Poster Presentation & Awards
The UNC Center for Women’s Health Research is continually seeking ways to promote the essential work being done by investigators in alignment with our mission: Learning about diseases, disorders, and conditions that uniquely affect women, predominantly affect women, and affect women differently than men.
To that end, coinciding with National Women’s Health Week, we are proud to present our third Women’s Health Research Poster Presentation & Awards Program to stimulate and showcase research being done by faculty and staff, graduate and undergraduate students, and postdocs (residents and fellows) of UNC-Chapel Hill and to encourage networking and multidisciplinary collaborations.
Abstracts were reviewed and judged on the following criteria: Impact to the delivery of health care in North Carolina; the evaluation of sex as a biological variable; multidisciplinary science; impact on health equity; and overall scientific value.
Keep scrolling to view this year’s submissions and award winners! Our sincere thanks to all who shared their research for this program as well as our abstract jury who volunteered their time to assist us in the awards process.
CWHR is also excited to use this event as an opportunity to promote the UNC Women’s Health Multidisciplinary Consortium, whose mission is “Creating a trainee-focused, unified community of faculty, clinicians, and researchers with a vested interest in advancing the health of women at UNC.”
To get more information and stay updated on the group’s activities, please fill out the Interest Form. You can also follow the Women’s Health Multidisciplinary Consortium on Twitter. The WHMC is currently being supported by CWHR and the Department of Pathology and Laboratory Medicine, but anyone with an interest in women’s health research from any UNC program or department is encouraged to get involved!
2023 Award Recipients
Best Poster by an Undergraduate Student
Single-Visit LARC Initiation Among Adolescents Before and During COVID-19
Ananya Tadikonda
Contact: ananyat@live.unc.edu
 Ananya is a senior undergraduate student and Morehead-Cain Scholar studying health policy and management and biology at the University of North Carolina at Chapel Hill. She started working as a research assistant in the UNC School of Medicine Division of Family Planning during the Spring of her first year at UNC, under the mentorship of Dr. Gretchen Stuart. While working on her first project examining college student abortion access, Ananya became further interested in adolescent reproductive health and began conducting research with Dr. Bianca Allison on adolescent contraceptive decision aids and LARC access for adolescents. Ananya is also interested in advancing healthcare payment and delivery system reform, and has contributed to a project called “North Carolina Integrated Care for Kids”. This project aims to create a novel payment and care delivery model for Medicaid-insured patients in five North Carolina counties that integrates social determinants of health such as housing, food security, and Kindergarten readiness. This has inspired Ananya to address the upstream barriers to health and well-being. During Summer 2022, Ananya interned at the Centers for Disease Control and Prevention in the Division of Reproductive Health, specifically on the Adolescent/Young Adult Team and the Fertility Epidemiology Studies Team. Through this experience, she enjoyed learning about the intersections between health services research, health policy, and care delivery innovation. Ananya will continue her learning journey in medical school next year, where she aspires to further explore her interests in reproductive health, adolescent medicine, primary care pediatrics, and health policy.
Ananya is a senior undergraduate student and Morehead-Cain Scholar studying health policy and management and biology at the University of North Carolina at Chapel Hill. She started working as a research assistant in the UNC School of Medicine Division of Family Planning during the Spring of her first year at UNC, under the mentorship of Dr. Gretchen Stuart. While working on her first project examining college student abortion access, Ananya became further interested in adolescent reproductive health and began conducting research with Dr. Bianca Allison on adolescent contraceptive decision aids and LARC access for adolescents. Ananya is also interested in advancing healthcare payment and delivery system reform, and has contributed to a project called “North Carolina Integrated Care for Kids”. This project aims to create a novel payment and care delivery model for Medicaid-insured patients in five North Carolina counties that integrates social determinants of health such as housing, food security, and Kindergarten readiness. This has inspired Ananya to address the upstream barriers to health and well-being. During Summer 2022, Ananya interned at the Centers for Disease Control and Prevention in the Division of Reproductive Health, specifically on the Adolescent/Young Adult Team and the Fertility Epidemiology Studies Team. Through this experience, she enjoyed learning about the intersections between health services research, health policy, and care delivery innovation. Ananya will continue her learning journey in medical school next year, where she aspires to further explore her interests in reproductive health, adolescent medicine, primary care pediatrics, and health policy.
Single-Visit LARC Initiation Among Adolescents Before and During COVID-19
Same-day long-acting reversible contraception (LARC) is cost-effective and convenient. We aimed to determine the patient- and provider-level factors associated with same-day LARC placement for adolescents 12 months before and after COVID-19 protocols began.
This retrospective cohort study analyzed electronic health records from UNC Health. Adolescents included (N=954) were 10-19 years old and received outpatient LARC from 3/15/2019 to 3/14/2021. A logistic regression model determined the relationship of multiple variables on receipt of same day LARC before and during COVID-19. An interrupted time series examined changes in same-day LARC initiation during the 12 months before and after 3/15/2020. Our institutional IRB approved the study.
There was no significant change in average monthly same-day LARC insertions before and after 3/15/2020 (p>0.05). County concordance was associated with same-day LARC both before and during the pandemic (aOR=2.31 and 1.83 respectively, both p<0.05). During the pandemic, a few factors reduced the odds of same-day LARC :1) public insurance (aOR=0.52, p<0.01, vs. private insurance), 2) non-OBGYN providers (pediatrics [aOR=0.34, p<0.01], family medicine [aOR=0.53, p<0.01] or internal medicine [aOR=0.13, p<0.05], vs. OBGYN), and 3) advanced practice practitioners (aOR=0.46, p<0.001, vs. physicians).
We identified differences in adolescent same-day LARC initiation during the pandemic by county concordance, insurance status, provider specialty, and provider type. Some potential explanations include barriers to accessing clinical care (i.e. appointment availability, transportation), and non-LARC concerns taking priority at in-person primary care visits during the pandemic. Findings from this study may guide policy and programmatic interventions to improve access to same-day LARC for all adolescents.

Click here for large version
Best Poster by a Graduate Student, Resident, or Fellow – Tie
Contraception, but possibly not estrogen, is related to thrombosis risk in women with sickle cell disease
Jennifer Newcome, MD
Contact: jennifje@email.unc.edu
I am a third-year pediatric hematology/oncology fellow at the University of North Carolina. My MD was obtained at the University of Arkansas for Medical Sciences, and I did my residency at East Carolina University in internal medicine and pediatrics. My clinical interests include benign hematology conditions, specifically sickle cell disease and women’s health. I am also interested in the transition care of patients moving from pediatric to adult care. My research interests are the intersection of sickle cell disease, contraception, and thrombosis. The first part of my research involves analyzing thrombosis markers in women with sickle cell disease who are initiating contraception and at a steady state. The second part is a retrospective review of women with sickle cell disease looking at the relationship between thrombosis with contraception. When I am not practicing medicine, I love spending time with my husband and dog, attending church, and running half marathons.
Contraception, but possibly not estrogen, is related to thrombosis risk in women with sickle cell disease
Estrogen-containing hormonal contraception (HC) is a well-established risk factor for venous thromboembolism (VTE). Women with sickle cell disease (SCD) also have increased VTE risk, but whether estrogen-containing HC contributes to this risk is unclear. This study aimed to compare the incidence of VTE in women with SCD on and off estrogen-containing HC. We analyzed a retrospective cohort of female patients with SCD between 15 and 65 years old seen at the University of North Carolina between 2010 to 2022. Out of 438 female patients with SCD, 114 (26.9%) patients had VTE. Of the 245 (55.9%) patients on any type of HC, 39 (15.9%) had a VTE while taking HC, and 10 (4.1%) had a VTE while on estrogen-containing HC. The adjusted OR for risk of VTE with any contraception use was 2.029 (95% CI 1.118, 3.464) (p=0.0095), while the adjusted OR for estrogen-containing HC was 1.024 (95% CI 0.502, 2.088). The thrombosis rate in women with SCD is higher in this single-center population than in other studies. HC use in any form at any time was associated with an increased rate of VTE, although estrogen-containing HC did not seem to be associated with an increased risk for VTE. s work contributes to our understanding of how HC affects VTE risk in women with SCD. Future studies investigating the impact of concurrent contraception use and coexisting risk factors on the incidence of VTE can further elucidate treatment guidelines for this population.

Click here for large version
Sterilization in the childfree population: an exploratory study
Ashley Parker, MBS
Contact: ashley_parker@med.unc.edu
 Originally from Rhode Island, Ashley made her way to North Carolina in 2010 to attend Davidson College. While at Davidson she majored in French and Francophone Studies, which led her to spend a year after college teaching English to elementary school children in France. Ashley worked in pediatrics, gynecologic oncology, and anesthesiology research, and earned a Master of Biomedical Science at Duke University before beginning medical school at UNC. While at UNC she conducted a quality improvement project on screening for intimate partner violence in a primary care clinic, researched sterilization in childfree people, and served as a student provider in the SHAC Gender Affirming Care Clinic. Outside of work, she enjoys running, listening to podcasts, baking cakes for friends, and watching NYT Cooking videos. She graduates in May 2023 and is excited to start her residency in OB/GYN at Brigham and Women’s Hospital/Massachusetts General Hospital this summer.
Originally from Rhode Island, Ashley made her way to North Carolina in 2010 to attend Davidson College. While at Davidson she majored in French and Francophone Studies, which led her to spend a year after college teaching English to elementary school children in France. Ashley worked in pediatrics, gynecologic oncology, and anesthesiology research, and earned a Master of Biomedical Science at Duke University before beginning medical school at UNC. While at UNC she conducted a quality improvement project on screening for intimate partner violence in a primary care clinic, researched sterilization in childfree people, and served as a student provider in the SHAC Gender Affirming Care Clinic. Outside of work, she enjoys running, listening to podcasts, baking cakes for friends, and watching NYT Cooking videos. She graduates in May 2023 and is excited to start her residency in OB/GYN at Brigham and Women’s Hospital/Massachusetts General Hospital this summer.
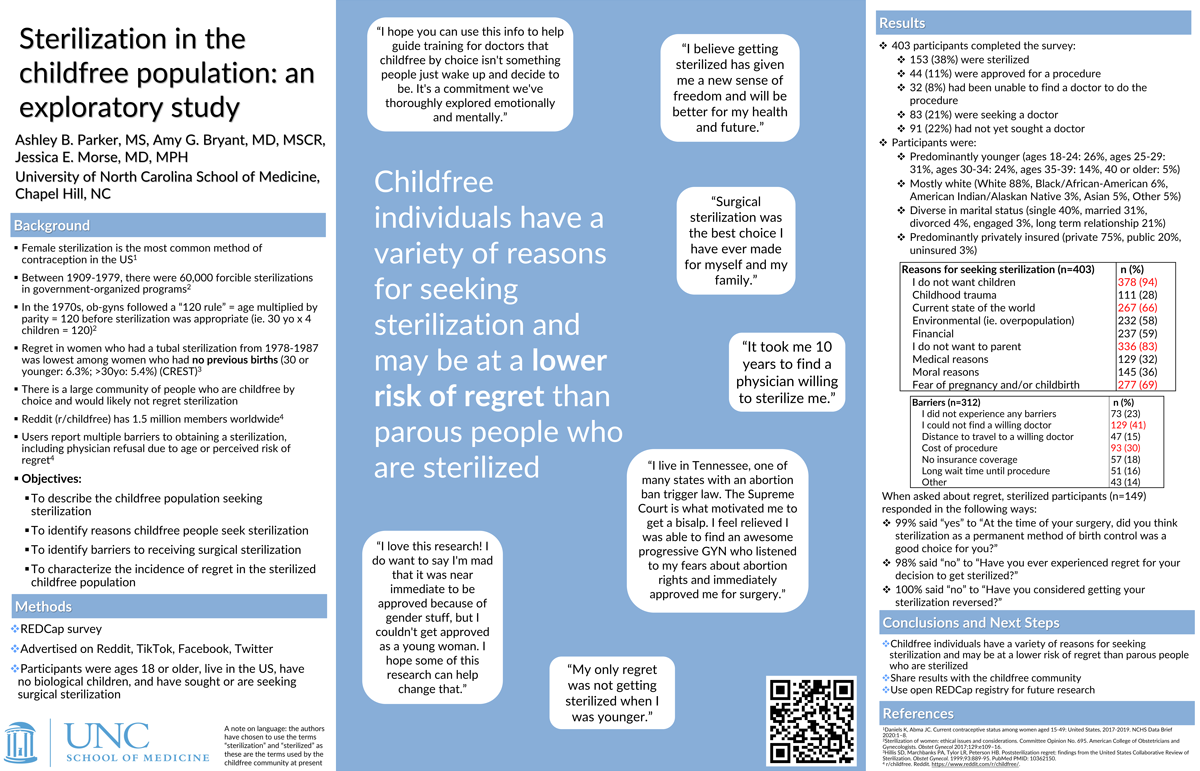
Sterilization in the childfree population: an exploratory study
Authors: Ashley B. Parker, MS, Amy G. Bryant, MD, MSCR, Jessica E. Morse, MD, MPH
Affiliation: University of North Carolina School of Medicine, Chapel Hill, NC
Objectives: To describe the childfree population seeking surgical sterilization, identify barriers to receiving care, and characterize the incidence of regret.
Methods: We conducted an exploratory survey of people in the US, 18 years and older, who do not have biological children, and who are seeking or have previously sought a sterilization procedure. Participants completed an online REDCap survey distributed over social media platforms, including Reddit, TikTok, and Facebook.
Results:
403 respondents completed the survey, of whom 153 (38%) were sterilized, 44 (11%) were approved for a procedure, 32 (8%) had been unable to find a doctor to do the procedure, 83 (21%) were seeking a doctor, and 91 (22%) had not yet sought a doctor.
Respondents were predominantly white (88%), identified as women (82%), and were diverse in sexual orientation (heterosexual 41%, bisexual 41%, other 18%). Reasons for seeking sterilization included not wanting children (94%), fear of pregnancy/childbirth (69%), the current state of the world (66%), environmental reasons (58%), and medical reasons (32%). Barriers to care included cost of the procedure (30%) and inability to find a doctor who would perform the procedure (41%).
Of the 149 respondents who had been surgically sterilized, 68 (46%) asked more than one doctor for the procedure. Of those sterilized, 99.3% answered “yes” to “Do you think sterilization as a permanent method of birth control was a good choice for you?”
Conclusions: Childfree individuals have a variety of reasons for seeking sterilization and may be at a lower risk of regret than parous people who are sterilized.
Click here for large version
Best Poster by Faculty or Staff
Trans*-affirming Care for New Reproductive Health Nurses
Rhonda Lanning, DNP, CNM, LCCE, IBCLC, RN
Contact: rlanning@unc.edu
Rhonda Lanning (she/her) is an Associate Professor at the University of North Carolina at Chapel Hill School of Nursing and the Program Director for Birth Partners, the volunteer doula program for UNC Medical Center. Trained as a Certified Nurse Midwife and International Board-Certified Lactation Consultant, Dr. Lanning has worked for more than 20 years in reproductive health care. She is the recipient of numerous teaching and service awards, including the UNC Medical Center Nurse Faculty of the Year, the Provost’s Award for Engaged Teaching and the Tanner Award for Excellence in Undergraduate Teaching at UNC-Chapel Hill. In 2021, she was selected as a Carolina Center for Public Service Thorp Faculty Engaged Scholar. Dr. Lanning has been the recipient of several grants, including funding to create an interdisciplinary service-learning course focused on training future health professionals as volunteer doulas. She has published and presented her innovative work, including the expansion of a hospital-based volunteer doula program to increase access to supportive maternity care, expanding doula services to the operating room, and incorporating doulas into the education of undergraduate nursing students. Dr. Lanning enthusiastically teaches and mentors students both within the School of Nursing and across several disciplines at UNC. She currently serves as the chair of the Baccalaureate Executive Committee. A first-generation college graduate, Dr. Lanning completed her BSN and MSN at the University of Pennsylvania and her Doctorate in Nursing Practice at Duke University. She can be reached at rlanning@unc.edu.
