCs lack conventional druggable targets and patients rely on chemotherapy as the main treatment option. Intra-tumoral heterogeneity and tumor cell plasticity are thought to contribute to resistance to chemotherapy. More than 70% of TNBCs subtype as basal-like breast cancers (BLBCs), which are characterized by high intra-tumoral heterogeneity and diverse tumor cells. Currently, the mechanism by which BLBC tumor cells develop resistance to chemotherapy is poorly understood. This work aims to identify the genetic regulators of plasticity between subpopulations of BLBCs and to test whether targeted agents blocking or initiating this plasticity can lead to changes in tumor chemo-sensitivity. To characterize the heterogeneity of epithelial cells in BLBC tumors, we performed flow cytometry and single cell RNA-sequencing (scRNA-seq) on multiple, independently arisen p53-null murine BLBC tumors. We found clear intra-tumoral heterogeneity with distinct cellular subpopulations present within most BLBC tumors tested thus far. We are currently using gene expression and network analyses to identify possible genetic regulators of each subpopulation. Further, we are testing chromatin-remodeling inhibitors and chemotherapies on murine BLBCs to measure transcriptional response to therapy. The goal is to determine if these cellular subpopulations change frequency or phenotype with treatment. Ultimately, identifying regulators and targeted agents that modulate cellular plasticity and chemo-sensitivity would lead to improved therapeutic regimens for patients with chemo-resistant TNBCs.
(Click here for large version)
Contact: crg11@email.unc.edu
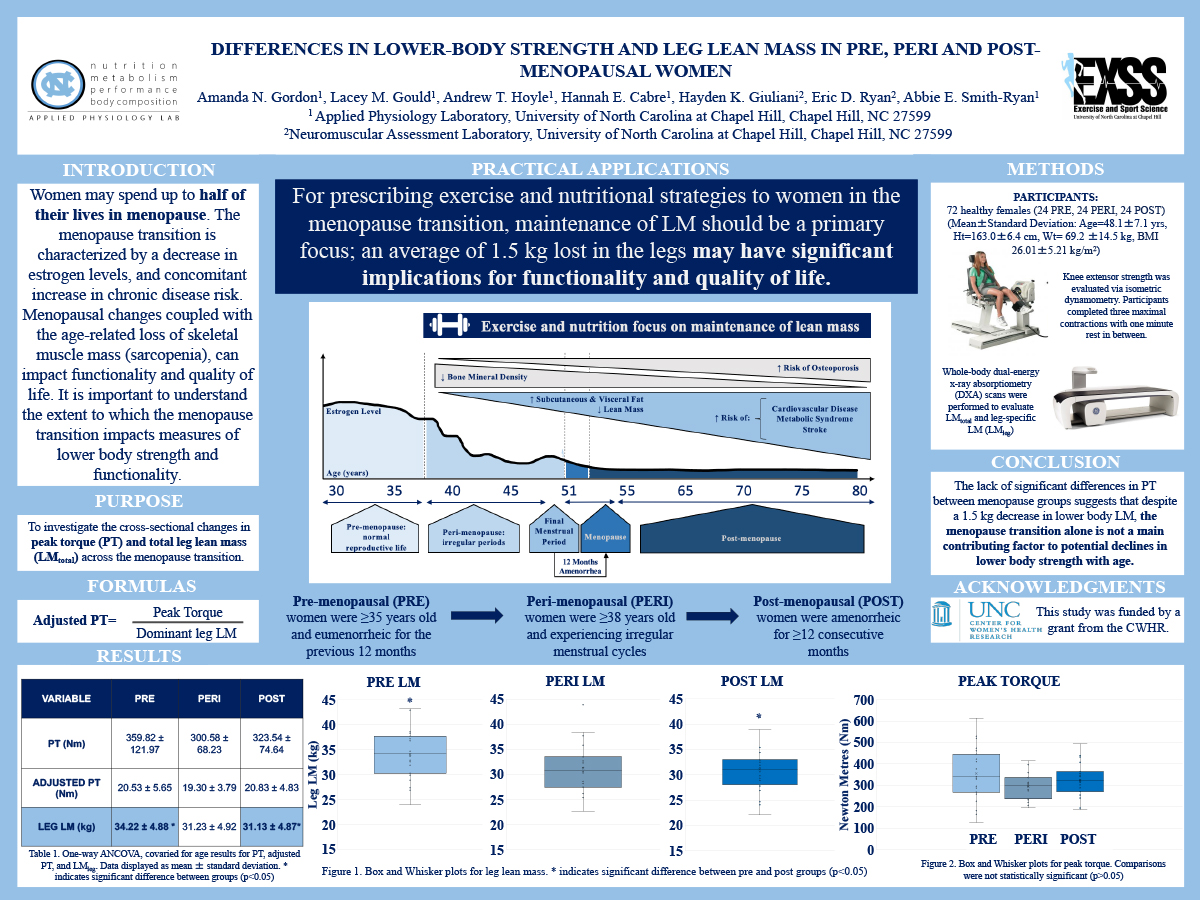
Differences in Lower-Body Strength and Leg Lean Mass in Pre, Peri and Post-Menopausal Women
Amanda Gordon, CSCS
 Amanda Gordon is an upcoming 2nd year Masters student in Exercise Physiology at The University of North Carolina at Chapel Hill under the mentorship of Dr. Abbie Smith-Ryan in the Applied Physiology Lab. Amanda’s research interests include nutrition supplementation, body composition and exercise performance specifically as they relate to women’s health. Her upcoming project will focus on the effects of creatine monohydrate supplementation on exercise recovery throughout the menstrual cycle. Amanda graduated from Auburn University with a BS in Exercise Science. Amanda is a Certified Strength and Conditioning Specialist (CSCS) with the National Strength and Conditioning Association
Amanda Gordon is an upcoming 2nd year Masters student in Exercise Physiology at The University of North Carolina at Chapel Hill under the mentorship of Dr. Abbie Smith-Ryan in the Applied Physiology Lab. Amanda’s research interests include nutrition supplementation, body composition and exercise performance specifically as they relate to women’s health. Her upcoming project will focus on the effects of creatine monohydrate supplementation on exercise recovery throughout the menstrual cycle. Amanda graduated from Auburn University with a BS in Exercise Science. Amanda is a Certified Strength and Conditioning Specialist (CSCS) with the National Strength and Conditioning Association
DIFFERENCES IN LOWER-BODY STRENGTH AND LEG LEAN MASS IN PRE, PERI AND POST-MENOPAUSAL WOMEN
Amanda N. Gordon1, Lacey M. Gould1, Andrew T. Hoyle1, Hannah E. Cabre1, Hayden K. Giuliani2, Eric D. Ryan2, Abbie E. Smith-Ryan1
1. Applied Physiology Laboratory, University of North Carolina at Chapel Hill, Chapel Hill, NC 27599; 2. Neuromuscular Assessment Laboratory, University of North Carolina at Chapel Hill, Chapel Hill, NC 27599
PURPOSE: To investigate the cross-sectional changes in peak torque (PT) and total leg lean mass (LMtotal) across the menopause transition. METHODS: Seventy-two healthy females (Mean±Standard Deviation: Age=48.1±7.1 yrs, Ht=163.0±6.4 cm, Wt= 69.2 ±14.5 kg) were stratified by menopausal status. Pre-menopausal (PRE) women were ≥35 years old and eumenorrheic for the previous 12 months. Peri-menopausal (PERI) women were ≥38 years old and experiencing irregular menstrual cycles, and post-menopausal (POST) women were amenorrheic for ≥12 consecutive months. Knee extensor strength was evaluated via isometric dynamometry. Whole-body dual-energy x-ray absorptiometry (DXA) scans were performed to evaluate LMtotal and leg-specific LM (LMleg). To account for differences in LM, dominant leg LM was used to calculate adjusted PT (PT/LMtotal). One-way ANCOVAs, covaried for age, were used to evaluate differences in PT, adjusted PT, and LMleg between groups. RESULTS: There were no significant differences in absolute PT between PRE and PERI (Mean Difference [MD]±Standard Error [SE]: 61.5±26.5 Nm, p=0.070) or PRE and POST (41.1±26.9 Nm, p=0.391). No significant differences were found in adjusted PT between PRE and PERI (MD±SE: 1.3±1.4 Nm, p<0.99) or PRE and POST (-0.2±1.4 Nm, p<0.99) menopausal groups. LMtotal trended downward between PRE and POST (MD±SE: 1.6±0.6 kg, p=0.055), but was not significantly different between PRE and PERI (1.4±0.6 kg, p=0.085). CONCLUSIONS: The lack of significant differences in PT between menopause groups suggests that despite a decrease in lower body LM, the menopause transition alone is not a main contributing factor to potential declines in lower body strength with age.
