Team Approach Engages Residents in Quality Improvement
In the American College of Graduate Medical Education (ACGME)’s new milestones era, the Practice-based Learning and Improvement Milestone requires “incorporation of quality improvement (QI) and patient safety initiatives into personal practice.” Since the 2012-2013 academic year, Vice Chair for Education, Dr. Harendra Arora has worked with PSQI-involved faculty members to assign clinical anesthesia (CA)-2 residents to faculty-led, team-based Patient Safety and Quality Improvement (PSQI) projects that teach them perioperative process improvement.


(L to R) Dr. Jessica Hodnett (CA-2) and Dr. Daniel Rosenkrans (CA-3) participated in a team-based PSQI project to develop best practice guidelines.
Arora noted: “Incorporating a team-based QI project into our resident academic curriculum has helped give our residents the unique opportunity to systematically identify problem areas in the clinical arena, implement a change and measure the impact of that change.”
In UNC School of Medicine (SOM)’s Institute for Healthcare Quality Improvement (IHQI) 2015-2016 seed grant cycle, the IHQI’s Improvement Scholars Program awarded Assistant Professor Dr. Greg Balfanz and Associate Professor Dr. Peggy McNaull $50K to carry out their proposal – “Implementation of an Updated UNC Hospitals Standard Surgical Blood Order Schedule and UNC Intraoperative Blood Product Transfusion Best Practice Guidelines.” Drs. Jessica Hodnett (then CA-2), Daniel Rosenkrans (then CA-1) and Joe Piscitello (then CA-3) all signed on, eager to learn intraoperative PSQI principles via participating in best practice guidelines development and implementation.
Approved Improvement Scholars Program projects are expected to improve a patient population’s clinical care and outcomes by implementing proven and/or expert-recommended strategies and approaches. To meet this aim, Balfanz and McNaull partnered with UNC’s Departments of Urology and Transfusion Medicine, using Urology’s large volume of high blood utilization cases (eg, cystectomy). If the pilot best practice guidelines could reduce transfusion rates, they could potentially be spread across all adult surgical cases at UNC.
From October 2015-April 2016, newly developed best practice guidelines were applied to all Urology cases. In comparing post-intervention case data (N=326) with its counterpart from a longer pre-intervention (April 2014-January 2015) period (N=529), the faculty/resident team examined two main metrics – 1) units of blood transfused intraoperatively; and 2) intraoperative nadir hemoglobin (nHb) levels. The Department’s PSQI Manager Nathan Woody then applied Process Sigma Calculation – a QI-driven data analysis approach to reduce variation, associated defects, wastes and risks in any process – to analyze pre- and post-intervention transfusion rates. Analysis showed a significant pre-/post-intervention reduction in transfusion rate (-7.7%), prompting implementation of the best practice guidelines across all adult Enhanced Recovery After Anesthesia (ERAS) programs within UNC.
Hodnett presented her experience learning PSQI principles and their results at the American Society of Anesthesiologists 2016 Annual Meeting. Now a CA-3, Rosenkrans shared his thoughts reflecting a trainee’s early-career exposure to identifying and developing ways to use PSQI principles to improve patient outcomes:
“When I started this project, it was hard to imagine how providing guidelines might change practices at our hospital. Now that [the best practice guidelines] have functioned for some time, it’s rewarding to receive periodic updates showing a reduction in transfusions. I learned that creating a system such as this requires many multidisciplinary conversations and the flexibility to overcome inevitable bumps along the road.”
Emphasizing the importance of PSQI education, Arora concluded: “Through the [team-based], systematic engagement of residents and faculty, the Department has cultivated a culture supporting QI which further encourages everyone to work toward the common goal of improved patient care and safety. This exercise prepares them for a future in healthcare delivery that is cost-effective, efficient, outcomes-based, and patient-centered.”