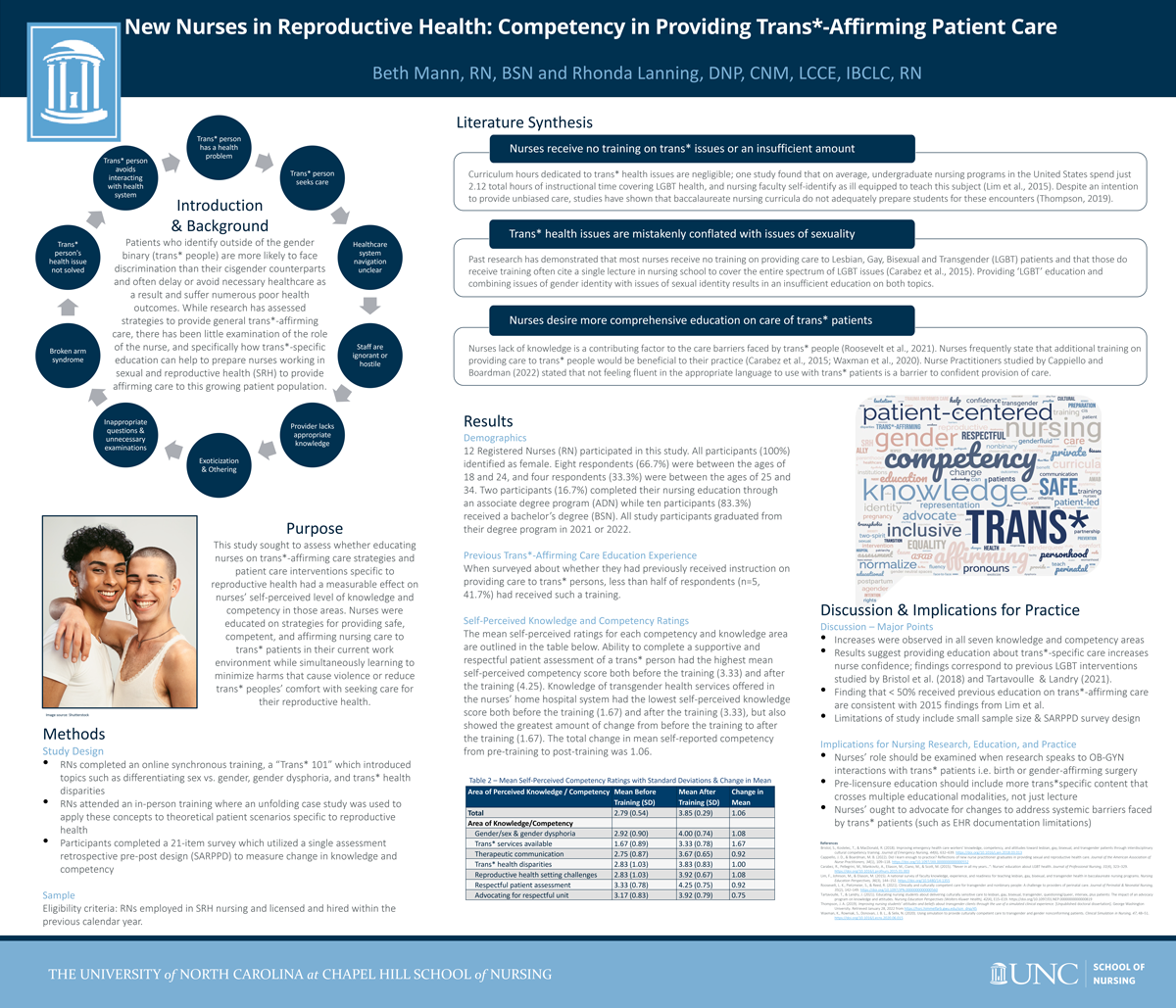
Trans*-affirming Care for New Reproductive Health Nurses
Patients who identify outside of the gender binary (trans* people) are more likely to face discrimination than their cisgender counterparts and often delay or avoid necessary healthcare as a result. While research has assessed strategies to provide general trans*-affirming care, there has been little examination of the role of the nurse and how trans*-specific education can help to prepare nurses working in sexual and reproductive health (SRH) to provide affirming care to this growing patient population. This study examines self-reported knowledge and competency among newly licensed Registered Nurses (RN) working in SRH after an educational intervention to teach trans*affirming care principles. RNs completed an online synchronous training, “Trans* 101” which introduced topics such as differentiating sex vs. gender, gender dysphoria, and health disparities. This was followed by an in-person training where an unfolding case study was used to apply these concepts to theoretical patient scenarios specific to reproductive health. Participants then completed a 21-item survey that utilized a single assessment retrospective pre-post design (SARPPD) to measure change in knowledge and competency. The results of the study suggest that nurses’ knowledge and competency with trans*-affirming care can be improved with educational intervention. All areas measured showed increases from pre-training to post-training. Nurses desire more knowledge on how to provide trans*-affirming care, and little education specific to trans* reproductive health is provided in pre-licensure educational curricula or unit training protocols; confidence in knowledge and competency increases after this type of education is provided.
Click here for large version
2023 Submissions
Black Female Adolescent Experiences with Reproductive Health Counseling In Primary Care: A Qualitative Study
Alessandra Angelino, MD, MPH
Contact: alessandra.angelino@unchealth.unc.edu
Alessandra Angelino MD, MPH (She/her) is a Pediatrics Resident at the University of North Carolina. She is pursuing an Adolescent Medicine fellowship at Johns Hopkins University starting July 2023 where she will focus her clinical, advocacy, and policy work on health equity, adolescent autonomy, Indigenous youth and adolescents, and gender diverse youth.
Dr. Angelino is passionate about health equity and public health, inspired by her undergraduate education at Georgetown University in International Health, her MPH in Global Health from the University of Washington, and her medical education at Rutgers Robert Wood Johnson Medical School. Her early educational experiences included working in an Aboriginal and Torres Strait Islander community in Australia, and formalizing connections with American Indian tribes and national Indigenous organizations in the US. These connections resulted in research and curricula development related to Two Spirit and gender diverse youth and adolescents, along with advocacy for Indigenous adolescents. She created the “Celebrating Our Magic Toolkit” and related publications which have been utilized globally as a tool for Indigenous Two Spirit and LGBTQ+ youth, parents, and healthcare providers.
During residency, Alessandra has continued to work with American Indian tribes, the Indian Health Service, and The Fenway Institute to create curricula and national guidelines related to Indigenous gender diverse youth. Her research and publications center on intersectionality, cultural connection and mental health outcomes, and community based participatory research. In the advocacy space, she is a liaison on the AAP’s Committee on Native American Child Health (CONACH) and serves to increase visibility for Indigenous youth and adolescents.
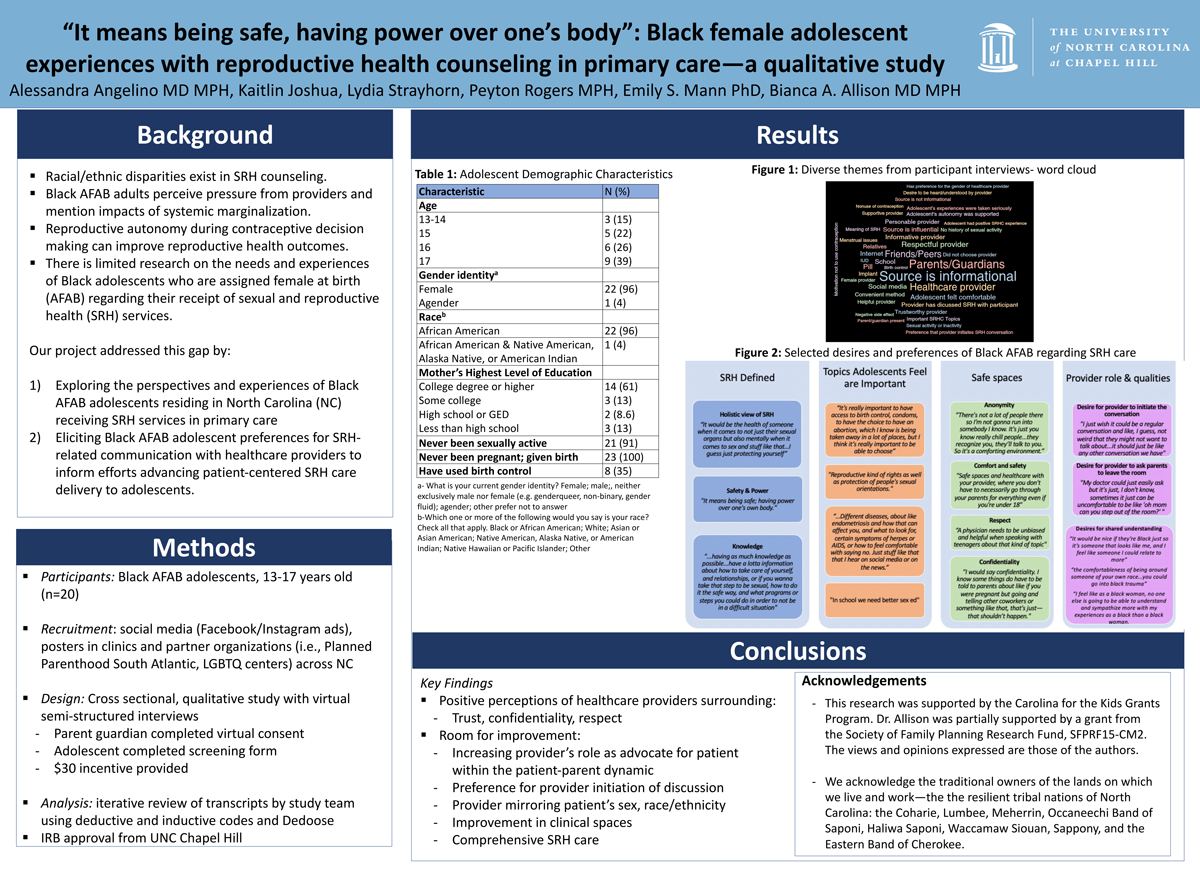
Black Female Adolescent Experiences with Reproductive Health Counseling In Primary Care: A Qualitative Study
Authors: Alessandra Angelino MD MPH, Kaitlin Joshua, Lydia Strayhorn BA, Peyton Rogers MPH, Emily Mann PhD, Bianca Allison MD MPH
There are limited data on the needs and experiences of Black adolescents assigned female at birth (AFAB) regarding sexual and reproductive health (SRH) services. Our research sought to fill this gap through a qualitative study that aimed to 1) understand perspectives and experiences of Black AFAB adolescents in North Carolina (NC) receiving SRH-counseling in primary care, and 2) elicit Black AFAB adolescent preferences for SRH-related communication with healthcare providers to inform future innovation in SRH care delivery. 23 Black AFAB adolescents 13 to 17 years old who received primary care across NC to completed virtual, semi-structured interviews. A codebook was inductively and deductively developed by the research team and applied to transcripts using Dedoose software. This project received IRB approval from the University of North Carolina-Chapel Hill and required parental consent prior to adolescent assent and participation. While most Black AFAB adolescents had positive perceptions of health providers regarding trust, confidentiality, and respect, there were significant gaps in the provision of comprehensive SRH care. Suggested areas for improvement identified by adolescents included revamping the provider role within the patient-parent relationship, a preference for provider initiation of SRH conversations, comprehensive SRH education by health provider given heterogeneous quality of non-clinical sources of SRH information, and improvement in physical clinical spaces (i.e., doctors’ offices) to improve comfort in discussing SRH topics. This work centers voices of a sample of Black AFAB adolescents receiving healthcare in NC, creating a framework for the development of reproductive counseling interventions and provider education supporting reproductive autonomy.
Click here for large version
Self-collection of microbiome samples and leg circumference measurements among endometrial cancer survivors: A pilot study
Jordyn Brown, MPH
Contact: jordyn.brown@unc.edu
 Jordyn Brown is a first-year PhD Student in the Department of Epidemiology at the UNC Gillings School of Global Public Health. She is a graduate research assistant under the direction of her faculty advisor, Dr. Hazel Nichols, focusing on endometrial cancer disparities within the Carolina Endometrial Cancer Study and Cancer Survivorship Cohort. Originally from Columbus, Ohio, she completed her BS in Public Health with a specialization in sociology and her MPH in Epidemiology from The Ohio State University. Prior to seeking a PhD, Jordyn contributed to qualitative and quantitative analyses to improve stark maternal and child health disparities and support initiatives to mitigate the Black-White infant mortality crisis at the Kirwan Institute for the Study of Race and Ethnicity and The Ohio State University Wexner Medical Center. Strategies to reduce disparities across the pregnancy continuum inspired her to implement similar strategies across the cancer continuum and ultimately contribute to working knowledge of the burden of social and healthcare disparities among endometrial cancer survivors. Jordyn’s research aims to identify and address contributors to endometrial cancer disparities with a special interest in the role of geographic location as it relates to the socio-physical environment, physical activity, and medical comorbidities on health-related quality of life.
Jordyn Brown is a first-year PhD Student in the Department of Epidemiology at the UNC Gillings School of Global Public Health. She is a graduate research assistant under the direction of her faculty advisor, Dr. Hazel Nichols, focusing on endometrial cancer disparities within the Carolina Endometrial Cancer Study and Cancer Survivorship Cohort. Originally from Columbus, Ohio, she completed her BS in Public Health with a specialization in sociology and her MPH in Epidemiology from The Ohio State University. Prior to seeking a PhD, Jordyn contributed to qualitative and quantitative analyses to improve stark maternal and child health disparities and support initiatives to mitigate the Black-White infant mortality crisis at the Kirwan Institute for the Study of Race and Ethnicity and The Ohio State University Wexner Medical Center. Strategies to reduce disparities across the pregnancy continuum inspired her to implement similar strategies across the cancer continuum and ultimately contribute to working knowledge of the burden of social and healthcare disparities among endometrial cancer survivors. Jordyn’s research aims to identify and address contributors to endometrial cancer disparities with a special interest in the role of geographic location as it relates to the socio-physical environment, physical activity, and medical comorbidities on health-related quality of life.