(Click here for large version)
Contact: amandang@email.unc.edu
Impact of Menopausal Status and BMI on Metabolic Flexibility
Lacey M. Gould, BS, CISSN
 Lacey Gould is from Clemmons, North Carolina and graduated from High Point University with a Bachelor of Science degree in Exercise Science and Biology. She is graduating in May 2021 with a master’s degree in Exercise Physiology from UNC Chapel Hill following the completion of her master’s thesis work that investigates metabolic health and body composition in women throughout the menopause transition. She has a strong desire to have a positive impact on the health of others and is focused on studying the impacts of nutrition and exercise in both clinical and athlete populations, with a special interest in female physiology. Lacey is and thankful for the opportunity to work alongside well-established and inspiring faculty, staff, and graduate students here at UNC Chapel Hill.
Lacey Gould is from Clemmons, North Carolina and graduated from High Point University with a Bachelor of Science degree in Exercise Science and Biology. She is graduating in May 2021 with a master’s degree in Exercise Physiology from UNC Chapel Hill following the completion of her master’s thesis work that investigates metabolic health and body composition in women throughout the menopause transition. She has a strong desire to have a positive impact on the health of others and is focused on studying the impacts of nutrition and exercise in both clinical and athlete populations, with a special interest in female physiology. Lacey is and thankful for the opportunity to work alongside well-established and inspiring faculty, staff, and graduate students here at UNC Chapel Hill.
IMPACT OF MENOPAUSAL STATUS AND BMI ON METABOLIC FLEXIBILITY
Lacey M. Gould1, Amanda N. Gordon1, Andrew T. Hoyle1, Hannah E. Cabre1, Abbie E. Smith- Ryan1
1. University of North Carolina at Chapel Hill, Chapel Hill, NC 27599
PURPOSE: To compare fat and carbohydrate oxidation at rest and during exercise (metabolic flexibility) in pre-menopausal (PRE), peri-menopausal (PERI), and post-menopausal (POST) women of varying adiposity levels. METHODS: Respiratory exchange ratio (RER) was measured via indirect calorimetry at rest (REST) and during a progressive exercise bout at 3 intensities: low intensity (LOW; <30% heart rate reserve [HRR]), moderate (MOD; 30- 50%HRR), and high (HIGH; 50-75%HRR) in 72 females (24 PRE, 24 PERI, 24 POST; Mean±SD: BMI 26.01±5.21 kg/m2, Range: 18.81-41.00 kg/m2). PRE were ≥35 yrs and eumenorrheic, PERI were ≥38 yrs and experiencing irregular menstrual cycles, and POST reported amenorrhea for ≥12 months. One-way ANOVAs with Bonferroni post-hoc comparisons were conducted by intensity (REST, LOW, MOD, HIGH) for the total sample and stratified by BMI: normal (N): 18.5-24.9 kg/m2 and overweight/obese (OB) ≥25.0 kg/m2. RESULTS: At REST, PERI had lower RER compared to PRE (Mean Difference [MD]±Standard Error [SE]: – 0.03±0.02 a.u., p=0.09) and POST (-0.03±0.02 a.u., p=0.08). During LOW, PERI had significantly lower RER than POST (MD±SE: -0.06±0.02 a.u., p=0.03). RER was similar for MOD and HIGH intensities (p>0.05). RER was similar across intensities in N individuals (p>0.05), however, RER in OB PRE was significantly greater than OB PERI at REST (MD±SE: 0.05±0.02 a.u., p=0.04); OB PERI was significantly lower than OB POST during LOW (- 0.08±0.03, p=0.02). CONCLUSIONS: PERI utilized more fat compared to POST during low intensity exercise, which may support better body composition and metabolic health; metabolic inflexibility through menopause may be exacerbated by obesity.
(Click here for large version)
Contact: lmgould@live.unc.edu
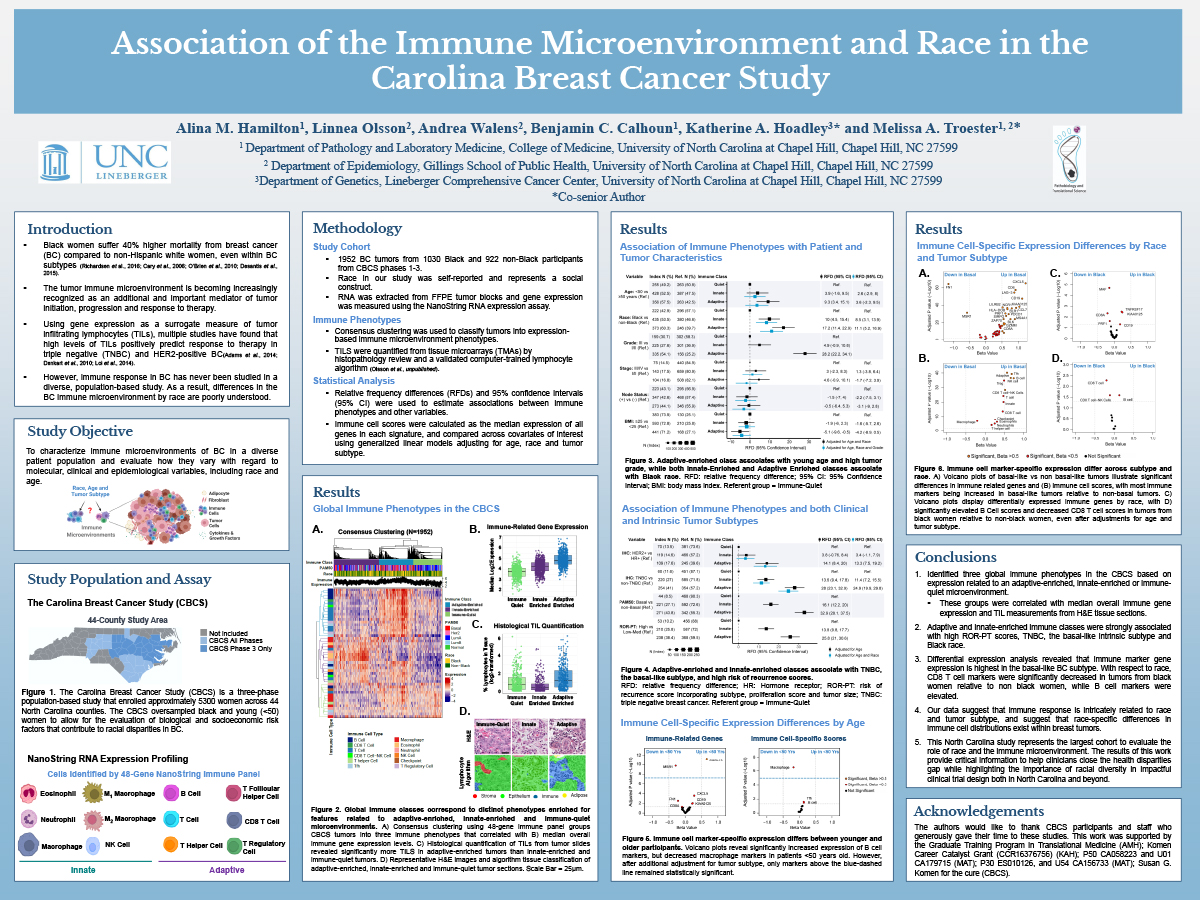
Association of the Immune Microenvironment and Race in the Carolina Breast Cancer Study
Alina M. Hamilton, MS
Alina is a PhD student in the laboratories of Dr. Melissa Troester and Dr. Katherine Hoadley studying the tumor microenvironment and its association with racial and survivorship disparities in breast cancer. Alina received her Bachelor of Science in Biology at the University of Texas Pan American followed by a Master’s in Biology at the University of Texas Rio Grande Valley, where she studied the effect of various environmental exposures on female pubertal onset, mammary gland development and breast cancer risk. Alina is a recipient of the Ruth L. Kirschstein Fellowship and the 2021 UNC Horizon Award, which recognizes dissertation research with high potential for making a significant impact on the well-being of North Carolina citizens. Alina is co-founder of the Pathobiology and Translational Science Student Committee, and co-founder of the UNC Women’s Health Multidisciplinary Consortium (WHMC), which seeks to advance research in women’s health through multidisciplinary collaboration and early career training. She serves as a peer mentor for UNC IMSD and BBSP programs, volunteers at the annual Susan G. Komen® Triangle Race for the Cure, and participates in scientific outreach benefiting her local North Carolina community. Outside of her work in the lab, she enjoys time with her family, long distance running and cycling, playing guitar and gardening.