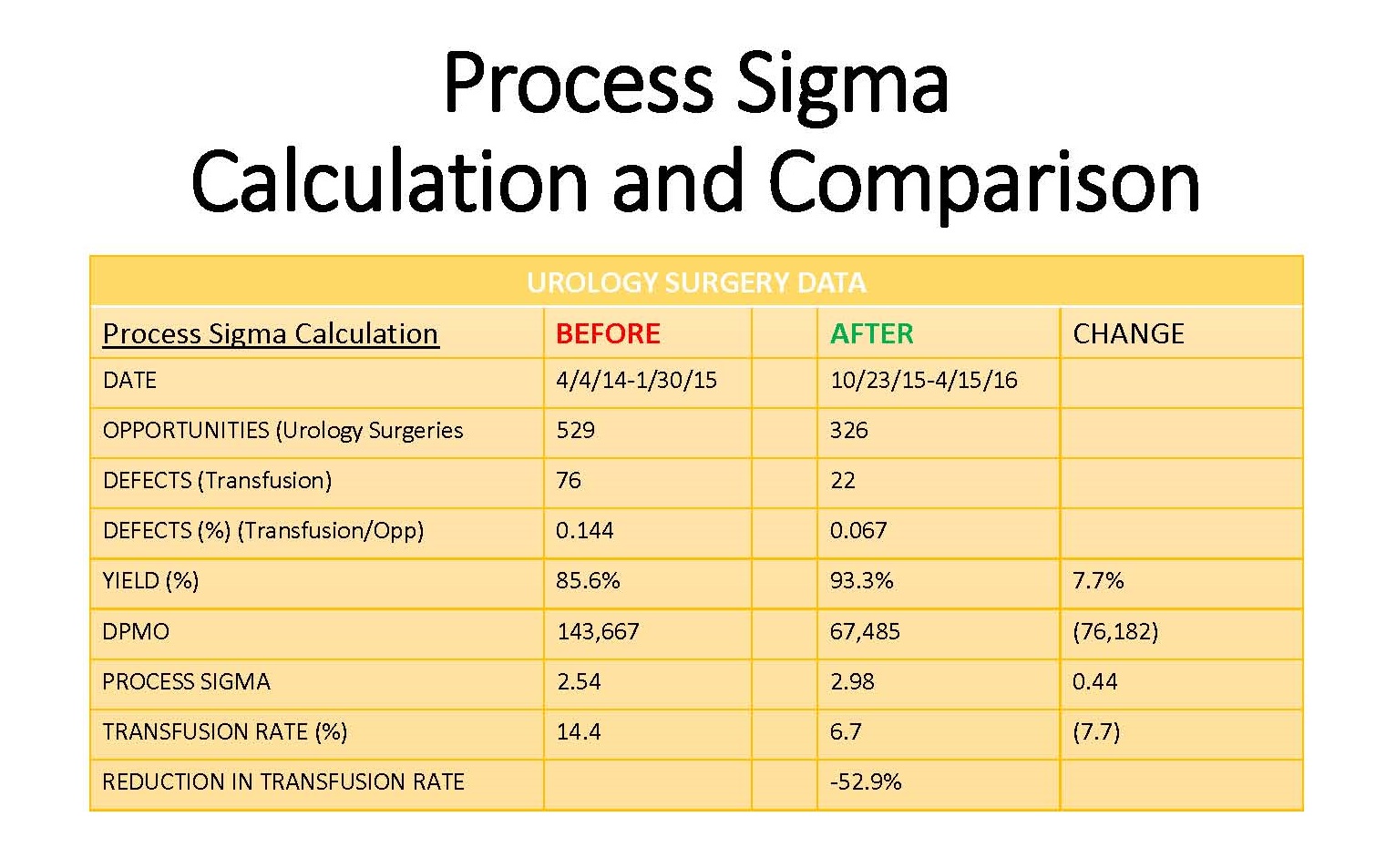 Data analysis accounting for process defects and waste (Process Sigma Calculation) indicated pilot best practice guidelines helped reduce transfusion rates in high blood utilization Urology cases. Reduced rates provided a means for broadly implementing these guidelines across adult Enhanced Recovery After Anesthesia (ERAS) programs at UNC Hospitals.
Data analysis accounting for process defects and waste (Process Sigma Calculation) indicated pilot best practice guidelines helped reduce transfusion rates in high blood utilization Urology cases. Reduced rates provided a means for broadly implementing these guidelines across adult Enhanced Recovery After Anesthesia (ERAS) programs at UNC Hospitals.