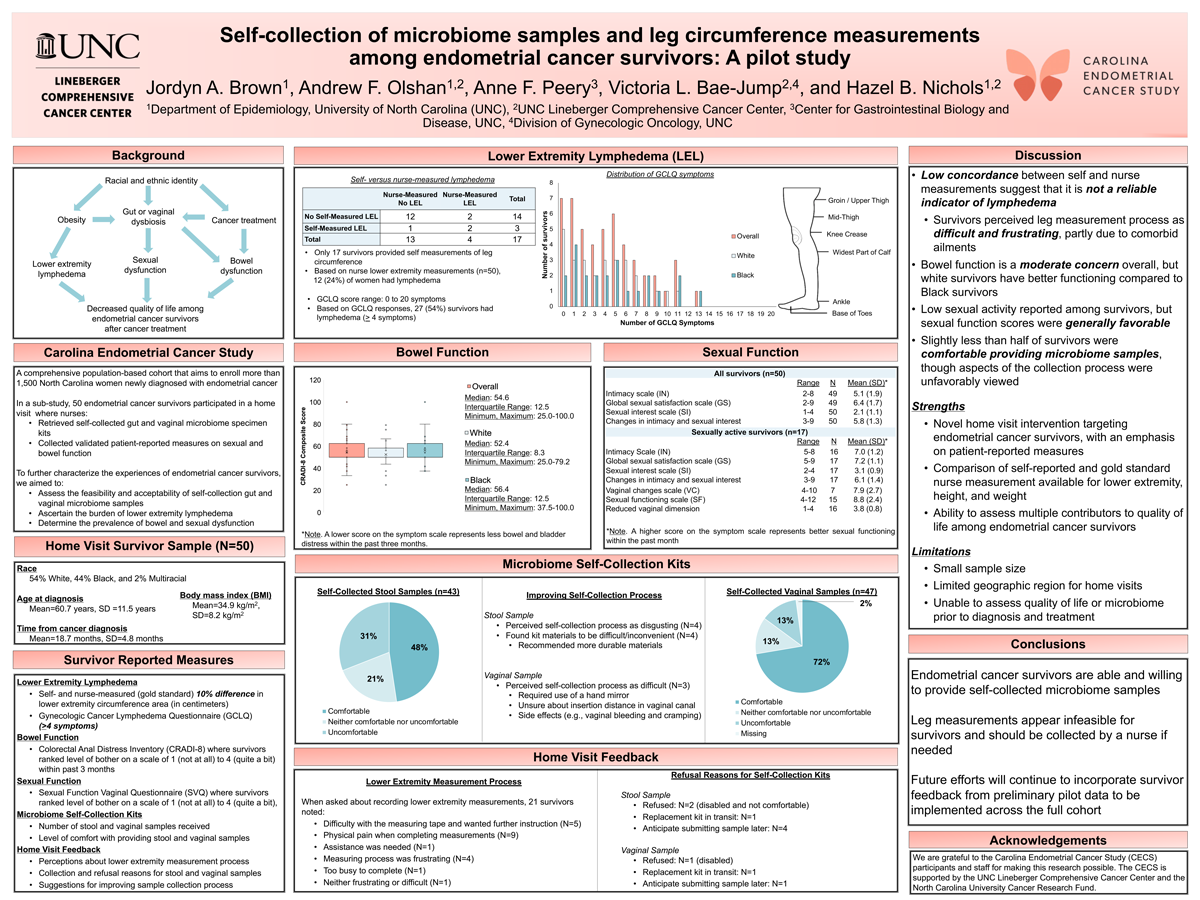
Self-collection of microbiome samples and leg circumference measurements among endometrial cancer survivors: A pilot study
Jordyn A. Brown1, Andrew F. Olshan1,2, Anne F. Peery3, Victoria L. Bae-Jump2,4, Hazel B. Nichols1,2
1. Department of Epidemiology, Gillings School of Global Public Health, University of North Carolina; 2. UNC Lineberger Comprehensive Cancer Center; 3. Center for Gastrointestinal Biology and Disease, University of North Carolina; 4. Division of Gynecologic Oncology, University of North Carolina
Endometrial cancer survivors experience declines in quality of life following cancer treatment. We conducted a pilot study to assess feasibility of self-collection of gut and vaginal microbiome samples, self-measurement of leg circumference, and to collect preliminary data on lymphedema, bowel and sexual function. Endometrial cancer survivors were mailed gut and vaginal microbiome self-collection kits; instructions for leg measurements; and bowel and sexual function and lower extremity lymphedema (LEL) surveys prior to a nurse home visit. Measures of feasibility included completion of microbiome kits and leg measurements. LEL had a 10% threshold difference between right and left leg measurements or > 4 symptoms on the Gynecologic Cancer Lymphedema Questionnaire (GCLQ). The Colorectal Anal Distress Inventory assessed bowel function [CRADI-8: 0 (no symptoms) to 100 (maximum symptom severity)]. Lower scores on the Sexual Function Vaginal Questionnaire (SVQ) indicated worse function. Among 50 participants, 44% were Black. Mean age was 60.8 years and mean BMI was 34.9 kg/m2. Most women submitted gut (N=43) or vaginal (N=47) samples; fewer (N=17) submitted leg measurements. Participants were comfortable with microbiome sample collection but not self-leg measurements. Among 17 women with nurse and self leg measurements, 24% met criteria for LEL. Overall, 24% met criteria for LEL by nurse measurement and 54% met criteria by GCLQ. CRADI-8 scores (mean=54.6) indicated moderate bowel distress and survivors had favorable SVQ intimacy and satisfaction scores. Self-collection of microbiome samples, but not lower leg measurements, was feasible. Prevalence of LEL was high, bowel distress moderate, and intimacy scores were often favorable.
Click here for large version
Effects of the Menstrual Cycle and Hormonal Contraception on Protein Turnover
Hannah Cabré, MS, RDN
Contact: saylor16@live.unc.edu
 Hannah Cabré, is a registered dietitian and a doctoral candidate in the Human Movement Science Curriculum, which is part of the UNC Chapel Hill School of Medicine. She attended the University of Georgia for her undergraduate degree in Dietetics and completed her masters degree in sports nutrition and exercise physiology, as well as her dietetic internship, at Florida State University. Currently, Hannah has successfully completed her dissertation data collection and analyses and is set to defend her dissertation on March 23rd. Her research focuses on the effects of hormonal contraception and the menstrual cycle on exercise outcomes. She received research funding from the National Strength and Conditioning Foundation and the University of North Carolina Graduate School to support her dissertation research. To date, Mrs. Cabré has 30 peer-reviewed manuscripts and 12 first author peer-reviewed research abstracts and poster presentations at regional and national conferences. She will begin a post-doctoral fellowship at Pennington Biomedical Research Center after graduation.
Hannah Cabré, is a registered dietitian and a doctoral candidate in the Human Movement Science Curriculum, which is part of the UNC Chapel Hill School of Medicine. She attended the University of Georgia for her undergraduate degree in Dietetics and completed her masters degree in sports nutrition and exercise physiology, as well as her dietetic internship, at Florida State University. Currently, Hannah has successfully completed her dissertation data collection and analyses and is set to defend her dissertation on March 23rd. Her research focuses on the effects of hormonal contraception and the menstrual cycle on exercise outcomes. She received research funding from the National Strength and Conditioning Foundation and the University of North Carolina Graduate School to support her dissertation research. To date, Mrs. Cabré has 30 peer-reviewed manuscripts and 12 first author peer-reviewed research abstracts and poster presentations at regional and national conferences. She will begin a post-doctoral fellowship at Pennington Biomedical Research Center after graduation.
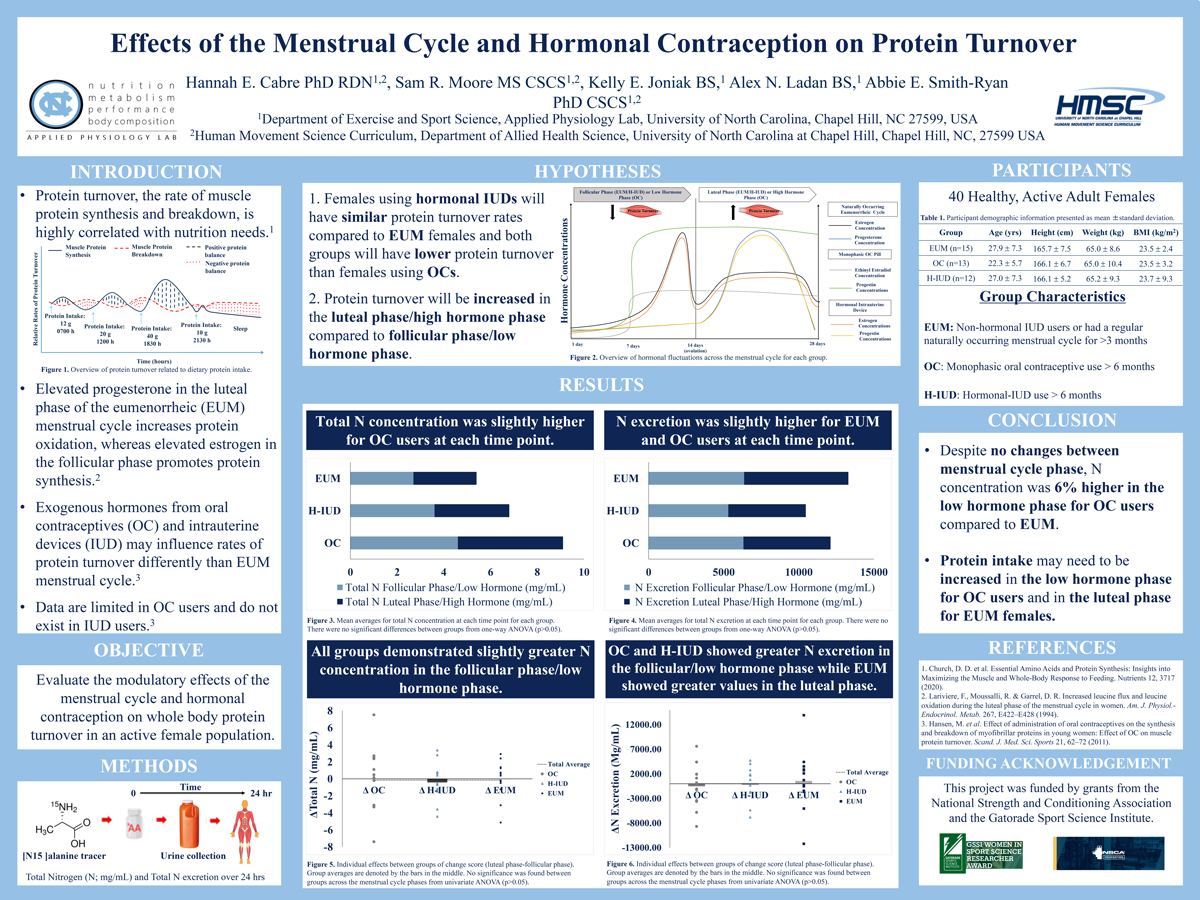
Effects of the Menstrual Cycle and Hormonal Contraception on Protein Turnover
Hannah E. Cabre1,2, Sam R. Moore1,2, Kelly E. Joniak1, Alex N. Ladan1, Abbie E. Smith-Ryan1,2
1. Applied Physiology Laboratory, Department of Exercise Sport and Science, University of North Carolina, Chapel Hill, NC; 2. Human Movement Science Curriculum, University of North Carolina, Chapel Hill, NC
This study aimed to evaluate the modulatory effects of the menstrual cycle (MC) and hormonal contraception on whole body protein turnover, an important metabolic health measure. Forty healthy, recreationally-active females (mean±standard deviation; Age: 25.8±7.1 yrs, BMI: 23.6±2.8 kg/m2) who were using a non-hormonal intrauterine device (IUD) or had a regular naturally occurring MC (≥3 months) (EUM; n=15), monophasic oral contraceptive users (OC; n=13), or had a hormonal-IUD (H-IUD; n=12) were evaluated. Females using hormonal contraceptives were required to utilize the same form for ≥6 months. Protein turnover measures were evaluated using [N15 ]alanine tracer for total nitrogen (N; mg/mL) concentration and total N excretion over 24 hrs. Participants were randomly assigned to begin in the follicular phase/placebo pill (FP) or in the luteal phase/active pill (LP) and were tested once in each phase. Univariate ANOVAs of change scores (LP-FP) showed no significant differences in total N or total N excretion (p>0.05) across the MC between groups. All groups demonstrated greater total N in the FP (OC: Δ-0.02±3.7 mg/mL; H-IUD: Δ-0.4±2.3 mg/mL; EUM: Δ-0.02±2.0 mg/mL). The OC (Δ-513.9±1272.8 mg/mL) and H-IUD (Δ-144.1±1324.8 mg/mL) groups showed greater N excretion in the FP, while EUM demonstrated greater excretion in the LP (Δ579.5±1184.9 mg/mL). Despite no changes between MC phase, N excretion was 6% higher in the FP for OC compared to EUM. Protein intake may need to be increased in the FP for OC users and in the LP for EUM females.
Click here for large version
Estrogen fluctuations predict depressive symptomatology in adolescent females at elevated risk for suicide
Lindsey Cunnane
Contact: lindsey_cunnane@med.unc.edu
Lindsey Cunnane is from Philadelphia, Pennsylvania. She attended East Carolina University with a Bachelors in Psychology and a Science minor and graduated Summa Cum Laude in 2021. Lindsey’s position at UNC involves overseeing and coordinating an NIH-funded longitudinal, observational study (R01-MH12246), on the predictors of suicidality, including intent, attempts, and non-suicidal self-injurious (NSSI) behavior in 125 adolescents assigned female at birth. She is interested in studying women’s reproductive health with a concentration on how traumatic reproductive experiences may exacerbate mental health conditions such as depression, OCD, and PTSD. She hopes to pursue a PhD in Clinical Psychology within the next few years.
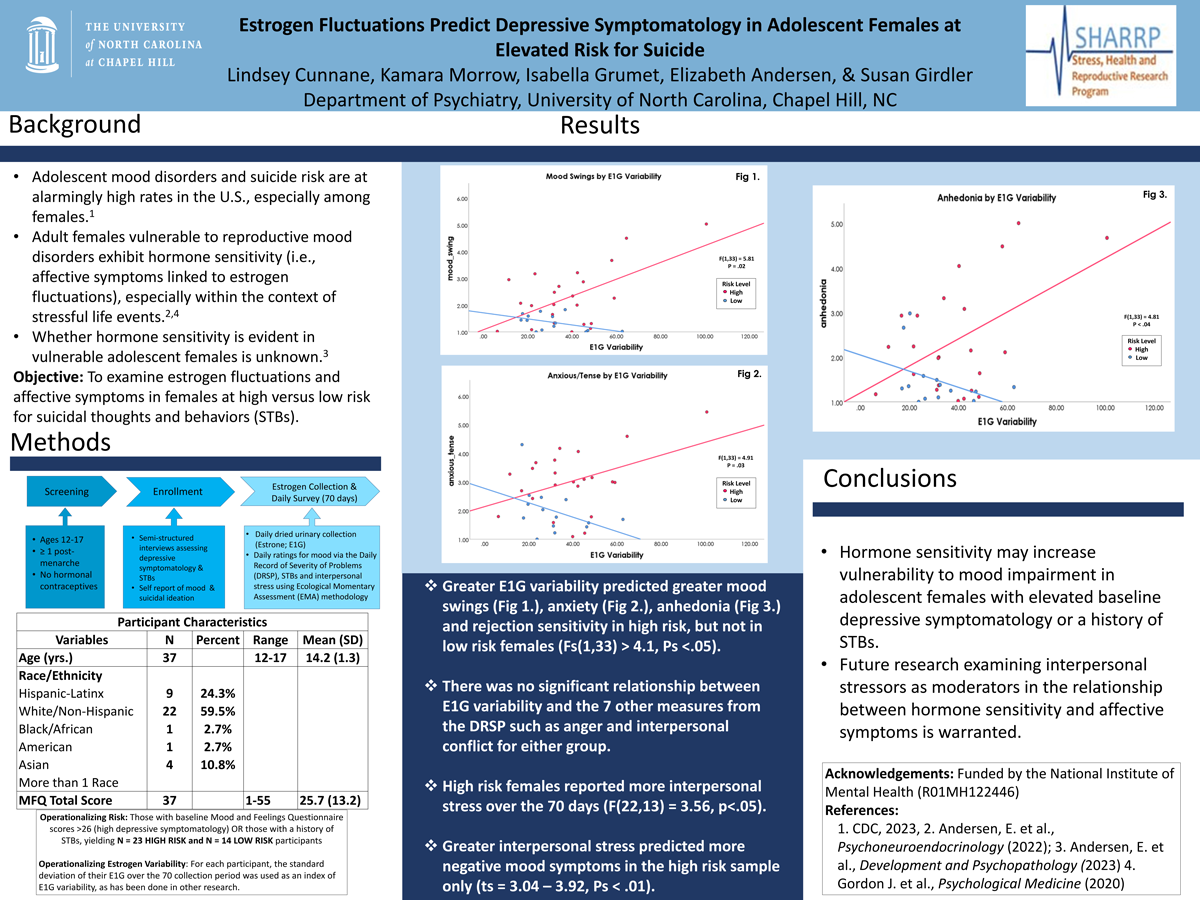
Estrogen fluctuations predict depressive symptomatology in adolescent females at elevated risk for suicide
Lindsey Cunnane1, Kamara Morrow1, Isabella Grumet1, Elizabeth Andersen1, Susan Girdler1
1. University of North Carolina at Chapel Hill
Adult females vulnerable to reproductive mood disorders exhibit hormone sensitivity, with affective symptoms linked to fluctuations in estrogen. Whether hormone sensitivity is evident in vulnerable adolescent females is unknown. Depression and suicidal thoughts and behaviors (STBs) in adolescents have increased substantially in the context of the COVID-19 pandemic. Examining hormone sensitivity in depression risk in adolescent females addresses a critical public health gap. Females aged 12 – 17 who were post-menarche were recruited as either high risk for depression and STBs based on elevated depressive symptomatology or a history of STBs using structured interviews (N=23), or as low risk based on low depressive symptoms and no STB history (N = 14). Over 70-days, participants provided daily urinary estrone (E1G; a metabolite of estradiol) and completed daily ratings for mood and interpersonal stressors using ecological momentary assessment methods. The relationship between E1G fluctuations and mood was examined using general linear modeling. Greater E1G variability predicted greater rejection sensitivity, mood swings and anxiety in high risk, but not low risk females (Fs(1,33) > 4.1, Ps <.05). High risk females reported more interpersonal stress over the 70 days (F(22,13) = 3.56, p<.05), which predicted more negative mood symptoms in the high risk sample only (ts = 3.04 – 3.92, Ps < .01). Hormone sensitivity may increase vulnerability to mood impairment in adolescent females with elevated baseline depressive symptomatology or a history of STBs. Future research examining interpersonal stressors as moderators in the relationship between hormone sensitivity and affective symptoms is warranted.