Association of the immune microenvironment and race in the Carolina Breast Cancer Study
Alina M. Hamilton1, Linnea Olsson2, Andrea Walens2, Benjamin C. Calhoun1, Katherine A. Hoadley3 and Melissa A. Troester1,2
1. Department of Pathology and Laboratory Medicine, College of Medicine, University of North Carolina at Chapel Hill, Chapel Hill, NC 27599; 2. Department of Epidemiology, Gillings School of Public Health, University of North Carolina at Chapel Hill, Chapel Hill, NC 27599; 3. Department of Genetics, Lineberger Comprehensive Cancer Center, University of North Carolina at Chapel Hill, Chapel Hill, NC 27599
Black women suffer a 40% higher breast cancer (BC) mortality rate compared to White women, and the underlying causes of this disparity remain uncertain. Evidence supports the importance of the immune microenvironment in BC outcomes, but immune response differences by race are poorly understood. Therefore, we sought to characterize the immune microenvironment of BC to evaluate how phenotypes of immune response vary across race and tumor intrinsic subtype. We curated a 48- gene panel representing 12 immune cell types and performed gene expression profiling on tumors from 1030 Black and 922 Non-Black participants from the Carolina Breast Cancer Study. Using consensus clustering, we identified three global immune phenotypes defined by features related to an Adaptive- enriched, Innate-enriched, or Immune-quiet microenvironment. Both Adaptive-enriched and Innate- enriched tumors were associated with high risk of recurrence scores, the basal-like intrinsic subtype and Black race. Using differential expression analyses, we found that nearly all immune cell scores were significantly increased in basal-like tumors relative to non-basal tumors. Among Black participants, CD8 T cell scores were significantly decreased and B cell scores were increased relative to non-Black participants, even after adjustments for age and tumor subtype. Our data suggest that immune response is intricately related to both race and tumor subtype, with race-specific differences in the distribution of immune cell types within breast tumors. The results of this work provide critical information to help clinicians close the health disparities gap while highlighting the importance of racial diversity in impactful clinical trial design both in North Carolina and beyond.
(Click here for large version)
Contact: alinamh@email.unc.edu
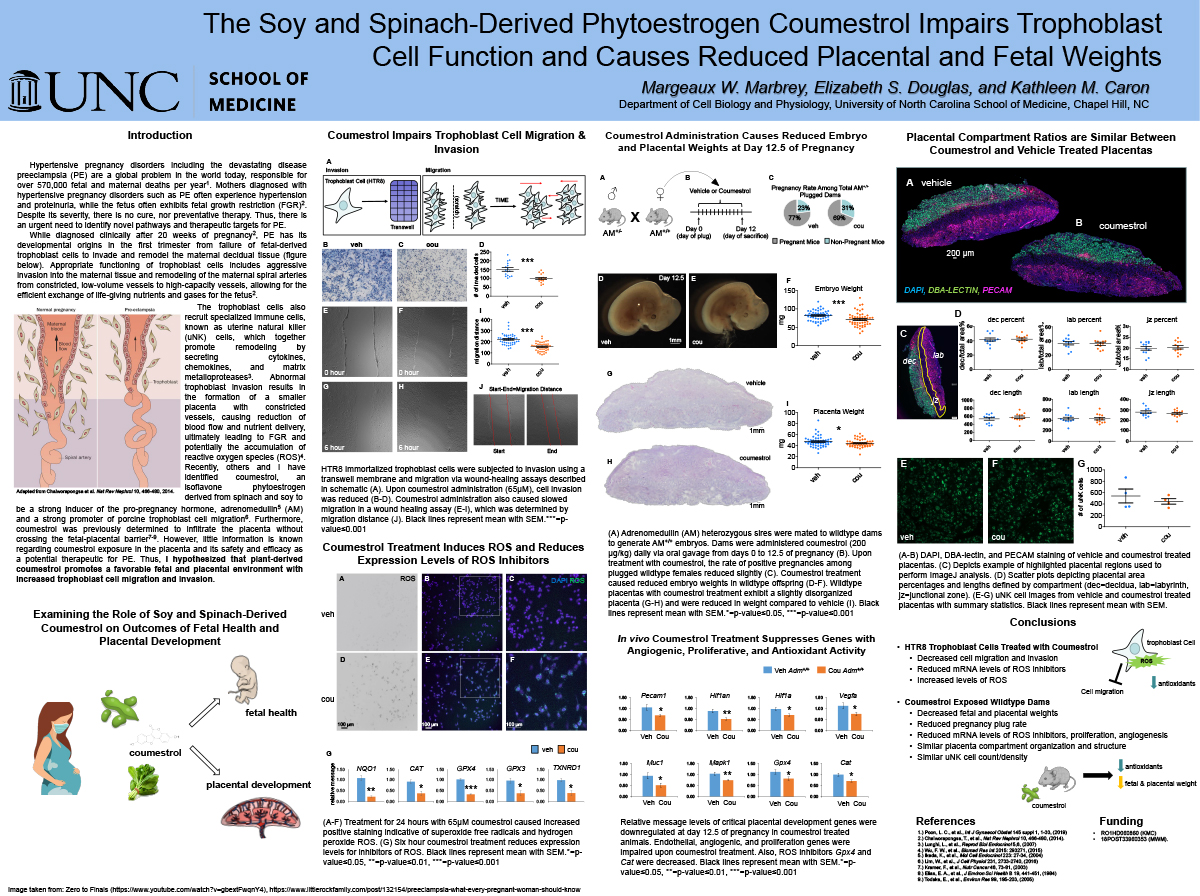
Plant-Derived Phytoestrogen Coumestrol Inhibits Trophoblast Cell Function and Causes Decreased Fetal and Placental Weights
Margeaux W. Marbrey, PhD
 Dr. Margeaux Marbrey received her PhD at Baylor College of Medicine by examining the role of the highly regulated progesterone signaling pathway during early pregnancy under the leadership of Dr. Francesco DeMayo. In continuing her strong commitment to female reproductive biology, Dr. Marbrey joined the laboratory of Dr. Kathleen Caron and has focused her research on the molecular factors that coordinate the beginning of pregnancy and the development of a healthy placenta. She has specifically examined how environmental effectors such as plasticizers and phytoestrogens as well as tobacco products including e-cigarettes can affect embryo attachment, placental development, and the progression of pregnancy. Results from her work shed light on the factors that result in infertility and miscarriage.
Dr. Margeaux Marbrey received her PhD at Baylor College of Medicine by examining the role of the highly regulated progesterone signaling pathway during early pregnancy under the leadership of Dr. Francesco DeMayo. In continuing her strong commitment to female reproductive biology, Dr. Marbrey joined the laboratory of Dr. Kathleen Caron and has focused her research on the molecular factors that coordinate the beginning of pregnancy and the development of a healthy placenta. She has specifically examined how environmental effectors such as plasticizers and phytoestrogens as well as tobacco products including e-cigarettes can affect embryo attachment, placental development, and the progression of pregnancy. Results from her work shed light on the factors that result in infertility and miscarriage.
