Research
We are committed to advancing innovative, high-quality geriatrics interprofessional education, research in geriatric medicine, and geriatric clinical care. In collaboration with the Center for Aging and Health, our overarching goal is to improve the health and well-being of the aging population across North Carolina and the nation.
Focus Areas
Research in the Division of Geriatric Medicine occurs in partnership with multiple Centers, Institutes, Divisions, Departments, and Schools at UNC. Furthermore, our faculty are Principal Investigators on research grants aimed at bringing critical evidence-based findings into healthcare practice to improve the care of older adults.
Alzheimer’s Disease and Related Dementias
The NIH-funded Duke University and the University of North Carolina Alzheimer’s Disease Research Center (Duke/UNC ADRC) brings together leading researchers in Alzheimer’s disease and related dementias across two major research institutions. Specifically, we aim to catalyze and support research, innovations in clinical care and academic work force development (with North Carolina Central University, East Carolina University and UNC Pembroke as partner institutions) in this field.
Ultimately, our purpose is to reduce the burden of Alzheimer’s disease and related dementias regionally and nationally. The outstanding scientific environment at both institutions enables novel research to identify effective methods of prevention and/or early intervention, and to reduce racial and urban/rural disparities associated with dementia.
Workforce Education on Aging
The Carolina Geriatric Workforce Enhancement Program (GWEP) funded by HRSA, is led by Project Director, Jan Busby-Whitehead, MD. The CGWEP integrates geriatric principles and interprofessional teamwork to address the 4Ms of age-friendly health systems (What Matters to older adults, Medication, Mentation, and Mobility) and to address dementia-friendly care. Academic partners and NC AHECs are providing both in person and virtual training and consultation to tribal organizations, rural and underserved primary care sites to better integrate age-friendly and dementia-friendly content into practices and health care systems.
Delirium Research
 Center for Aging and Health Director Dr. Jan Busby-Whitehead is Co-Investigator and Dissemination Task Force Co-Leader for the NIA’s Network for the Investigation of Delirium: Unifying Scientists (NIDUS). NIDUS gathers data on all delirium research, grants, and studies worldwide, and advocates to advance delirium research and understanding. NIDUS has five Cores:
Center for Aging and Health Director Dr. Jan Busby-Whitehead is Co-Investigator and Dissemination Task Force Co-Leader for the NIA’s Network for the Investigation of Delirium: Unifying Scientists (NIDUS). NIDUS gathers data on all delirium research, grants, and studies worldwide, and advocates to advance delirium research and understanding. NIDUS has five Cores:
- Delirium Research Hub – Focuses on improving research collaboration
- Measurement & Harmonization – Develops delirium measurement resources
- Pilot Awards & Innovation – Encourages new delirium research
- Mentoring & Career Development – Trains and develops future delirium researchers
- Dissemination & Communication – Communicates news on delirium research
Dr. Adrian Austin (MD, MCSR) is a delirium researcher who is dually board certified in Geriatric Medicine and Critical Care / Pulmonary Medicine. Additionally, he has two pilot projects on delirium: a tablet-based delirium assessment tool for home use and a pharmacogenomic study of dose and response variability among mechanically ventilated ICU patients.
Deprescribing
As adults age, it is important to reconsider the risks and benefits of medications. Many medications that were once appropriate no longer hold the same benefit as the risk for side effects increases. Deprescribing is the gradual reduction of medications when the benefits no longer outweigh the potential harms. Undoubtedly, it is a cornerstone of geriatrics clinical practice to optimize care for older adults. Deprescribing is a rapidly growing area of research in geriatric medicine. As such, the Division of Geriatrics, and the Center for Aging and Health is quickly becoming a hub these projects.
Stefanie Ferreri, PharmD, Vice Chair of the Division of Practice Advancement and Clinical Education at the UNC Eshelman School of Pharmacy and Geriatric Medicine Division Chief Jan Busby-Whitehead, MD, are co-Principal Investigators of a CDC-funded grant on screening older adults who use prescription opioids and are at risk for falls. The study will engage patients 65 years and older within the UNC Health Care system. Specifically, these are patients who are taking either an opioid or benzodiazepine. Accordingly, a centralized team of clinical pharmacists will screen patients. In the end, the team will provide recommendations on deprescribing these medications with the goal of reducing the risk for future falls.
Dr. Ferreri also led a 2016 CDC-funded grant on implementing an integrative falls prevention program for which Dr. Busby-Whitehead is a Co-Investigator. This work led to the development of STEADI-Rx. This guide helps improve collaboration between prescribers and pharmacists to screen patients and intervene to reduce falls risk.
Physical Function and Obesity in Older Adults
Learn more about Dr. John Batsis, his team, and their research on Physical Function, Obesity, and other topics.
Palliative Care
With funding from a Tier 2 Clinical / Translational Award from the UNC Lineberger Comprehensive Cancer Center, Laura Hanson, MD, MPH, and other Geriatrics, Palliative Care and Oncology faculty have developed and begun testing a collaborative palliative care model for patients with Stage IV cancer. Specifically, the research tests an innovative approach to support continuity of care between inpatient and outpatient providers. It also facilitates efficient and targeted use of specialty Palliative Care.
With funding from the Gordon and Betty Moore Foundation, Chrissy Kistler, MD, and Laura C. Hanson, MD, are Co-Principal Investigators for a 2-year project on Improving Primary Care Clinicians’ Communication Skills in Dementia Palliative Care. Advance care planning decisions are particularly challenging in the context of Alzheimer’s disease and related neurodegenerative dementias. These diseases last for years yet affect cognitive and communication abilities early in the disease course.