Click here for large version
Improving Cesarean Hemorrhage Through the Use of a Protocolized Checklist; a Quality Improvement Initiative
Brittany Cureton, MPH
Contact: brittany_cureton@med.unc.edu
 Brittany Cureton is a fourth-year medical student from Charlotte, NC, completing her Master of Public Health at Gillings School of Global Public Health. She has a passion for understanding the complexities of health and dismantling health disparities and inequities seen in marginalized and vulnerable communities and which guides her work in medicine and public health. She aspires to one day serve as a physician who incorporates social determinants of health, health disparities, and inequities into clinical practice to better understand and treat patients from all populations. She hopes to one day be a leader in health equity, someone who, on a national level, creates evidence-based recommendations and strategies for equalizing social determinants of health and improving health outcomes for all.
Brittany Cureton is a fourth-year medical student from Charlotte, NC, completing her Master of Public Health at Gillings School of Global Public Health. She has a passion for understanding the complexities of health and dismantling health disparities and inequities seen in marginalized and vulnerable communities and which guides her work in medicine and public health. She aspires to one day serve as a physician who incorporates social determinants of health, health disparities, and inequities into clinical practice to better understand and treat patients from all populations. She hopes to one day be a leader in health equity, someone who, on a national level, creates evidence-based recommendations and strategies for equalizing social determinants of health and improving health outcomes for all.
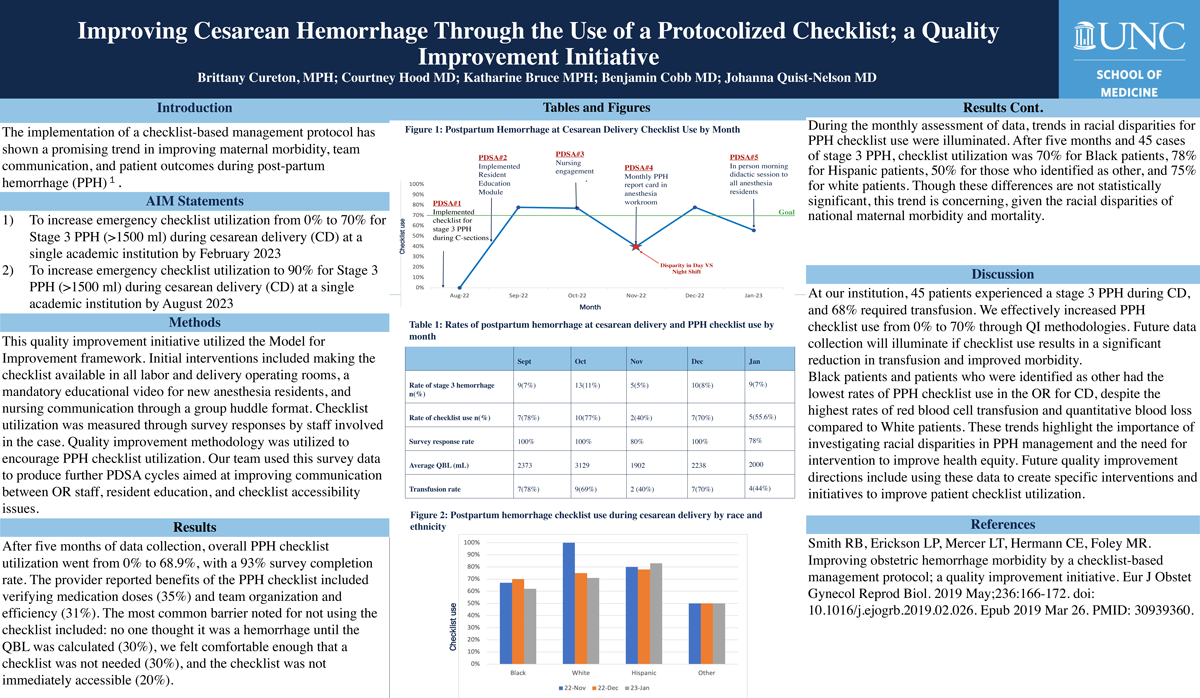
Improving Cesarean Hemorrhage Through the Use of a Protocolized Checklist; a Quality Improvement Initiative
Brittany Cureton, BA, MPH; Courtney Hood, MD; Katharine Bruce, MPH; Benjamin Cobb, MD; Johanna Quist-Nelson, MD
Implementing a checklist-based management protocol has shown a promising trend in improving maternal morbidity, team communication, and patient outcomes during post-partum hemorrhage (PPH).1 The aim of this quality improvement (QI) study was to increase emergency checklist utilization from 0% to 90% for Stage 3 PPH (>1500 ml) during cesarean delivery (CD) at a single academic institution. This quality improvement study measured PPH checklist utilization for all Stage 3 PPH in the operating room (OR) starting in September 2022. Checklist utilization was measured through survey responses by staff involved in the case. Quality improvement methodology was utilized to encourage PPH checklist utilization. Our team used this survey data to produce further PDSA cycles to improve communication between OR staff, resident education, and checklist accessibility issues. After four months of data collection and 37 cases, overall PPH checklist utilization went from 0% to 70% with a 95% survey completion rate. The reported benefits of the PPH checklist included verifying reported benefits of the PPH checklist included: verification of medication doses (35%) and team organization and efficiency (31%). The most common barrier noted for not using the checklist included: no one thought it was a hemorrhage until the QBL was calculated (30%), we felt comfortable enough that a checklist was not needed (30%), and the checklist was not immediately accessible (20%). At our institution, 37 patients experienced stage 3 PPH during CD, and 68% of those patients required transfusion. We effectively increased PPH checklist use from 0% to 70%. Future data collection will illuminate if checklist use results in a significant reduction in transfusion and improved morbidity.
- Smith RB, Erickson LP, Mercer LT, Hermann CE, Foley MR. Improving obstetric hemorrhage morbidity by a checklist-based management protocol; a quality improvement initiative. Eur J Obstet Gynecol Reprod Biol. 2019 May;236:166-172. doi: 10.1016/j.ejogrb.2019.02.026. Epub 2019 Mar 26. PMID: 30939360.
Click here for large version
Feasibility Testing of a Virtually Delivered Educational Intervention in Women with Acute Coronary Syndrome
Leslie Davis, PhD, RN
Contact: LLDavis@email.unc.edu
 Dr. Leslie Davis, PhD, APRN, FAAN, FAANP, FACC, FAHA, FPCNA is an Associate Professor at UNC Chapel Hill. She maintains a part-time NP practice with the Division of Cardiology at the UNC. A cardiovascular expert, Dr. Davis is a fellow in the American Academy of Nurses, the American College of Cardiology (ACC), the American Association of NPs, the American Heart Association, and the Preventive Cardiovascular Nurses Association. Dr. Davis has served as editor for Cardiovascular Nursing Secrets, as guest editor for an upcoming cardiovascular issue of Nursing Clinics of North America and two past issues in the Journal for NPs, as author for 45+ papers in peer-reviewed journals, three ACC Expert Consensus Decision Pathways, and 15 book chapters. In 2021 she received the Distinguished Associate Award from the ACC and serves as Associate Editor for the JNP. Dr. Davis’ research addresses self-care and symptom management in women with cardiovascular conditions. Dr. Davis has developed and tested an individualized self-care intervention aimed at improving symptom recognition and care-seeking behavior in women who have experienced an acute coronary syndrome (ACS) event. Her intervention is informed by qualitative studies with women with ACS. The intervention is virtually delivered within a month of an ACS event when survivors are at highest risk for readmission for recurrent symptoms and less likely to have started cardiac rehabilitation. Improving symptom recognition and timely communication of recurrent symptoms is considered the single most important factor for improving ACS patient outcomes, especially for those from traditionally underrepresented communities.
Dr. Leslie Davis, PhD, APRN, FAAN, FAANP, FACC, FAHA, FPCNA is an Associate Professor at UNC Chapel Hill. She maintains a part-time NP practice with the Division of Cardiology at the UNC. A cardiovascular expert, Dr. Davis is a fellow in the American Academy of Nurses, the American College of Cardiology (ACC), the American Association of NPs, the American Heart Association, and the Preventive Cardiovascular Nurses Association. Dr. Davis has served as editor for Cardiovascular Nursing Secrets, as guest editor for an upcoming cardiovascular issue of Nursing Clinics of North America and two past issues in the Journal for NPs, as author for 45+ papers in peer-reviewed journals, three ACC Expert Consensus Decision Pathways, and 15 book chapters. In 2021 she received the Distinguished Associate Award from the ACC and serves as Associate Editor for the JNP. Dr. Davis’ research addresses self-care and symptom management in women with cardiovascular conditions. Dr. Davis has developed and tested an individualized self-care intervention aimed at improving symptom recognition and care-seeking behavior in women who have experienced an acute coronary syndrome (ACS) event. Her intervention is informed by qualitative studies with women with ACS. The intervention is virtually delivered within a month of an ACS event when survivors are at highest risk for readmission for recurrent symptoms and less likely to have started cardiac rehabilitation. Improving symptom recognition and timely communication of recurrent symptoms is considered the single most important factor for improving ACS patient outcomes, especially for those from traditionally underrepresented communities.
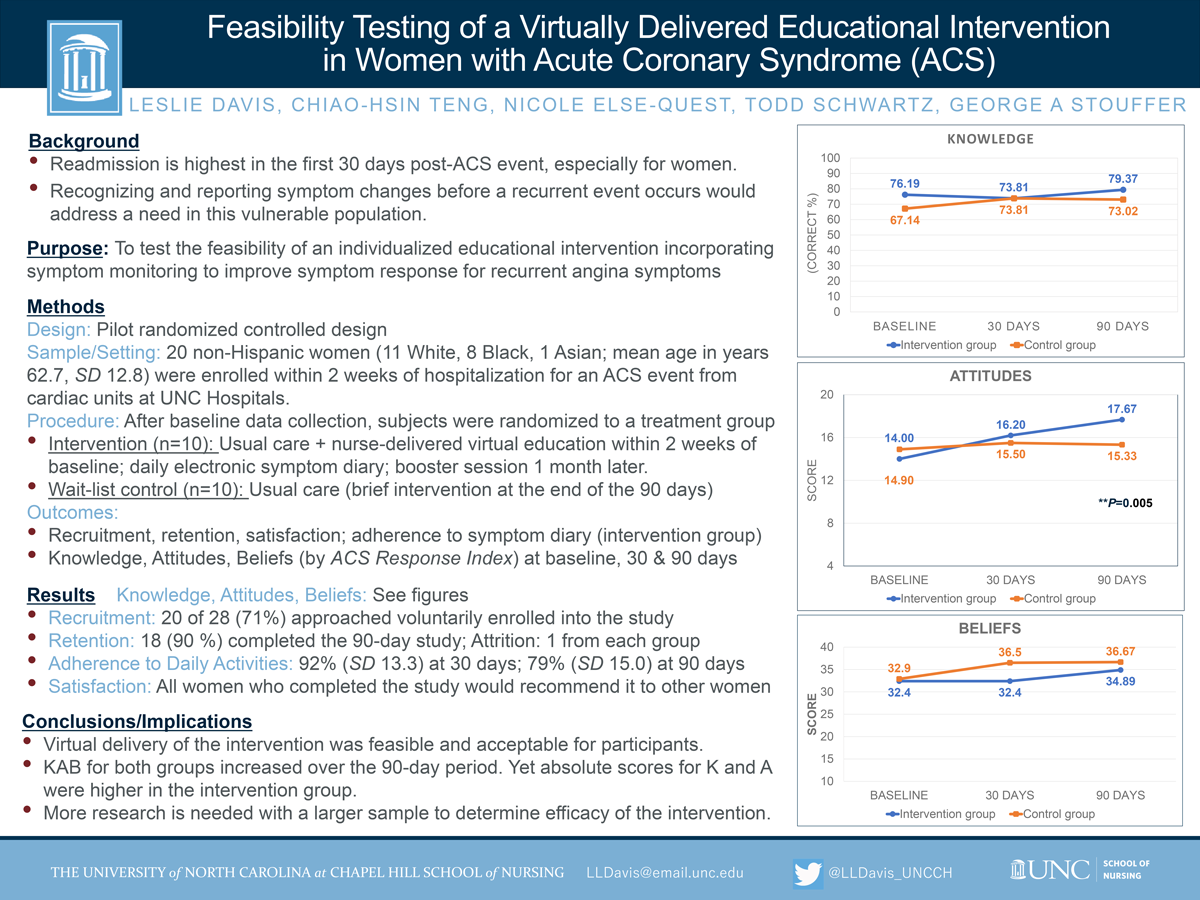
Feasibility Testing of a Virtually Delivered Educational Intervention in Women with Acute Coronary Syndrome
Leslie L Davis1, Chiao-Hsin Teng2, Nicole Else-Quest3, Todd A Schwartz4, George (Rick) Stouffer5
1. Associate Professor; UNC Chapel Hill, School of Nursing; 2. PhD student, UNC Chapel Hill, School of Nursing; 3. Associate Professor, UNC Chapel Hill, Women’s and Gender Studies; 4. Professor, UNC Chapel Hill, School of Nursing/School of Public Health; 5. Professor, UNC Chapel Hill, School of Medicine, Dept of Medicine, Division of Cardiology
Background: Readmission is highest in the month following an acute coronary syndrome (ACS) event. Recognizing recurrent symptoms addresses a clinical need in this vulnerable population. We developed an educational intervention (INT) incorporating symptom monitoring to improve response.
Methods: A pilot RCT design was used to test feasibility of our INT. We enrolled women with a recent ACS event from UNC hospitals. Following baseline data collection, subjects were randomized to INT or control (C). Within 2 weeks of baseline, the INT group received virtually-delivered education followed by a booster session 1 month later. The C group received usual care. Knowledge, attitudes, and beliefs (KAB) were collected at baseline, 30, and 90 days for both groups.
Results: Of the 20 women (11 White, 8 Black, 1 Asian) enrolled, 18 completed the study. Mean KAB scores from baseline-to-30 days for the INT group changed by -2.4%, +2.2, and 0 versus +7.1%, +0.9, +2.6 for the C group. Mean KAB scores from baseline-to-90 days increased by +3.2%, +3.4, and +3.1 for the INT group versus +5.8%, +0.6, +3.4 in the C group. Mean adherence to monitoring activities for the INT group was 92% (SD 13.3) and 79% (SD 15.0) at 30 and 90 days.
Conclusion: Virtual delivery of the INT was feasible and acceptable for participants. KAB for both groups increased over the 90 day period; although absolute scores for K and A were higher for the INT group. Further research is needed with a larger sample to determine the efficacy of the INT.
Click here for large version
Metal mixtures in private well water are associated with preterm birth in North Carolina
Lauren Eaves, PhD, IBCLC
Contact:laeaves@live.unc.edu
 I am currently a research scientist with the Institute of Environmental Health Solutions at the Gillings School of Public Health as well as an Adjunct Assistant Professor in the Department of Environmental Sciences and Engineering. My research focuses on environmental drivers of health outcomes, particularly women’s and perinatal health, and children’s developmental trajectories. My commitment to investigating women’s and perinatal health stems from clinical experience as a doula and an International Board Certified Lactation Consultant (IBCLC). In these roles I provide companionate, patient-centered bedside/in-clinic care to pregnant and postpartum families. Clinical experiences with families navigating illness drives my motivation to investigate environmental and structural drivers of the diseases that I witness patients experiencing.