Plant-derived phytoestrogen coumestrol inhibits trophoblast cell function and causes decreased fetal and placental weights
Preeclampsia (PE) is a hypertensive pregnancy disorder affecting 8% of pregnant women, resulting in life-threatening hypertension, proteinuria, and fetal growth restriction (FGR). PE is caused by the improper invasion of fetal trophoblast cells and reduction of spiral artery remodeling resulting in unstable vasculature and accumulation of reactive oxygen species (ROS). The placenta is sensitive to a variety of external factors including diet and cigarette smoke. Recently, we have identified coumestrol, a phytoestrogen derived from spinach and soy, does not cross the fetal-placental barrier and induces the protective pregnancy hormone, adrenomedullin. Thus, coumestrol may be a valuable supplement to promote placentation and prevention of PE. Since the popularity of vegetarian and soy-based diets has escalated recently, we sought to examine how coumestrol may affect the placenta. I hypothesized that plant-derived coumestrol promotes a favorable fetal and placental environment with increased trophoblast cell migration and invasion. We first examined trophoblast cell function and showed that coumestrol significantly reduced migration and invasion. Upon gene expression analysis, inhibitors of ROS were significantly decreased. To examine in vivo pregnancy, coumestrol was administered to wildtype mice from pregnancy days 0-12.5. Coumestrol exposed fetal and placental tissues were decreased in weight compared to vehicle. Therefore, coumestrol impairs trophoblast function and may induce ROS resulting in decreased placental weight and FGR. These data suggest that consuming vegetarian or soy-based diets high in coumestrol during pregnancy may cause deleterious effects to the fetus and placenta.
(Click here for large version)
Contact: margeaux_wetendorf@med.unc.edu
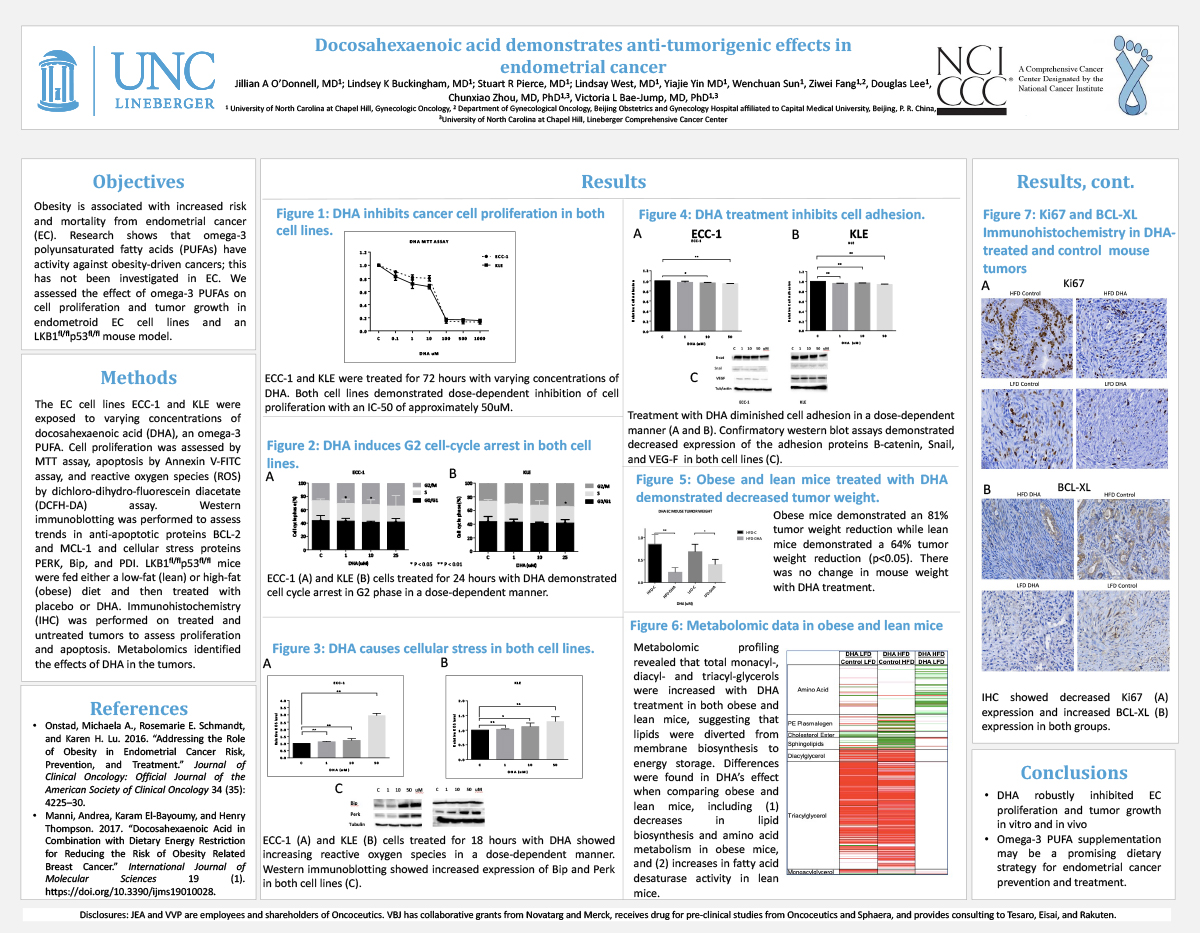
Docosahexaenoic Acid Demonstrates Anti-Tumorigenic Effects in Endometrial Cancer
Jillian A O’Donnell, MD
Docosahexaenoic acid demonstrates anti-tumorigenic effects in endometrial cancer
Jillian A O’Donnell, MD1; Lindsey K Buckingham, MD1; Stuart R Pierce, MD1; Lindsay West, MD1, Yiajie Yin MD1, Wenchuan Sun1, Ziwei Fang1,3, Douglas Lee, PhD Chunxiao Zhou, MD, PhD1,4, Victoria L Bae-Jump, MD, PhD1,4
1. University of North Carolina at Chapel Hill, Gynecologic Oncology; 2. North Carolina Central University; 3. Department of Gynecological Oncology, Beijing Obstetrics and Gynecology Hospital affiliated to Capital Medical University, Beijing, P. R. China; 4. University of North Carolina at Chapel Hill, Lineberger Comprehensive Cancer Center; 5. Omic Insight, Durham, NC
Objectives: Obesity is associated with increased risk and mortality from endometrial cancer (EC). Research shows that omega-3 polyunsaturated fatty acids (PUFAs) have activity against obesity-driven cancers; this has not been investigated in EC. We assessed the effect of omega-3 PUFAs on cell proliferation and tumor growth in endometroid EC cell lines and an LKB1fl/flp53fl/fl mouse model.
Methods: The EC cell lines ECC-1 and KLE were exposed to varying concentrations ofdocosahexaenoic acid (DHA), an omega-3 PUFA. Cell proliferation was assessed by MTT assay, apoptosis by Annexin V-FITC assay, and reactive oxygen species (ROS) by dichloro-dihydro-fluorescein diacetate (DCFH-DA) assay. Western immunoblotting was performed to assess trends in anti-apoptotic proteins BCL-2 and MCL-1 and cellular stress proteins PERK, Bip, and PDI.
LKB1fl/flp53fl/fl mice were fed either a low-fat (lean) or high-fat (obese) diet and then treated with placebo or DHA. Immunohistochemistry (IHC) was performed on treated and untreated tumors to assess proliferation and apoptosis. Metabolomics identified the effects of DHA in the tumors.
Results: DHA caused dose-dependent inhibition of cell proliferation in both cell lines. DHA increased expression of annexin V (p<0.05) as well as decreased BCL-2 and MCL-1 expression. DHA increased ROS and induced PERK, Bip, and PDI expression in both cell lines.
Obese mice demonstrated an 81% tumor weight reduction while lean mice demonstrated a 64% tumor weight reduction (p<0.05). There was no change in mouse weight with DHA treatment. IHC showed decreased Ki67 and increased BCL-XL expression in both groups with DHA treatment. Metabolomic profiling revealed that total monacyl-, diacyl- and triacyl-glycerols were increased with DHA treatment in both obese and lean mice, suggesting that lipids were diverted from membrane biosynthesis to energy storage. Differences were found in DHA’s effect when comparing obese and lean mice, including (1) decreases in lipid biosynthesis and amino acid metabolism in obese mice, and (2) increases in fatty acid desaturase activity in lean mice.
Conclusions: DHA inhibits EC proliferation and tumor growth in vitro and in vivo. Omega-3 PUFAs may be a promising dietary strategy for EC prevention and treatment.