This project addresses the gap in dementia-specific advance care planning and medical treatment decisions for clinicians who provide primary care. Specifically, the training uses 4 video-based advance care planning scenarios and an accompanying training toolkit. Furthermore, trained clinicians are assessed for actual application of these skills in their clinical encounters. In addition, the training modules are disseminated through collaboration with Vital Talk.
Aging Research Training Programs
The UNC Geriatric Oncology Training Program (UNC-GO) is a T32 training application specifically focused on training physicians (MDs, DOs). The focus is clinical/translational and/or health services research at the interface of Geriatrics and Oncology. The central component of UNC-GO training is the mentored research experience. Trainees choose between two research tracks that represent the best research areas that UNC has to offer. Furthermore, these two tracks are clinical/translational research and health services research. Additionally, under the guidance of the mentoring team, trainees design and conduct one or more independent projects.
Dr. Hyman Muss, Vice Chair of Hematology/Oncology and Dr. Jan Busby-Whitehead, Geriatric Medicine Division Chief, are Co-Principal Investigators and lead the Geriatric Oncology Program. This program trains fellows in Medical Oncology and Geriatric Medicine through several pathways.

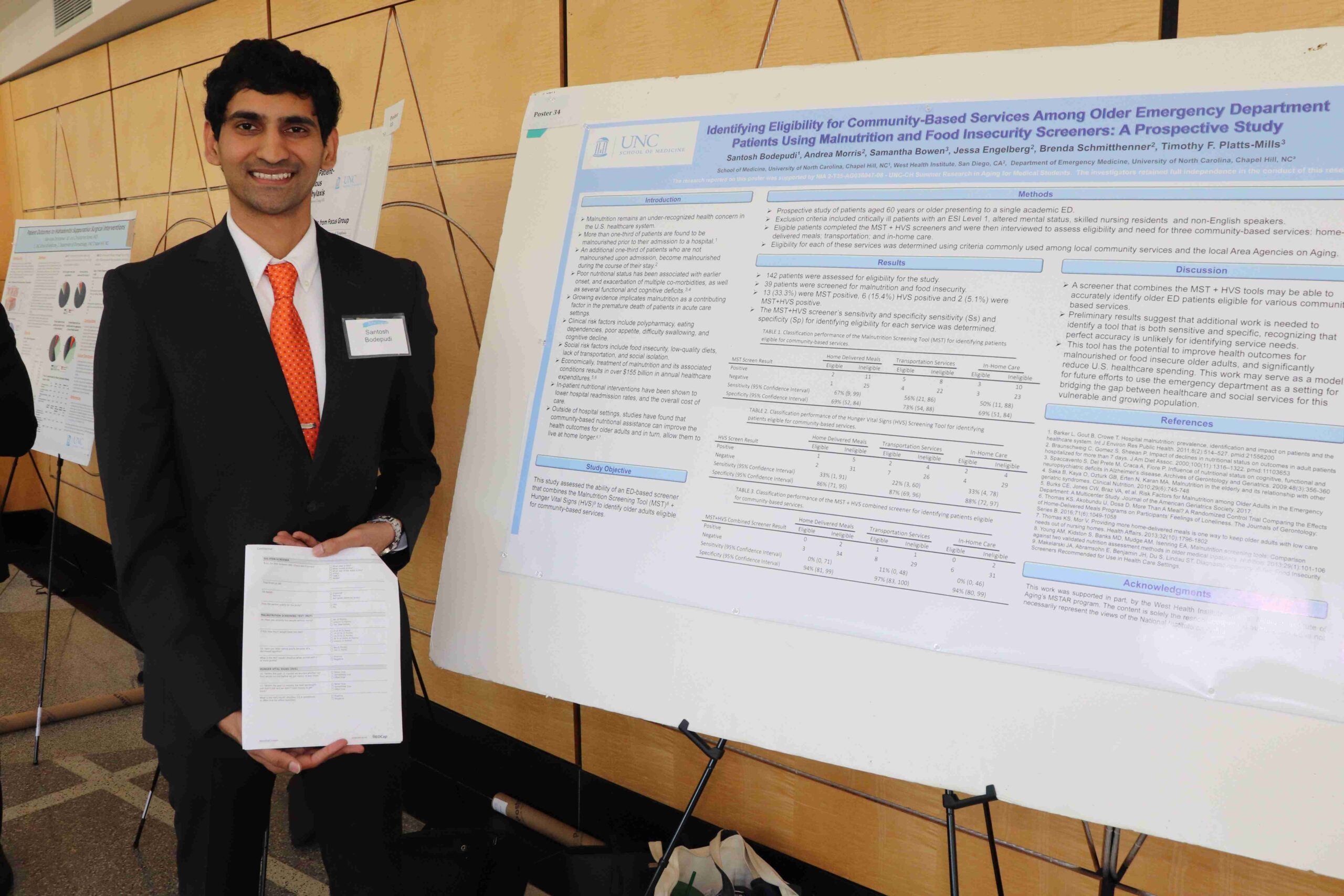
UNC’s Division of Geriatric Medicine is one of seven national Medical Students Training in Aging Research (MSTAR) training centers. It has been funded since 2010. The National Institute on Aging (NIA) sponsors this program to connect medical students with mentored research opportunities and academic experiences. Mentorship helps to advance students’ knowledge of aging. It also exposes them to broad possibilities for basic science, clinical, and health services research.