I am currently a research scientist with the Institute of Environmental Health Solutions at the Gillings School of Public Health as well as an Adjunct Assistant Professor in the Department of Environmental Sciences and Engineering. My research focuses on environmental drivers of health outcomes, particularly women’s and perinatal health, and children’s developmental trajectories. My commitment to investigating women’s and perinatal health stems from clinical experience as a doula and an International Board Certified Lactation Consultant (IBCLC). In these roles I provide companionate, patient-centered bedside/in-clinic care to pregnant and postpartum families. Clinical experiences with families navigating illness drives my motivation to investigate environmental and structural drivers of the diseases that I witness patients experiencing.
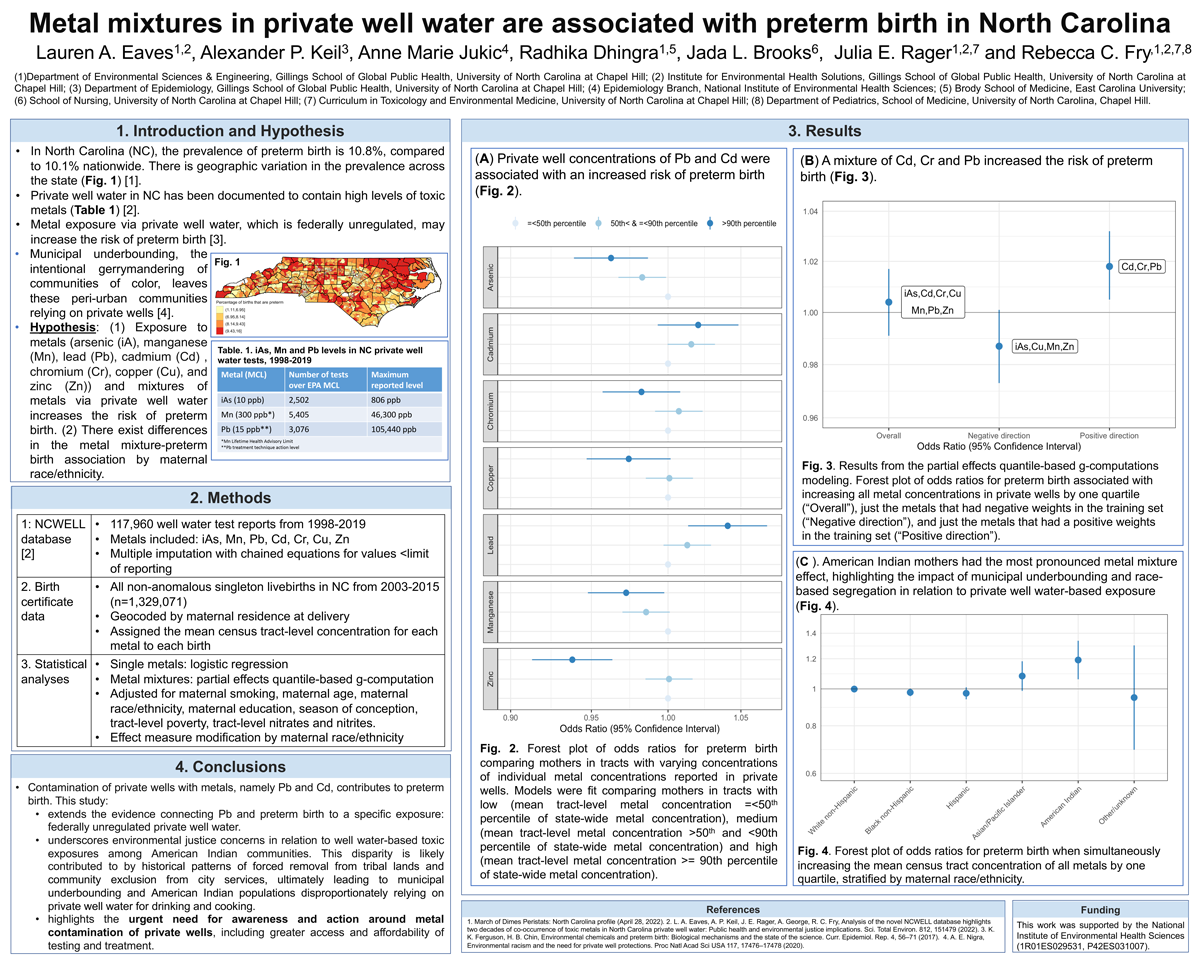
Metal mixtures in private well water are associated with preterm birth in North Carolina
Lauren A. Eaves, Alexander P. Keil, Anne Marie Jukic, Radhika Dhingra, Jada L Brooks, Julia E. Rager and Rebecca C. Fry
Prenatal exposure to metals in private well water may increase the risk of preterm birth. In this study, we estimated associations between arsenic, manganese, lead, cadmium, chromium, copper, and zinc concentrations in private well water and preterm birth incidence in North Carolina (NC). Birth certificates from 2003-15 (n = 1,329,071) were assigned exposure using the mean concentration and the percentage of tests above the maximum contaminant level (MCL) in each tract from the NC-WELL database (117,960 well water tests from 1998-2019). We evaluated associations between individual metals and preterm birth using adjusted logistic regression models. Metals mixtures were assessed using quantile-based g-computation to estimate joint associations. Compared with mothers in other tracts, mothers residing in census tracts where over 25% of tests exceeded the maximum contaminant level (MCL, 15ppb) for lead had 1.10 times the odds of preterm birth (95%CI 1.02,1.18). Likewise, for mothers in census tracts where >25% of tests exceeded the MCL for cadmium (5ppb), the OR for preterm birth was 1.11 (95% CI 1.00,1.23). Zinc and copper concentrations were associated with reduced odds of preterm birth. A mixture of lead, cadmium, and chromium was associated with a small increased odds for preterm birth. This metal mixture effect was most pronounced among American Indian mothers (OR per quartile increase in all metals: 1.19 (95% CI 1.06,1.34)), highlighting racial health disparities and the need for more awareness and action to protect vulnerable populations from private well metal contamination.
Click here for large version
Standardizing Blood Pressure Measurement: Step One of An Outpatient Safety Bundle for Severe Pregnancy-Related Hypertension
Elizabeth Finnessy, BSN, RN
Contact: finnessy@live.unc.edu
 Elizabeth “Liz” Finnessy, BSN, RN, is a doctoral student and research assistant in the School of Nursing at The University of North Carolina at Chapel Hill. She holds a Bachelor of Science in Nursing with Honors from the University of North Carolina at Chapel Hill, as well as a minor in Medical Anthropology. She is a member of the 8th cohort of Hillman Scholars. In 2022 she completed her training in Clinician Leadership in Quality and Safety (CLQS) as well as her Hillman Clinical Fellowship. Finnessy continues to work as a clinical nurse on Labor and Delivery at UNC-Medical Center while engaging in various quality improvement projects pertaining to pre-eclampsia. Her research interests include pregnancy, equitable care, and advocacy.
Elizabeth “Liz” Finnessy, BSN, RN, is a doctoral student and research assistant in the School of Nursing at The University of North Carolina at Chapel Hill. She holds a Bachelor of Science in Nursing with Honors from the University of North Carolina at Chapel Hill, as well as a minor in Medical Anthropology. She is a member of the 8th cohort of Hillman Scholars. In 2022 she completed her training in Clinician Leadership in Quality and Safety (CLQS) as well as her Hillman Clinical Fellowship. Finnessy continues to work as a clinical nurse on Labor and Delivery at UNC-Medical Center while engaging in various quality improvement projects pertaining to pre-eclampsia. Her research interests include pregnancy, equitable care, and advocacy.
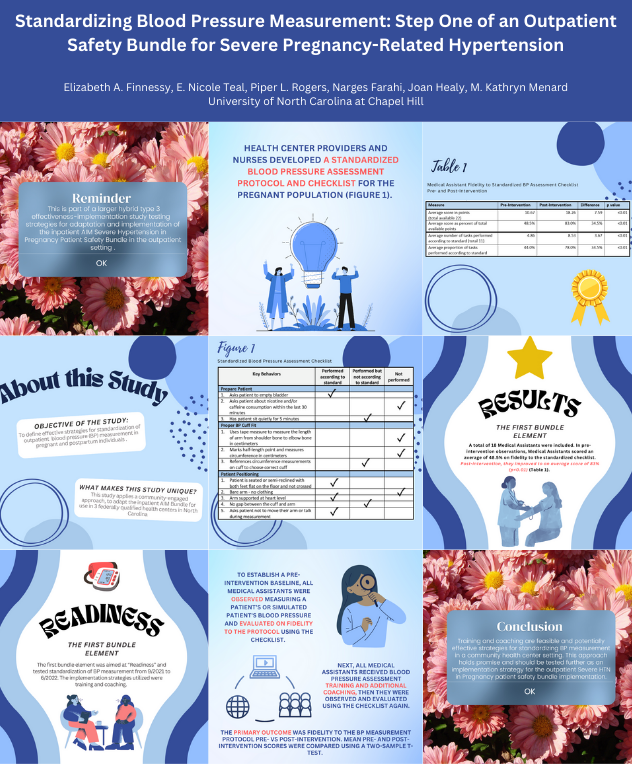
Standardizing Blood Pressure Measurement: Step One of An Outpatient Safety Bundle for Severe Pregnancy-Related Hypertension
Elizabeth A. Finnessy, E. Nicole Teal, Piper L. Rogers, Narges Farahi, Joan Healy, M. Kathryn Menard
University of North Carolina at Chapel Hill
The objective of this study is to define effective strategies for standardization of outpatient blood pressure (BP) measurement in pregnant and postpartum individuals. This is part of a larger hybrid type 3 effectiveness-implementation study testing strategies for adaptation and implementation of the inpatient AIM Severe HTN in Pregnancy Patient Safety Bundle in the outpatient setting. Applying a community-engaged approach, the inpatient AIM Bundle was adapted for use in 3 federally qualified health centers. The first bundle element was aimed at “Readiness” and tested standardization of BP measurement from 9/2021 to 6/2022. The implementation strategies utilized were training and coaching. Health center providers and nurses developed a standardized BP assessment protocol and checklist for the pregnant population (Figure 1). To establish a pre-intervention baseline, all Medical Assistants (MAs) were observed measuring a patient’s BP and evaluated on fidelity to the protocol using the checklist. Next, all MAs received BP assessment training and additional coaching, and were again observed and evaluated using the checklist. The primary outcome was fidelity to the BP measurement protocol pre- vs post-intervention. Mean pre- and post-intervention scores were compared using a two-sample t-test. A total of 18 MAs were included. Pre-intervention, MAs scored an average of 48.5% on fidelity to the standardized checklist. Post-intervention, they improved to an average of 83% (p<0.01). These findings demonstrate that training and coaching are feasible and potentially effective strategies for standardizing BP measurement in pregnant and postpartum patients in a community health center setting.
Click here for large version
Social and Cultural Barriers to Reproductive Health for Adolescent Women in the Altiplano of Bolivia: A Mixed Methods Analysis
Heather Frank, MD
Contact: heather.frank@unchealth.unc.edu
 Dr. Frank is a resident in the combined Internal Medicine and Pediatrics program. She earned a bachelor’s degree in Cellular Neuroscience from Colgate University and spent two years as a Post-Baccalaureate Intramural Research Fellow at the National Institutes of Health. Dr. Frank went on to earn her MD from Duke University School of Medicine where she spent a year working at the Duke Margolis Center for Health Policy. Throughout her medical training she has sought out opportunities to care for Spanish-speaking patients to understand and address their barriers to healthcare. Through the Global Health Scholars’ Program, she will collaborate with local physicians and patient advocates in La Paz and El Alto, Bolivia to study interculturality as a determinant of sexual health for adolescent women of Aymara descent. She will be working with Dr. Cecilia Uribe, the medical director of Child Family Health International, Bolivia, who is an expert in socioeconomic determinants of health and healthcare delivery strategies in low-resource setting.
Dr. Frank is a resident in the combined Internal Medicine and Pediatrics program. She earned a bachelor’s degree in Cellular Neuroscience from Colgate University and spent two years as a Post-Baccalaureate Intramural Research Fellow at the National Institutes of Health. Dr. Frank went on to earn her MD from Duke University School of Medicine where she spent a year working at the Duke Margolis Center for Health Policy. Throughout her medical training she has sought out opportunities to care for Spanish-speaking patients to understand and address their barriers to healthcare. Through the Global Health Scholars’ Program, she will collaborate with local physicians and patient advocates in La Paz and El Alto, Bolivia to study interculturality as a determinant of sexual health for adolescent women of Aymara descent. She will be working with Dr. Cecilia Uribe, the medical director of Child Family Health International, Bolivia, who is an expert in socioeconomic determinants of health and healthcare delivery strategies in low-resource setting.
Social and Cultural Barriers to Reproductive Health for Adolescent Women in the Altiplano of Bolivia: A Mixed Methods Analysis
Heather Frank, MD, Moira Rogers, PhD, Bianca Allison, MD MPH, and Cecilia Uribe MD
Bolivia is undergoing healthcare reform, however the Indigenous population, one of the largest in South America, is being left behind (Francisco N Alvarez, 2016). Young women are particularly affected by the political and social exclusion with high rates of adolescent unintended pregnancy along with disparities in maternal and infant morbidity and mortality compared to non-indigenous populations (Pan American Health Organization, 2008). We designed a convergent parallel mixed methods study of pregnant Indigenous adolescent females (N=9) presenting to hospitals in El Alto and La Paz Bolivia (the Altiplano) to qualitatively explore their barriers to contraception and reproductive health. Using thematic content analysis alongside demographic summary statistics, we identified key barriers and cultural determinants that influenced their current pregnancy including relationships with their partners (e.g., age difference, time in relationship, cohabitation, beliefs about marriage), use and knowledge of contraception (e.g., types of contraception, ability to access contraception, previous use and desire for future use), and their social and cultural beliefs about contraception (e.g., concerns about side effects, partners beliefs, traditional medicine alternatives). These findings can inform interventions focused on culturally competent sexual and reproductive education that integrate traditional medicine concepts, address misconceptions about contraception, and empower young women living within a machismo culture, to promote reproductive autonomy and lower rates of unintended pregnancy for young Indigenous women in the Altiplano of Bolivia.

Click here for large version
Accelerated epigenetic clock aging in peripheral blood is associated with preterm birth (PTB)
Emily Gascoigne
Contact: emilyg11@med.unc.edu
Emily Gascoigne is a recent graduate of the University of North Carolina at Chapel Hill and a current graduate student at NC State. She has been working with the Manuck Research Team since 2019, and she is interested in maternal-fetal health, both locally and globally. Emily also volunteers as a Doula on Labor and Delivery at UNC. She is applying to medical school and aspires to one day work as a Maternal Fetal Medicine physician.