(Click here for large version)
Contact: jillian.odonnell@unchealth.unc.edu
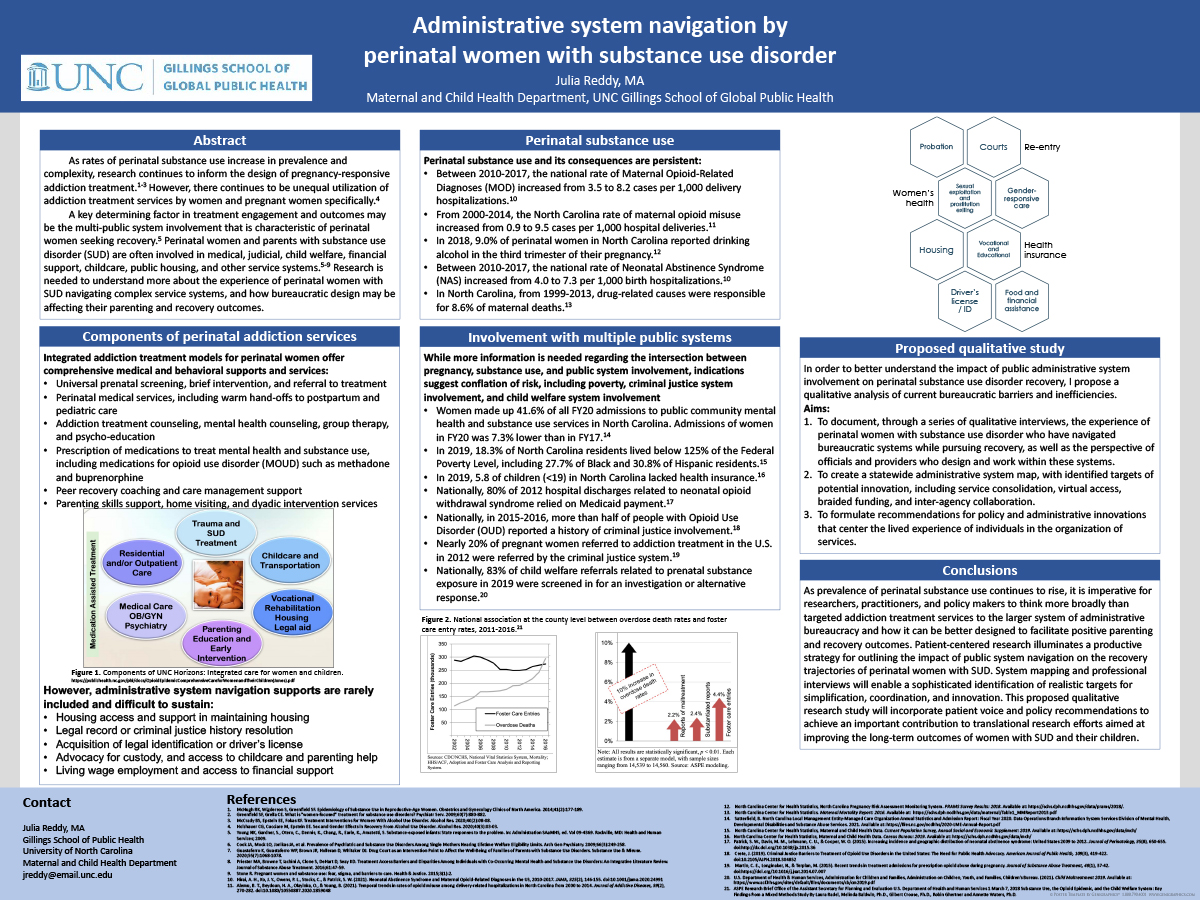
Administrative System Navigation by Perinatal Women with Substance Use Disorder
Julia Reddy, MA
 Julia is a research intern for the Children’s Data Network and a doctoral student at the University of North Carolina at Chapel Hill Gillings School for International Public Health in the Maternal and Child Health Department. Her research interests include families impacted by substance use disorders and intersections between families and public service systems. Previously, Julia served as the Women and Families Service Coordinator for the Massachusetts Department of Public Health’s Bureau of Substance Addiction Services, where she focused on improving the structural design of addiction treatment and community-based service systems to better serve women, perinatal women, and families. Julia received a master’s degree from the Eliot-Pearson Department of Human Development and Child Study at Tufts University and a BA from Duke University.
Julia is a research intern for the Children’s Data Network and a doctoral student at the University of North Carolina at Chapel Hill Gillings School for International Public Health in the Maternal and Child Health Department. Her research interests include families impacted by substance use disorders and intersections between families and public service systems. Previously, Julia served as the Women and Families Service Coordinator for the Massachusetts Department of Public Health’s Bureau of Substance Addiction Services, where she focused on improving the structural design of addiction treatment and community-based service systems to better serve women, perinatal women, and families. Julia received a master’s degree from the Eliot-Pearson Department of Human Development and Child Study at Tufts University and a BA from Duke University.
Administrative system navigation by perinatal women with substance use disorder
There are substantial gender differences in the etiology, manifestations, and evidence-based treatment of substance use disorders in women and perinatal people1. Over the past four decades, research has grown to identify important components of gender-responsive addiction treatment2,3. More research is needed, however, to investigate gender differences in barriers to access and adherence to treatment services and achievement of recovery goals4. A key determining factor in treatment engagement and outcomes may be the multi-system involvement characteristic of perinatal women seeking recovery from substance use disorders5. Perinatal and parenting people with substance use disorder are often involved in medical, judicial, child welfare, financial support, and other service systems6,7. Involvement with multiple administrative systems presents competing priorities, barriers to access, and limitations to the provision of comprehensive, family-centered care8,9. While the viral suppression efforts that arose in response to COVID-19 exacerbated many of these gaps in service continuity, it also exposed opportunities for improved collaboration and service integration. The proposed poster will map the trajectories of perinatal people seeking recovery from substance use disorder in North Carolina as they navigate multiple service systems and highlight the challenges that arise from a lack of integration at the provider and bureaucratic level. The impacts of COVID-19 on service delivery will be presented as an opportunity to engage in and sustain practice improvement. Lastly, a research study will be proposed that centers qualitative interviews with perinatal people who have opioid use disorder and are seeking recovery in North Carolina to inquire about the lived experience of navigating multiple administrative and service provision systems, with an aim at exposing additional opportunities to improve service cohesion and access.
- McHugh RK, Wigderson S, Greenfield SF. Epidemiology of Substance Use in Reproductive-Age Women. Obstetrics and Gynecology Clinics of North America. 2014;41(2):177-189.
- Greenfield SF, Grella CE. What is “women-focused” treatment for substance use disorders? Psychiatr Serv. 2009;60(7):880-882.
- McCrady BS, Epstein EE, Fokas KF. Treatment Interventions for Women With Alcohol Use Disorder. Alcohol Res. 2020;40(2):08-08.
- Holzhauer CG, Cucciare M, Epstein EE. Sex and Gender Effects in Recovery From Alcohol Use Disorder. Alcohol Res. 2020;40(3):03-03.
- Young NK, Gardner, S., Otero, C., Dennis, K., Chang, R., Earle, K., Amatetti, S. Substance-exposed infants: State responses to the problem. In: Administration SAaMHS, ed. Vol 09-4369. Rockville, MD: Health and Human Services; 2009.
- Cook JA, Mock LO, Jonikas JA, et al. Prevalence of Psychiatric and Substance Use Disorders Among Single Mothers Nearing Lifetime Welfare Eligibility Limits. Arch Gen Psychiatry. 2009;66(3):249-258.
- Guastaferro K, Guastaferro WP, Brown JR, Holleran D, Whitaker DJ. Drug Court as an Intervention Point to Affect the Well-Being of Families of Parents with Substance Use Disorders. Substance Use & Misuse. 2020;55(7):1068-1078.
- Priester MA, Browne T, Iachini A, Clone S, DeHart D, Seay KD. Treatment Access Barriers and Disparities Among Individuals with Co-Occurring Mental Health and Substance Use Disorders: An Integrative Literature Review. Journal of Substance Abuse Treatment. 2016;61:47-59.
- Stone R. Pregnant women and substance use: fear, stigma, and barriers to care. Health & Justice. 2015;3(1):2.