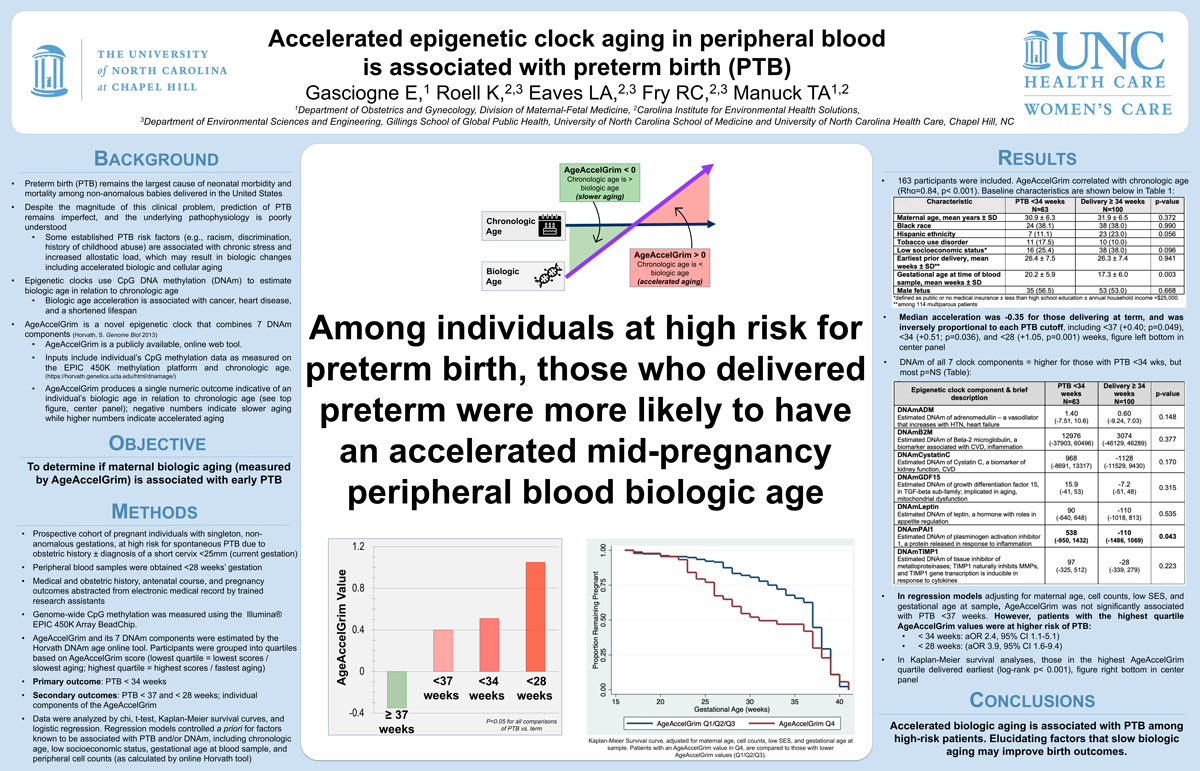
Accelerated epigenetic clock aging in peripheral blood is associated with preterm birth (PTB)
Authors: Gacoigne E, Roell K, Eaves LA, Fry RC, Manuck TA
Objective: Epigenetic clocks estimate biological age using CpG DNA methylation (DNAm). Acceleration is linked to cancer, heart disease, and shorter lifespan. Studies on DNAm age and pregnancy outcomes are limited. We aimed to investigate if maternal aging (via AgeAccelGrim) is linked to early preterm birth.
Methods: Prospective cohort study of high-risk singleton gestations delivering at UNC. Blood samples were taken before 28 weeks and CpG methylation measured using Illumina® EPIC BeadChip. The Horvath DNAm age online tool estimated AgeAccelGrim and its 7 DNAm components. The primary outcome was PTB <34 wks; secondary outcomes were PTB <37 and <28 wks. Data were analyzed by chi2, t-test, logistic regression (controlling for maternal age, cell counts, low SES, and sample GA), and Kaplan-Meier.
Results: The study included 163 eligible patients, with 49%, 38%, and 18% delivering <37, <34, and <28 weeks, respectively. AgeAccelGrim correlated strongly with maternal age (Rho=0.84, p<0.001). Median acceleration was inversely proportional to each PTB cutoff. While DNAm of all 7 clock components was higher for those with PTB <34 weeks, most associations were not significant. Regression models showed higher PTB risk for those with highest AgeAccelGrim quartile values for <34 (aOR 2.4, 95% CI 1.1-5.1) and <28 (aOR 3.9, 95% CI 1.6-9.4) weeks. Kaplan-Meier analysis showed the earliest delivery for those in the highest AgeAccelGrim quartile (log-rank p<0.001). Cohort characteristics and DNAm data are presented in Table 1A and 1B, respectively.
Conclusions: Accelerated biologic aging is associated with PTB among high-risk patients. Elucidating factors that slow biologic aging may improve birth outcomes.
Click here for large version
Loss of CD73 promotes mutant β-catenin oncogenic activity in endometrial cancer
Rebecca Hirsch
Contact: rhirsch@email.unc.edu
I am a 3rd year PhD candidate in the Cell Biology and Physiology curriculum conducting research in Dr. Jessica Bowser’s lab. The Bowser lab studies adenosine signaling in cancer and tissue repair. My research focuses on understanding the molecular and cellular mechanisms of endometrial cancer recurrence. I also investigate individual patient-relevant mutations in the oncoprotein β-catenin for precision medicine efforts. I am a trainee in the Translational Medicine Certificate Program, where I shadow Dr. Siobhan O’Connor, a gynecological pathologist, to gain a better understanding of endometrial cancer and women’s reproductive health. I am a member of the inaugural trainee class of the Women’s Health Multidisciplinary Consortium. I am very passionate about advancing women’s health and reproductive justice.
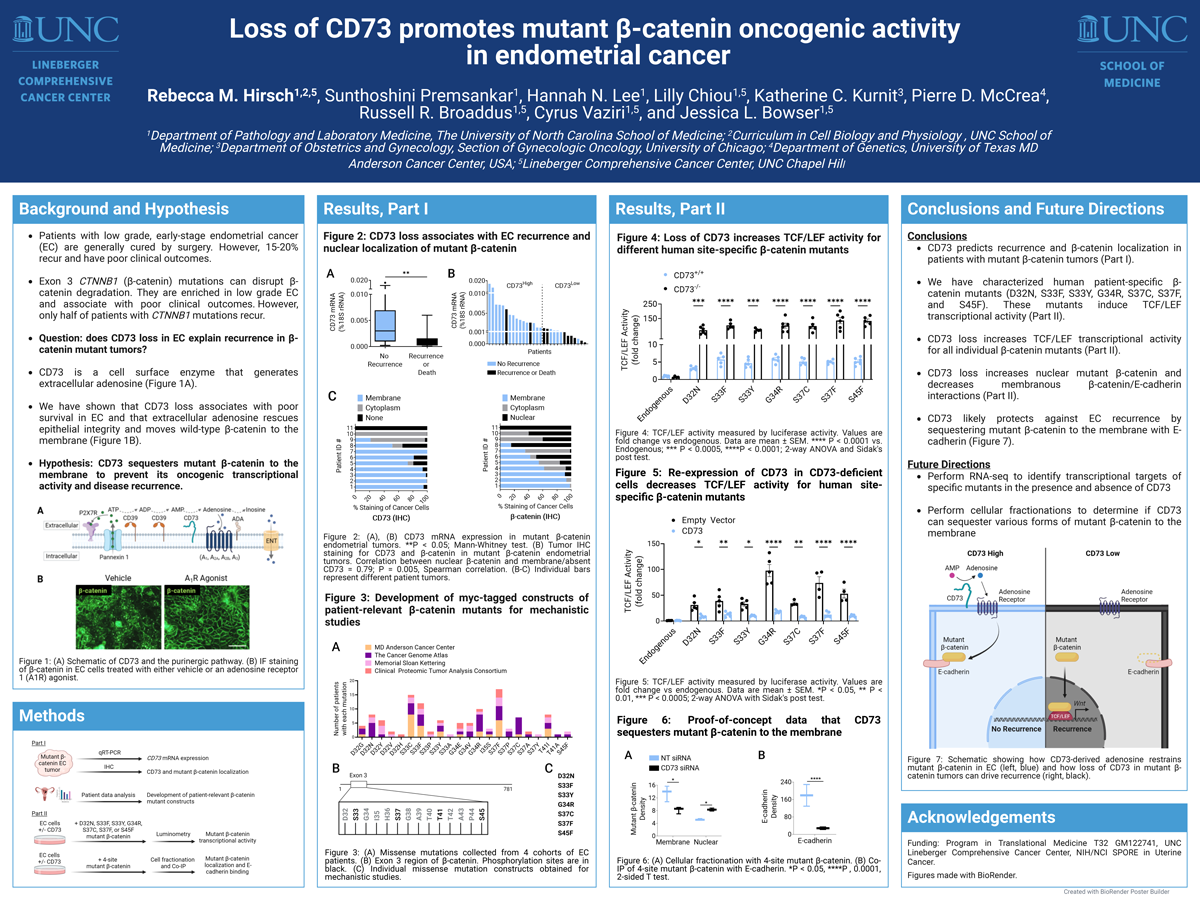
Loss of CD73 promotes mutant β-catenin oncogenic activity in endometrial cancer
Most (80%) endometrial cancers (EC) are diagnosed at an early stage and cured by surgery alone. A gap in knowledge is that 20% of these patients recur, do poorly, and biomarkers to predict recurrence are lacking. While missense mutations in exon 3 of CTNNB1 (encodes β-catenin) identify patients at higher risk, not all patients recur. We recently reported that ecto-5’nucleotidase (CD73) downregulation in EC with exon 3 mutant β-catenin is a strong predictor of recurrence. To understand how CD73 restrains mutant β-catenin, we first performed proof-of-concept experiments using a 4-site exon 3 β-catenin mutant to show CD73 limits mutant β-catenin nuclear translocation and transcriptional activity. In EC, single site mutations in exon 3 are common. We next interrogated patient-relevant β-catenin mutations. We obtained (7) patient-relevant β-catenin mutant constructs for expression in EC cells (HEC-1-A and Ishikawa) with genetic deletion or re-expression of CD73. Reporter assays showed patient-relevant β-catenin mutants at baseline induce TCF/LEF transcriptional activity. With CD73 loss, TCF/LEF transcriptional activity for all mutants increased significantly. With re-expression of CD73, transcriptional activity of the β-catenin mutants decreased. These data suggest that loss of CD73 is a major driver of mutant β-catenin oncogenic activity in EC.
Click here for large version
Characterizing the Neural Substrates of Irritability in Women: A 7T fMRI Study
Megan Hynd
Contact: mhynd@unc.edu
 Megan Hynd is a first-year Clinical Psychology Doctoral Student under the supervision of Dr. Gabriel Dichter. Her research interests are firmly rooted in field of translational medicine; specifically, in determining how aberrant neuronal functioning contributes to depression symptomatology and using that information to develop novel, efficacious treatments. She is currently working on a clinical trial combining PET-MR with hormone treatment to understand reward circuitry in perimenopausal-onset anhedonia and psychosis. Prior to her studies at UNC Chapel Hill, she earned a B.A. in Psychology from the University of Iowa and completed an honors thesis in the Wessel Cognitive Neurology Lab under the supervision of Dr. Jan Wessel. Additionally, she completed a post-bac fellowship at the National Institute of Mental Health, in the Noninvasive Neuromodulation Unit supervised by Dr. Sarah ‘Holly’ Lisanby.
Megan Hynd is a first-year Clinical Psychology Doctoral Student under the supervision of Dr. Gabriel Dichter. Her research interests are firmly rooted in field of translational medicine; specifically, in determining how aberrant neuronal functioning contributes to depression symptomatology and using that information to develop novel, efficacious treatments. She is currently working on a clinical trial combining PET-MR with hormone treatment to understand reward circuitry in perimenopausal-onset anhedonia and psychosis. Prior to her studies at UNC Chapel Hill, she earned a B.A. in Psychology from the University of Iowa and completed an honors thesis in the Wessel Cognitive Neurology Lab under the supervision of Dr. Jan Wessel. Additionally, she completed a post-bac fellowship at the National Institute of Mental Health, in the Noninvasive Neuromodulation Unit supervised by Dr. Sarah ‘Holly’ Lisanby.
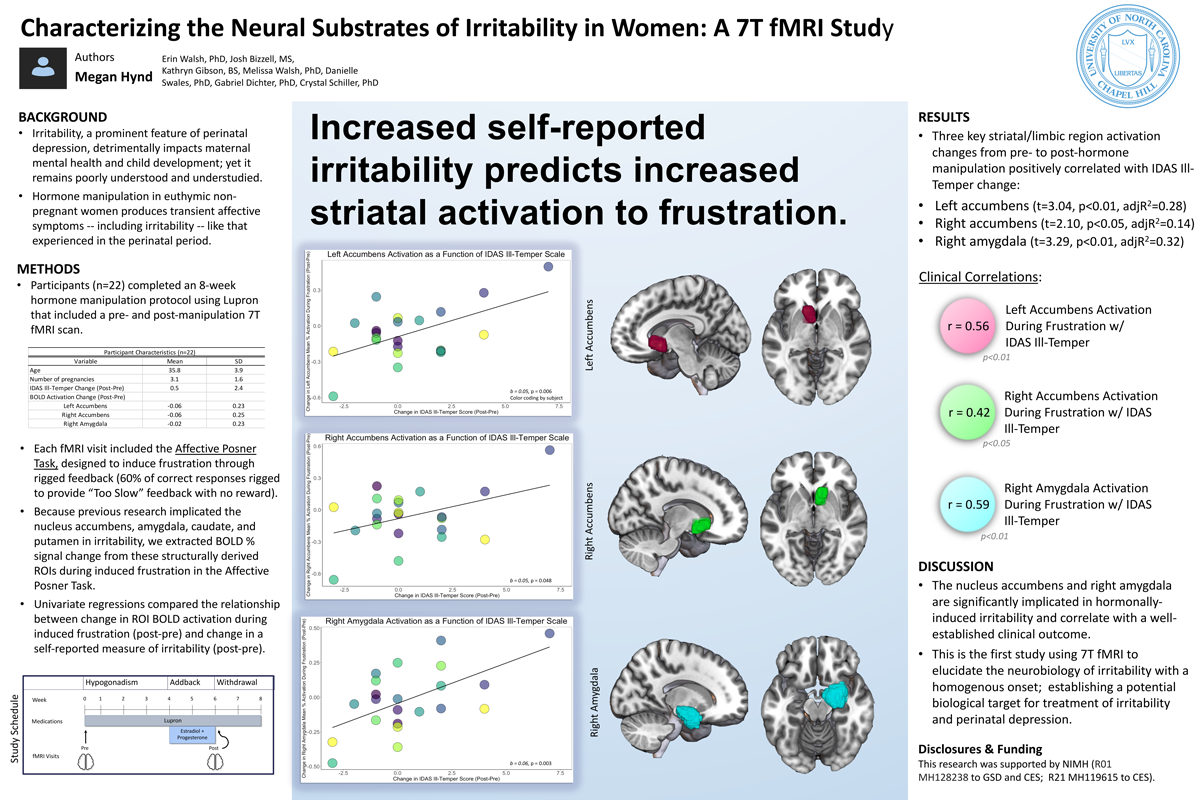
CHARACTERIZING THE NEURAL SUBSTRATES OF IRRITABILITY IN WOMEN: A 7T FMRI STUDY
Authors: Megan Hynd1, Erin Walsh2, Josh Bizzell2, Kathryn Gibson2, Gabriel Dichter1,2, Crystal Schiller2
1. Department of Psychology & Neuroscience, University of North Carolina at Chapel Hill, Chapel Hill, United States; 2. Department of Psychiatry, University of North Carolina at Chapel Hill, Chapel Hill, United States
Background: Irritability is a prominent symptom of perinatal depression (PND). Previous research has validated the experimental manipulation of reproductive hormones to mimic the perinatal period in non-pregnant, euthymic women and to distinguish between hormone sensitive (HS+) and non-hormone sensitive (HS-) women. To determine how female reproductive hormones regulate neural dysfunction that leads to irritability in PND, we conducted an experimental hormone manipulation and functional magnetic resonance imaging (fMRI) study in HS+ females and controls.
Methods: HS+ participants (n=11) and HS- controls (n=12) received a baseline leuprolide acetate injection (Lupron; 3.75mg) to induce stable hypogonadism. Following one month in a hypogonadal state, participants began a two-week hormone “add-back”, using micronized estradiol and progesterone tablets (4mg/day and 400mg/day, respectively). fMRI scans were performed at baseline and at the conclusion of hormone addback on a 7T Siemens MR scanner. Scans included the Affective Posner task to induce frustration. During frustration runs, 60% of correct responses were followed by rigged feedback and 40% of correct responses were followed by positive feedback.
Results: After hormone addback, HS+ (vs. HS-) participants showed increased activation in the pregenual anterior cingulate cortex (k=374) and left putamen (k=143) during rigged feedback relative to positive feedback (TFCE, p<0.05, uncorrected).
Conclusions: Preliminary analyses suggest HS+ participants show increased activation in regions specific to mood regulation and reward processing during frustration after inducing hormone changes similar to the perinatal period.
Click here for large version
The Role of Estradiol in Modifying Circadian Rhythms, Sleep Regularity and Risk for Depression During the Pubertal Transition
Kayla Jensen
Contact: kayla_jensen@med.unc.edu
 Kayla is a study coordinator in the Neuroendocrinology of Reproductive Mood Disorders (NERD) lab, under the mentorship of Drs. Elizabeth Andersen and Susan Girdler. She received her undergraduate degree in biology from the University of North Carolina at Chapel Hill and aims to pursue a career in medicine. She is passionate about improving health outcomes, particularly for underrepresented groups. In her free time, Kayla enjoys reading, painting, and spending time outside.
Kayla is a study coordinator in the Neuroendocrinology of Reproductive Mood Disorders (NERD) lab, under the mentorship of Drs. Elizabeth Andersen and Susan Girdler. She received her undergraduate degree in biology from the University of North Carolina at Chapel Hill and aims to pursue a career in medicine. She is passionate about improving health outcomes, particularly for underrepresented groups. In her free time, Kayla enjoys reading, painting, and spending time outside.
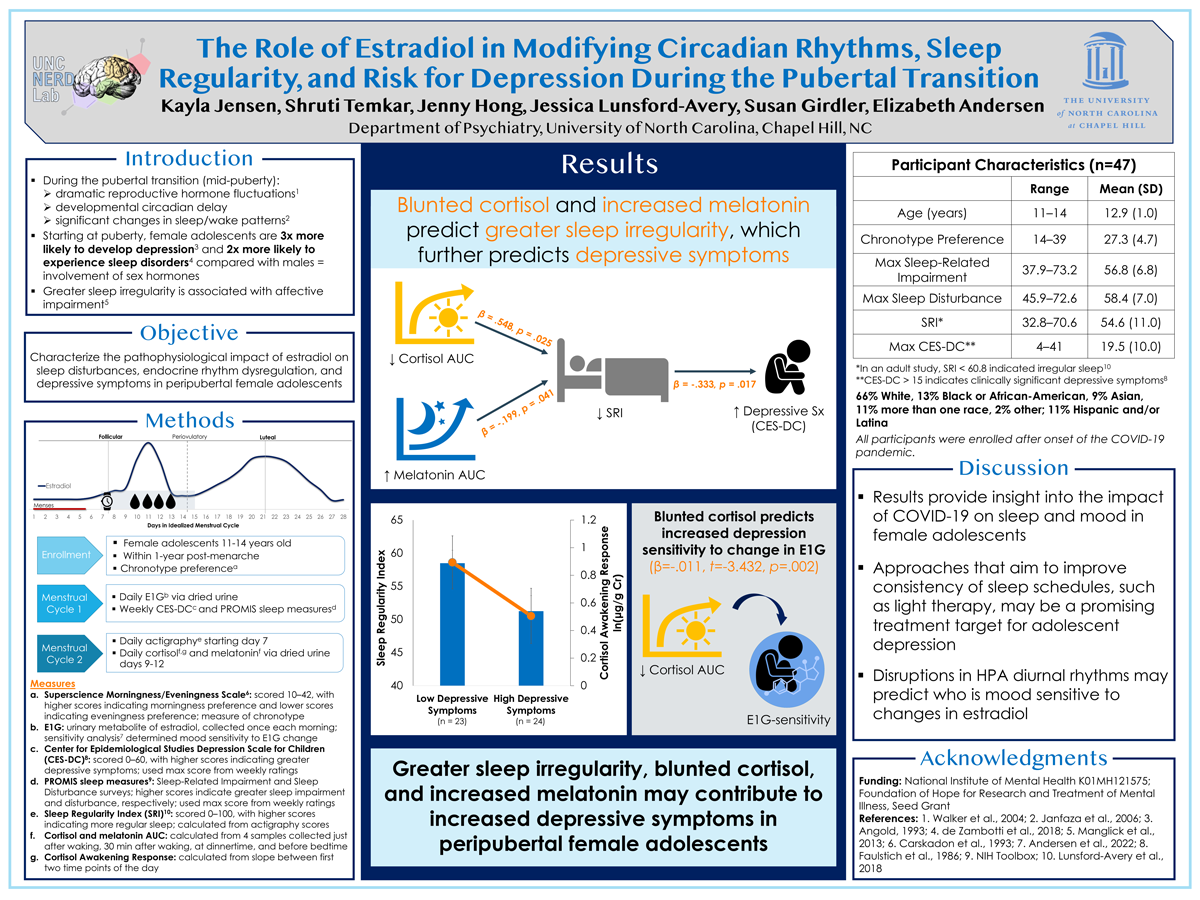
The Role of Estradiol in Modifying Circadian Rhythms, Sleep Regularity and Risk for Depression During the Pubertal Transition
Kayla Jensen1, Shruti Temkar1, Jessica Lunsford-Avery2, Paul Geiger3, Susan Girdler1, Elizabeth Andersen1
1. University of North Carolina at Chapel Hill; 2. Duke University; 3. RTI International
The pubertal transition (PT) is characterized by dramatic reproductive hormone fluctuations, a developmental circadian delay, and significant changes in sleep and wake patterns. The PT also marks an abrupt divergence between the sexes in risk for depression and sleep disorders that remains elevated for females across the reproductive lifespan, implicating ovarian hormones (i.e., estradiol (E2)) as a common pathway of risk. Notably, inconsistent schedules during the COVID-19 pandemic have contributed to greater sleep irregularity (especially for adolescents), which is associated with affective impairment and inferior clinical outcomes. The objective of this research is to characterize the pathophysiological impact of E2 on sleep disturbances, endocrine rhythm dysregulation and depressive symptoms in peripubertal females. 44 peripubertal females (ages 11-14, within 1-year post-menarche) provided daily hormone (E1G–urinary metabolite of E2) and mood assessments for one menstrual cycle and completed an 8-day sleep assessment (actigraphy, daily sleep diaries), with cortisol and melatonin circadian measurement (over four days) starting at day 7 of the following menstrual cycle. Minute-to-minute consistency in sleep/wake state over 24-hrs was calculated to index sleep regularity (SRI). A multiple regression model predicted depressive symptoms (CES-DC) from follicular menstrual cycle phase E1G-AUC, sleep regularity index (SRI), cortisol and melatonin AUCs (F(4,18) = 3.833, p=.020, R2=.46). E1G, cortisol-AUC (p<.05) and SRI (marginally, p=.08) contributed to the prediction. Results suggest that greater sleep irregularity, greater follicular estradiol and blunted cortisol may contribute to increased depressive symptoms in peripubertal females, providing mechanistic insight into the estradiol-related sleep and affect disruptions experienced during the pubertal transition.
Click here for large version
Maresin-1, a specialized-pro-resolving mediator of inflammation, demonstrates anti-tumorigenic activity in obesity-driven endometrial cancer (EC) / Orlistat exerts anti-obesity and anti-tumorigenic effects in a transgenic mouse model of endometrial cancer / Sulindac, a COX1/COX2 inhibitor, exhibits anti-tumorigenic effects in obesity-driven models of endometrioid endometrial cancer
Catherine John, MD
Contact: catherine.john@unchealth.unc.edu
 Dr. Catherine John is a current gynecologic oncology fellow at the University of North Carolina. She attended medical school at Oregon Health and Science University and then went on to complete her OBGYN Residency at Cedars Sinai Medical Center. Catherine is passionate about delivering excellent gynecologic oncology care to the women of North Carolina and has spent her research year studying preclinical therapeutic models for the treatment of obesity-driven endometrial cancer in the hope that these targeted therapies will improve the treatment options for patients with all stages of endometrial cancer.
Dr. Catherine John is a current gynecologic oncology fellow at the University of North Carolina. She attended medical school at Oregon Health and Science University and then went on to complete her OBGYN Residency at Cedars Sinai Medical Center. Catherine is passionate about delivering excellent gynecologic oncology care to the women of North Carolina and has spent her research year studying preclinical therapeutic models for the treatment of obesity-driven endometrial cancer in the hope that these targeted therapies will improve the treatment options for patients with all stages of endometrial cancer.
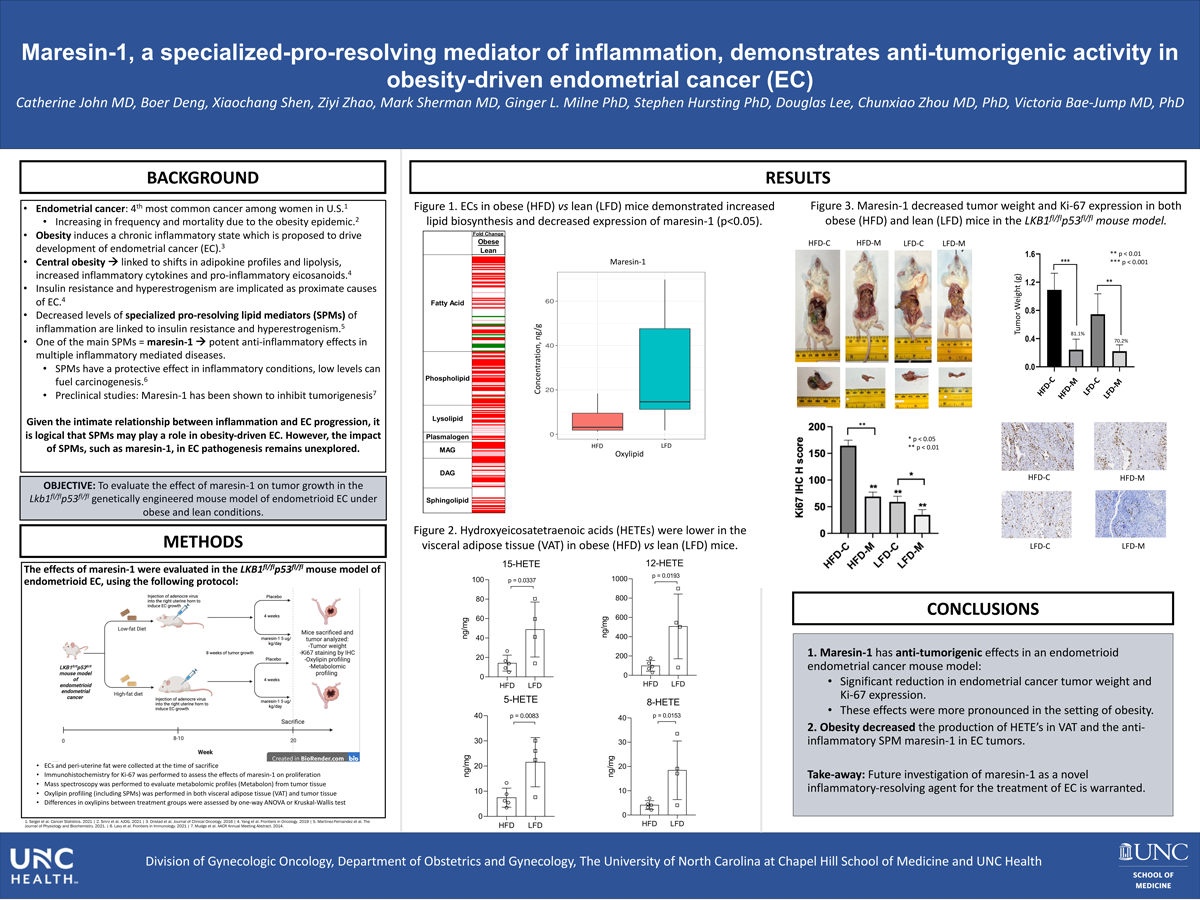
Maresin-1, a specialized-pro-resolving mediator of inflammation, demonstrates anti-tumorigenic activity in obesity-driven endometrial cancer (EC)
Catherine John MD, Beor Deng, Xiaochang Shen, Ziyi Zhao, Mark Sherman, Ginger L. Milne, Stephen Hursting, Douglas Lee, Chunxiao Zhou MD, Victoria Bae-Jump MD, PhD
Objectives: Obesity, with accumulation of visceral fat, induces a chronic inflammatory state which is proposed to drive development of endometrial cancer (EC). Specifically, central obesity is linked to shifts in adipokine profiles and lipolysis, increased inflammatory cytokines and pro-inflammatory eicosanoids, and decreased specialized-pro-resolving lipid mediators (SPMs) of inflammation that may culminate in insulin resistance and hyperestrogenism, which are implicated as proximate causes of EC. Maresin-1, a SPM, has shown potent anti-inflammatory effects in multiple inflammatory mediated diseases. Thus, we aimed to evaluate the effect of maresin-1 on tumor growth in the Lkb1fl/flp53fl/fl genetically engineered mouse model of endometrioid endometrial cancer (EC) under obese and lean conditions.
Methods: Lkb1fl/flp53fl/fl transgenic mice were studied to evaluate the effects of diet-induced obesity and maresin-1 on EC growth. Mice (n=10/group) were fed a low-fat diet (LFD, lean) with 10% calories from fat, or a high-fat diet (HFD, obese) with 60% calories from fat starting at 3 weeks of age. At 8 weeks of age, AdCre was injected into the uterine horn to induce EC. The obese and lean mice were treated with placebo or maresin-1 (5 ug/kg/day) intraperitoneally for 4 weeks. ECs and peri-uterine fat were collected at the time of sacrifice. Immunohistochemistry for Ki-67 (marker of proliferation) was performed to assess the effects of maresin-1 on proliferation. Mass spectroscopy was performed to evaluate metabolomic profiles and measure oxylipins (including SPMs) with validated assays. Differences in oxylipins between treatment groups were assessed by one-way ANOVA or Kruskal-Wallis test.
Results: Mice fed a HFD achieved a mean body weight of 33.2g and developed ECs weighing 1.27g whereas LFD fed mice reached a weight of 23.4g and developed ECs weighing 0.75g (p<0.05). As a correlate, ECs in obese mice showed increased lipid biosynthesis and down-regulation of the potent SPM, maresin-1 (p<0.05). Further, hydroxyeicosatetraenoic acids (HETEs), including 5-HETE, 8-HETE, 12-HETE and 15-HETE were lower in the fat of obese versus lean mice ECs (p<0.001-0.05). Subsequent diet supplementation with maresin-1 for 4 weeks decreased tumor weight by 81.1% (0.24g vs 1.27g; p<0.001) in obese mice and 70.2% (0.22g vs 0.75g; p<0.01) in lean mice, without toxicity or weight change as compared to control mice. Ki-67 expression was greater in the obese-ECs compared to lean-ECs, and maresin-1 significantly decreased Ki-67 in the ECs as compared to placebo-treated controls (p<0.05).
Conclusions: Obesity halted the production of HETEs and the anti-inflammatory SPM maresin-1 in ECs, in parallel with diet-induced weight gain and more rapid EC growth. Administration of exogenous maresin-1 dramatically inhibited tumor growth in Lkb1fl/flp53fl/fl mice, with more pronounced effects in the setting of obesity. We suggest that further investigation of maresin-1 as a novel inflammatory-resolving agent for the treatment of EC is warranted.