(Click here for large version)
Contact: jreddy@email.unc.edu
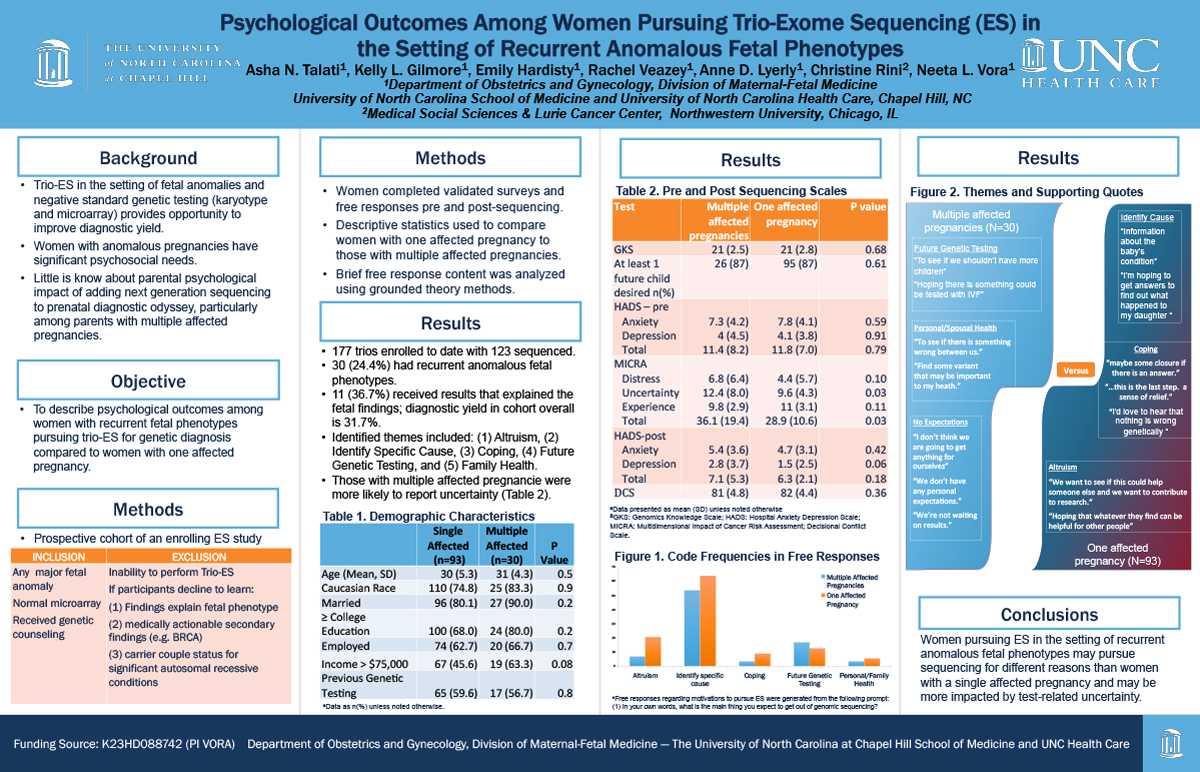
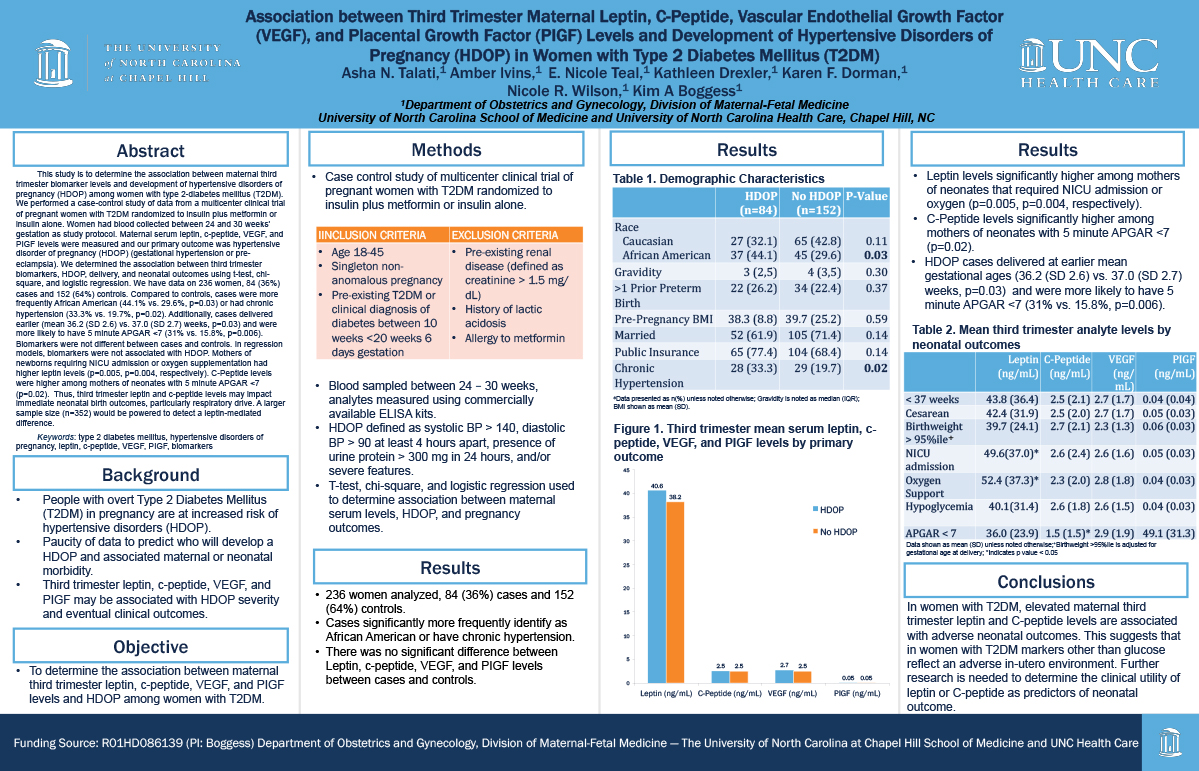
Psychological Outcomes Amongst Women Pursuing Trio-Exome Sequencing (ES) in the Setting of Recurrent Anomalous Fetal Phenotypes / Associations between Third Trimester Maternal Leptin, C-Peptide, Vascular Endothelial Growth Factor (VEGF), and Placental Growth Factor (PIGF) Levels and Development of Hypertensive Disorders of Pregnancy (HDOP) in Women with Type 2 Diabetes Mellitus (T2DM)
Asha N. Talati, MD, MSCR
 Asha Talati MD, MSCR is a clinical instructor and fellow in the division of Maternal Fetal Medicine, Department of Obstetrics & Gynecology at University of North Carolina at Chapel Hill. Dr. Talati completed medical school and residency at Case Western Reserve University in Cleveland, Ohio, where she was a part of the Alpha Omega Alpha Honor Society. She served as chief resident at University Hospitals Case Medical Center in Obstetrics & Gynecology 2016-2017. From 2017-2019, Dr. Talati completed the Women’s Health Research fellowship and earned her Masters of Science in Clinical Research at UNC, serving as a clinical instructor in the division of General Obstetrics & Gynecology. Dr. Talati is currently in her second year of a combined Maternal Fetal Medicine and Medical Genetics & Genomics fellowship. Her current research includes assessing how biopsychosocial factors impact maternal decisions for prenatal diagnosis and pregnancy care in the setting of fetal anomalies, impact of chronic medical conditions on perinatal outcomes, and the use of telehealth for maternity care.
Asha Talati MD, MSCR is a clinical instructor and fellow in the division of Maternal Fetal Medicine, Department of Obstetrics & Gynecology at University of North Carolina at Chapel Hill. Dr. Talati completed medical school and residency at Case Western Reserve University in Cleveland, Ohio, where she was a part of the Alpha Omega Alpha Honor Society. She served as chief resident at University Hospitals Case Medical Center in Obstetrics & Gynecology 2016-2017. From 2017-2019, Dr. Talati completed the Women’s Health Research fellowship and earned her Masters of Science in Clinical Research at UNC, serving as a clinical instructor in the division of General Obstetrics & Gynecology. Dr. Talati is currently in her second year of a combined Maternal Fetal Medicine and Medical Genetics & Genomics fellowship. Her current research includes assessing how biopsychosocial factors impact maternal decisions for prenatal diagnosis and pregnancy care in the setting of fetal anomalies, impact of chronic medical conditions on perinatal outcomes, and the use of telehealth for maternity care.
Psychological Outcomes Amongst Women Pursuing Trio-Exome Sequencing (ES) in the Setting of Recurrent Anomalous Fetal Phenotypes
The current study describes psychological outcomes among women with recurrent fetal phenotypes pursuing trio-exome sequencing (ES) for genetic diagnosis compared to women with one affected pregnancy. We analyzed a prospective cohort that enrolls patients with any major fetal anomaly and normal microarray. Women completed validated scales and short-free responses before and after sequencing. Psychological outcomes were compared between women with recurrent fetal phenotypes and those with only one affected pregnancy. Free responses were compared using thematic content analysis. 177 trios were enrolled in the study; of those, 123 have sequencing data. 30 (24.4%) women had recurrent anomalous pregnancies; among them, 11 women received a fetal result (36.7%). Diagnostic yield in the cohort overall was 31.7%. There was no significant difference in pre and post-sequencing anxiety, depression, or decisional conflict scores between the two groups. However, women with recurrent phenotypes had significantly higher uncertainty scores (12.4 vs. 9.6 p= 0.03) and scored worse on the Multidimensional Impact (MICRA) Questionnaire (36.1 vs. 28.9 p=0.03). Women with recurrent phenotypes report testing to inform: (1) reproductive decisions, 2) personal and spousal health. By contrast, women with the incident affected pregnancy were more hopeful about: (1) immediate diagnosis, (2) advancing science and “helping others,” and (3) personal reassurance or “closure.” Thus, women pursuing ES in the setting of recurrent anomalous phenotypes may be motivated differently than those with a single affected pregnancy and may be more impacted by test-related uncertainty.
(Click here for large version)
Associations between Third Trimester Maternal Leptin, C-Peptide, Vascular Endothelial Growth Factor (VEGF), and Placental Growth Factor (PIGF) Levels and Development of Hypertensive Disorders of Pregnancy (HDOP) in Women with Type 2 Diabetes Mellitus (T2DM)
This study is to determine the association between maternal third trimester biomarker levels and development of hypertensive disorders of pregnancy (HDOP) among women with type 2-diabetes mellitus (T2DM). We performed a case-control study of data from a multicenter clinical trial of pregnant women with T2DM randomized to insulin plus metformin or insulin alone. Women had blood collected between 24 and 30 weeks’ gestation as study protocol. Maternal serum leptin, c-peptide, VEGF, and PIGF levels were measured and our primary outcome was hypertensive disorder of pregnancy (HDOP) (gestational hypertension or pre-eclampsia). We determined the association between third trimester biomarkers, HDOP, delivery, and neonatal outcomes using t-test, chi-square, and logistic regression. We have data on 236 women, 84 (36%) cases and 152 (64%) controls. Compared to controls, cases were more frequently African American (44.1% vs. 29.6%, p=0.03) or had chronic hypertension (33.3% vs. 19.7%, p=0.02). Additionally, cases delivered earlier (mean 36.2 (SD 2.6) vs. 37.0 (SD 2.7) weeks, p=0.03) and were more likely to have 5 minute APGAR <7 (31% vs. 15.8%, p=0.006). Biomarkers were not different between cases and controls. In regression models, biomarkers were not associated with HDOP. Mothers of newborns requiring NICU admission or oxygen supplementation had higher leptin levels (p=0.005, p=0.004, respectively). C-Peptide levels were higher among mothers of neonates with 5 minute APGAR <7 (p=0.02). Thus, third trimester leptin and c-peptide levels may impact immediate neonatal birth outcomes, particularly respiratory drive. A larger sample size (n=352) would be powered to detect a leptin-mediated difference.
(Click here for large version)
Contact: asha_talati@med.unc.edu
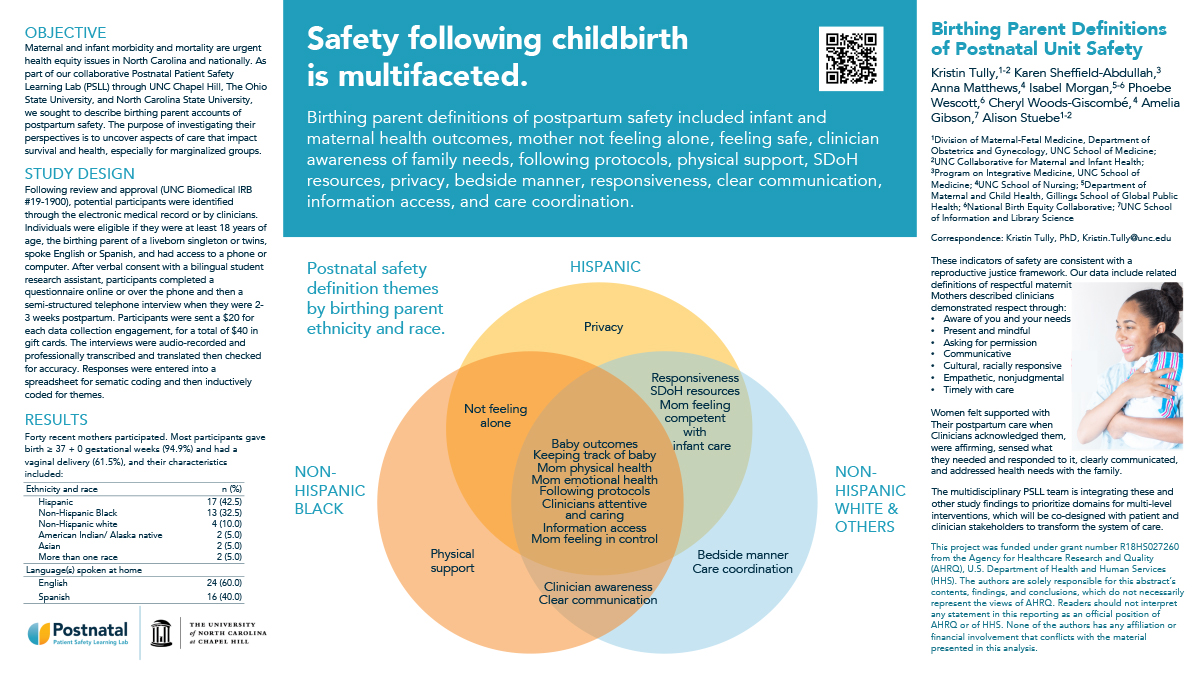
Birthing Parent Definitions of Postnatal Patient Safety
Kristin Tully, PhD
 Dr. Kristin Tully is a Research Assistant Professor in the Department of Obstetrics and Gynecology at the University of North Carolina at Chapel Hill. She is also a member of the UNC Collaborative for Maternal and Infant Health. Her doctorate is in Medical Anthropology and she completed an NICHD-supported postdoc through the Carolina Consortium on Human Development through the Duke University School of Nursing.
Dr. Kristin Tully is a Research Assistant Professor in the Department of Obstetrics and Gynecology at the University of North Carolina at Chapel Hill. She is also a member of the UNC Collaborative for Maternal and Infant Health. Her doctorate is in Medical Anthropology and she completed an NICHD-supported postdoc through the Carolina Consortium on Human Development through the Duke University School of Nursing.
Kristin seeks to transform perinatal care so that birthing parents and their families are treated in the ways they deserve and are supported in realizing their health goals.
Her collaborative program of research is currently supported by the Agency for Healthcare Research and Quality, the National Institutes of Health, the Patient Centered Outcome Research Institute, and the U.S. Health Resources & Services Administration to address mechanisms underlying “4th Trimester” outcomes such patient safety, breastfeeding, sleep practices, and maternal health. The objective is to enable more patient- and family-centered care, which is achieved by partnering with diverse stakeholders to identify unmet health needs and then co-develop sustainable solutions.
Birthing parent definitions of postnatal patient safety
Tully KP,1,2 Sheffield-Abdullah K,3 Matthews A,4 Morgan I, Wescott P,5 Woods Giscombé C,4 Gibson A,6 Stuebe AM1,2
1. Collaborative for Maternal and Infant Health, UNC School of Medicine; 2. Department of Obstetrics and Gynecology, UNC School of Medicine; 3. Program on Integrative Medicine, UNC School of Medicine; 4. UNC School of Nursing; 5. National Birth Equity Collaborative; 6. UNC School of Information and Library Science
Maternal and infant morbidity and mortality are urgent health equity issues in North Carolina and nationally. A key objective of the AHRQ-funded Postnatal Patient Safety Learning Laboratory was to define safety from the perspectives of birthing parents. The purpose was to identify their accounts of aspects of care that impact both survival and health.
Following review and approval (UNC Biomedical IRB #19-1900), potential participants were identified through the electronic medical record or by clinicians. Individuals were eligible if they were at least 18 years of age, the birthing parent of a liveborn singleton or twins, spoke English or Spanish, and had access to a phone or computer. After verbal consent with a bilingual student research assistant, participants completed a questionnaire online or over the phone and then a semi-structured telephone interview when they were 2-3 weeks postpartum. The 40 interviews were audio-recorded and professionally transcribed and translated then checked for accuracy. Responses were entered into a spreadsheet for sematic coding and then inductively coded for latent themes.
Patient definitions of safety included outcomes such as whether the baby is well and the mother is physically and emotionally healthy and safety was also: a feeling (emotional/affective response), action/process/behavior (such as keeping track of the baby and clinicians following protocols), access to resources, privacy/agency/control.
The multidisciplinary team across UNC Chapel Hill, The Ohio State University, and North Carolina State University is integrating these and other study findings to prioritize domains for multi-level interventions, which will be co-designed with stakeholders.
(Click here for large version)
Contact: kristin.tully@unc.edu
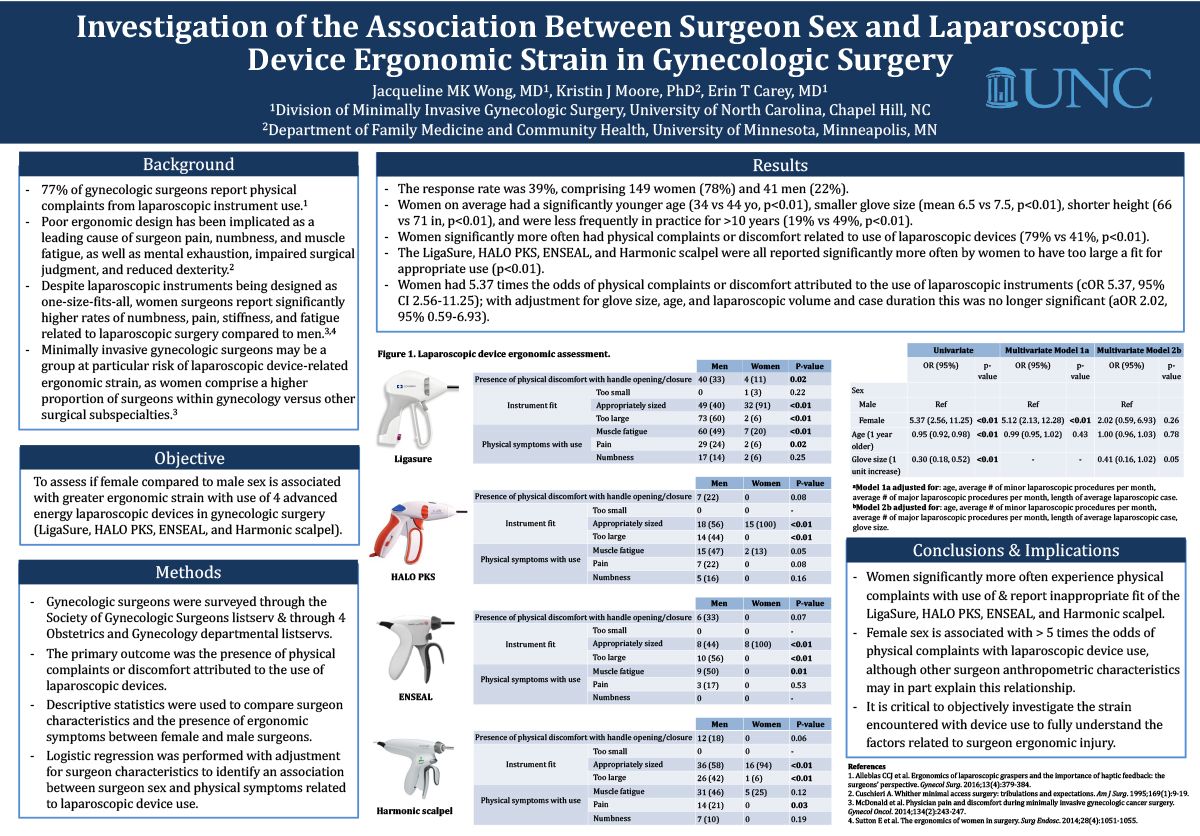
Investigation of the Association Between Surgeon Sex and Laparoscopic Device Ergonomic Strain in Gynecologic Surgery
Jacqueline Wong, MD
 Jackie Wong is in the last year of her fellowship training in Minimally Invasive Gynecologic Surgery and Chronic Pelvic Pain at the University of North Carolina. She attended medical school at Northwestern University in Chicago, IL and went on to complete her residency in Obstetrics and Gynecology at Northwestern University. Throughout her fellowship, she has concurrently completed a Master of Science in Clinical Research at the Gillings School of Public Health at the University of North Carolina. Dr. Wong has particular research interests in surgical technology and ergonomics, sex disparities in medicine, and the multimodal treatment of chronic pelvic pain. Her clinical interests include holistic care for medically and surgically complex patients and long-term solutions for chronic pain. Outside of work, she enjoys cooking, sharing time with loved ones, and exploring the outdoors with her partner and puppy.
Jackie Wong is in the last year of her fellowship training in Minimally Invasive Gynecologic Surgery and Chronic Pelvic Pain at the University of North Carolina. She attended medical school at Northwestern University in Chicago, IL and went on to complete her residency in Obstetrics and Gynecology at Northwestern University. Throughout her fellowship, she has concurrently completed a Master of Science in Clinical Research at the Gillings School of Public Health at the University of North Carolina. Dr. Wong has particular research interests in surgical technology and ergonomics, sex disparities in medicine, and the multimodal treatment of chronic pelvic pain. Her clinical interests include holistic care for medically and surgically complex patients and long-term solutions for chronic pain. Outside of work, she enjoys cooking, sharing time with loved ones, and exploring the outdoors with her partner and puppy.
Investigation of the Association Between Surgeon Sex and Laparoscopic Device Ergonomic Strain in Gynecologic Surgery
Objective: To assess if female compared to male sex is associated with greater ergonomic strain with use of 4 advanced energy laparoscopic devices in gynecologic surgery (LigaSure, HALO PKS, ENSEAL, and Harmonic scalpel).
Study Design: Gynecologic surgeons were surveyed through the Society of Gynecologic Surgeons listserv and 4 Obstetrics/Gynecology departmental listservs. The primary outcome was the presence of physical complaints attributed to use of laparoscopic devices. Descriptive statistics compared surgeon characteristics and ergonomic symptoms by surgeon sex. Logistic regression was performed with adjustment for factors including surgeon glove size.
Results: The response rate was 39%, comprising 149 women (78%) and 41 men (22%). Women had a significantly younger age (mean 34 vs 44yo, p<0.01), smaller glove size (mean 6.5 vs 7.5, p<0.01), and shorter height (median 66 vs 71in, p<0.01). Women significantly more often reported physical complaints from use of laparoscopic devices (79% vs 41%, p<0.01). The LigaSure, HALO PKS, ENSEAL, and Harmonic scalpel were all reported significantly more often by women to have too large a fit for use (p<0.01). Women had 5.37 times the odds of physical complaints attributed to the use of laparoscopic instruments (cOR 5.37, 95% CI 2.56-11.25); with adjustment for surgeon glove size this was no longer significant (aOR 2.02, 95% 0.59-6.93).
Conclusions: Women significantly more often experience physical complaints with use of and inappropriate fit of the LigaSure, HALO PKS, ENSEAL, and Harmonic scalpel. Female sex is associated with over fivefold greater odds of physical complaints with laparoscopic device use, although other surgeon characteristics may partly explain this relationship.
(Click here for large version)
Contact: jmkwong@med.unc.edu