Click here for large version
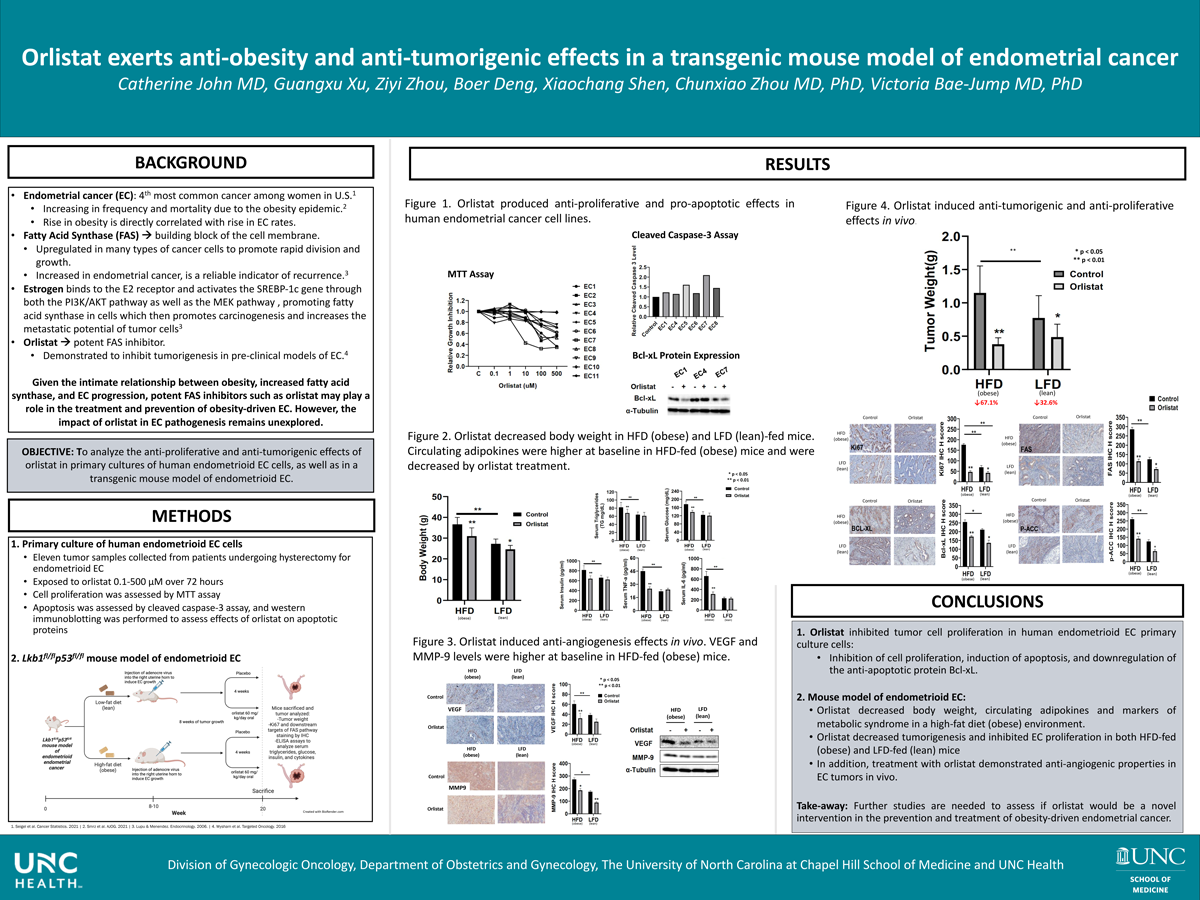
Orlistat exerts anti-obesity and anti-tumorigenic effects in a transgenic mouse model of endometrial cancer
Catherine John, MD, Guangxu Xu, Ziyi Zhao, Boer Deng, Xiaochang Shen, Chunxiao Zhou MD, PhD, Victoria Bae-Jump MD, PhD
Objectives: Endometrial cancer (EC) is strongly associated with obesity, with more than 60% of EC’s identified in obese women. Fatty acid synthase (FAS), a key lipogenic enzyme, is highly expressed in EC and is associated with a poor prognosis. Orlistat, a specific FAS inhibitor, is an FDA approved weight loss medication that has demonstrated anti-tumorigenic activity in pre-clinical cancer models. Thus, we aimed to investigate the anti-tumorigenic effects of orlistat in primary cultures of EC cells and an obesity-driven transgenic EC mouse model.
Methods: Eleven tumor samples were collected from patients undergoing hysterectomy for endometrioid EC and exposed to varying doses of orlistat for 72 hrs. Cell proliferation was assessed by MTT assay. Apoptosis was assessed by cleaved caspase-3 assay. Western immunoblotting was performed to assess effects of orlistat on apoptotic proteins.
To assess the effect of orlistat on endometrioid EC growth, Lkb1fl/flp53fl/fl mice were fed either a low-fat diet (LFD, 10% calories from fat, lean) or a high -fat diet (HFD, 60% calories from fat, obese), starting at 3 wks of age. At 8 wks of age, AdCre was injected into the right uterine horn to induce EC growth. Eight wks after tumor induction, mice were treated with placebo or orlistat (60 mg/kg, oral gavage, daily) for 4 wks. Serum triglycerides, glucose, insulin and cytokines were examined by ELISA assays. Immunohistochemistry (IHC) was used to assess effects of orlistat on proliferation (Ki-67), apoptosis (Bcl-xL) as well as downstream targets of the FAS pathway and angiogenesis in the EC tumors.
Results: Orlistat inhibited cell proliferation in 9 of 11 EC primary cultures (IC50=25.4-146.4 uM). Treatment with orlistat increased cleaved caspase 3 activity (p<0.05), with downregulation of Bcl-xL expression.
Diet-induced obesity (via a HFD) increased mouse body weight by 34.5% and increased tumor weight by 33.4% compared to the LFD group (p<0.01). Orlistat reduced body weight in the HFD and LFD groups by 3.5 and 1.5 grams, respectively (p<0.01). Orlistat inhibited tumor growth by 67.1% and 32.6% in the HFD and LFD groups, respectively (p<0.01). Obese mice had increased circulating triglycerides, glucose, insulin, IL6 and TNF-α levels as compared to lean mice, and all were effectively reduced by orlistat in the obese mice. Orlistat decreased expression of Ki-67, Bcl-xL, FAS and phos-ACC in endometrial tumors from both obese and lean mice (p<0.05), with the greatest effects seen in obese mice. Importantly, obesity increased VEGF and MMP9 expression in the ECs, while orlistat reduced expression of VEGF in the ECs of obese mice and decreased expression of MMP9 in the ECs of both obese and lean mice (p<0.05).
Conclusions: These data suggest that orlistat has promising anti-tumorigenic activity in pre-clinical models of obesity-driven EC; and thus, may have potential as an adjunct therapy in EC prevention and treatment, in addition to impacting weight loss.
Click here for large version
Sulindac, a COX1/COX2 inhibitor, exhibits anti-tumorigenic effects in obesity-driven models of endometrioid endometrial cancer
Catherine John MD, Ziyi Zhou, Xiaochang Shen, Boer Deng, Isabella Strauss, Chunxiao Zhou MD, PhD, Mark Sherman, PhD, Stephen Hursting, PhD and Victoria Bae-Jump MD, PhD
Objectives: Endometrial cancer (EC) incidence and mortality has risen in the U.S., paralleling the rising prevalence of obesity. Obesity is a strong, causal risk factor for EC, which is likely mediated by chronic inflammation and metabolic dysregulation. Sulindac, a potent anti-inflammatory drug that inhibits the COX1 and COX2 pathways, has demonstrated anti-tumorigenic activity in pre-clinical cancer models, but its utility in preventing and treating clinical EC remains unknown. To gain insights into the effects of sulindac on EC development and biology, we analyzed effects of drug in EC cell lines and a transgenic mouse model of endometrioid EC.
Methods: Human endometrioid EC cell lines, HEC-1A and KLE, were exposed to varying concentrations of sulindac (1, 10, 25, 50, and 100 uM), and then assessed for cell proliferation by MTT assay and apoptosis by measuring cleaved caspase-3. Levels of reactive oxygen species (ROS) and mitochondrial membrane potential were detected by DCFH-DA and JC-1 assays, respectively. Western immunoblotting was performed to assess effects on downstream targets related to cellular stress, apoptosis, cell cycle control, and DNA damage.
To assess the effect of sulindac on EC growth, Lkb1fl/flp53fl/fl mice were fed either a low fat diet (LFD, 10% calories from fat, lean) or a high fat diet (HFD, 60% calories from fat, obese). At 8 weeks of age, AdCre was injected into the right uterine horn to induce EC growth. Eight weeks after tumor induction, mice were treated with placebo or sulindac (7.5 mg/kg/day, drinking water) for 4 weeks. Immunohistochemistry was used to assess effects of sulindac on proliferation (Ki-67) and COX2 in the EC tumors.
Results: Sulindac inhibited cell proliferation in a dose-dependent fashion after 72 hours of treatment. Treatment of KLE and HEC-1A cells with varying concentrations of sulindac (6-8 hours) upregulated ROS and caspase 3 production (p<0.01). In both the KLE and HEC-1A cells, sulindac (24 hours) increased the expression of cellular stress proteins such as IRE-1-a and PERK, and decreased expression of the anti-apoptotic protein MCL-1, accompanied by downregulation of extracellular matrix proteins vimentin, slug, and N-cadherin. Treatment with increasing concentrations of sulindac for 8 hours also downregulated mitochondrial membrane potential (p<0.01).
In Lkb1fl/flp53fl/fl mice, HFD promoted tumor growth compared to the LFD mice. Treatment with sulindac reduced tumor weight in both the HFD fed (obese) and the LFD fed (lean) mice, by 63.7% and 75.5% (p < 0.01), respectively. Expression of Ki-67 and COX2 was decreased by sulindac in both obese and lean mice (p<0.01), as compared to their respective control groups.
Conclusions: Sulindac exerts anti-tumorigenic effects in EC cell lines and mouse models of endometrioid EC, suggesting that further studies of this agent in the prevention and treatment of EC is warranted.

Click here for large version
Menopause Status And Regional Body Composition
Kelly Joniak, BS, CSCS, USAW
Contact: kjoniak@ad.unc.edu
 Kelly Joniak is a master’s student in Exercise Physiology at The University of North Carolina at Chapel Hill under the mentorship of Dr. Abbie Smith-Ryan in the Applied Physiology Lab. Kelly’s research interests include nutrition, body composition, and exercise performance, specifically in females. Her thesis work will investigate high intensity interval training performance across the menstrual cycle and between two work to rest ratios. Kelly graduated from The University of Oklahoma with a BS in Health and Exercise Science. She is a Certified Strength and Conditioning Specialist (CSCS) and USA Weightlifting Level 1 coach.
Kelly Joniak is a master’s student in Exercise Physiology at The University of North Carolina at Chapel Hill under the mentorship of Dr. Abbie Smith-Ryan in the Applied Physiology Lab. Kelly’s research interests include nutrition, body composition, and exercise performance, specifically in females. Her thesis work will investigate high intensity interval training performance across the menstrual cycle and between two work to rest ratios. Kelly graduated from The University of Oklahoma with a BS in Health and Exercise Science. She is a Certified Strength and Conditioning Specialist (CSCS) and USA Weightlifting Level 1 coach.
MENOPAUSE STATUS AND REGIONAL BODY COMPOSITION
Kelly E. Joniak1, Sam R. Moore1,2, Hannah E. Cabre1,2, Alex N. Ladan1, Abbie E. Smith-Ryan1,2
1. University of North Carolina at Chapel Hill, Applied Physiology Laboratory, Chapel Hill, NC; 2. Human Movement Science Curriculum, University of North Carolina, Chapel Hill, NC
Metabolic and hormonal changes across the menopause transition may cause adverse alterations in body composition, which are associated with increased disease risk. This pilot study aimed to evaluate the impact of menopause status on bone, muscle, and fat of the dominant thigh. Sixteen healthy women were grouped by menopause status determined using The North American Menopause Society validated Menopause Health Questionnaire: pre-(PRE: eumenorrheic, n=3), peri-(PERI: irregular periods or amenorrheic for <12 months and ³38 years old, n=5), and post-menopausal (POST: amenorrheic for ³12 months, n=8). Bone area (BA; mm2) and cortical density (BCD; mg/cm3), muscle area (MA; mm2) and density (MD; mg/cm3), fat area (FA; mm2), bone-to-muscle (BMR; %), and fat-to-muscle (FMR; %) were assessed using a peripheral quantitative computed tomography (pQCT) scan of the mid-dominant thigh. A one-way ANOVA revealed no significant difference between groups for BA, BCD, MA, MD, FA, or BMR (p>0.05). Although not statistically significant, FA was greater in POST vs PRE (mean difference±standard error: 5930.9±2441.2mm2), but lower than PERI (-281.5±2055.7mm2). MA POST was lower than PRE (-1779.4±1160.6mm2) and PERI (-961.4±977.3mm2). FMR was significantly different between groups (p=0.038) with PRE demonstrating a significantly lower ratio than POST (-66.8±23.2%; p=0.039), with no difference between PERI and POST (-9.4±19.6%; p=1.000). Despite a small sample size, these findings suggest there may be a shift in body composition from PRE to PERI with few changes occurring from PERI to POST, indicating potential for stage specific nutrition and exercise recommendations.
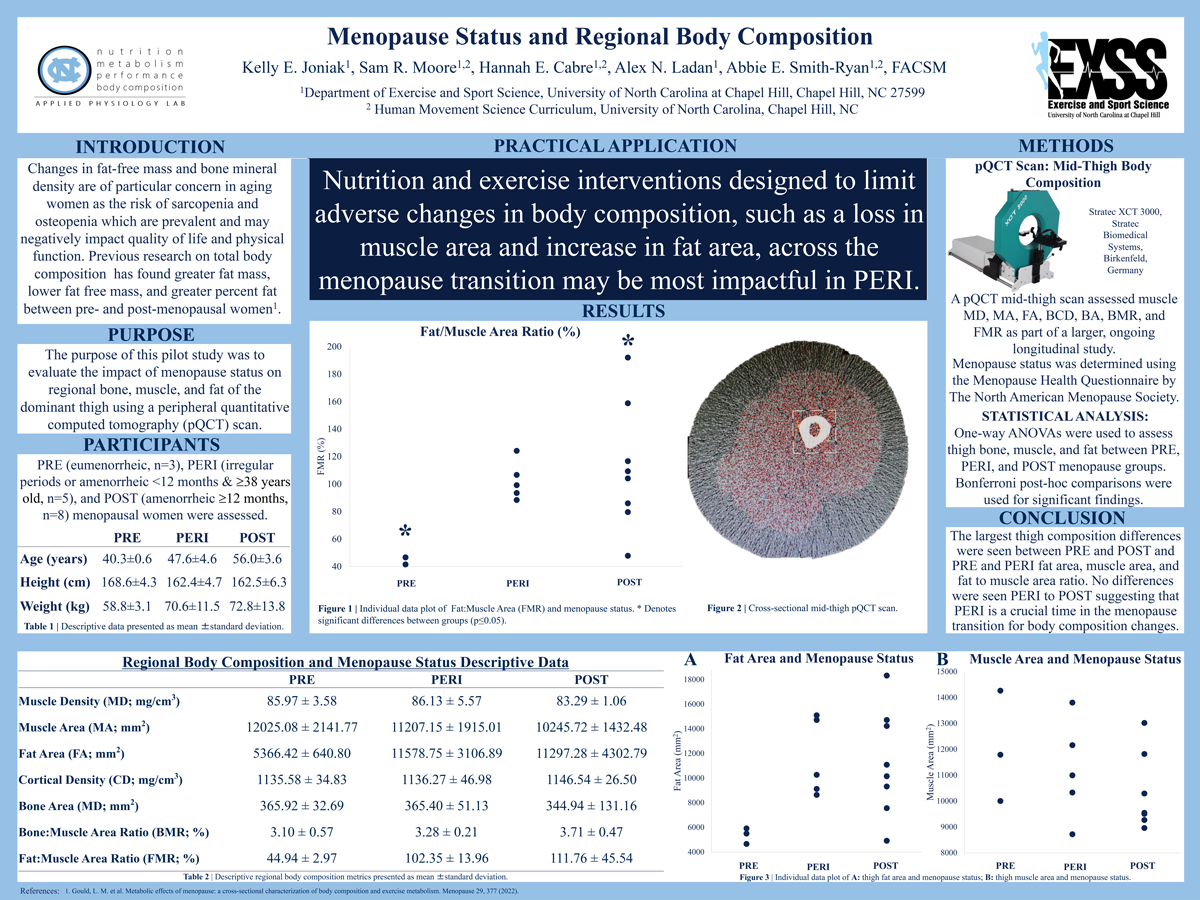
Click here for large version
Stress and Resilience Across Gestation Among Pregnant Individuals with Psychiatric Disease
Mary Kimmel, MD
Contact: mary_kimmel@med.unc.edu
Mary Kimmel, MD is an Assistant Professor and Medical Director of the UNC’s Perinatal Psychiatry Inpatient Unit (PPIU). Her clinical expertise is in treating women’s mood and anxiety disorders and in treating psychiatric disorders and other mental health issues during pregnancy and the postpartum time period. Dr. Kimmel’s research interests include studying changes of systems such as the microbiota-gut-brain axis, the stress system and the immune system across pregnancy in relation to the development of maternal depression and anxiety and in relation to the child’s psychological development in order to develop treatments.
Stress and Resilience Across Gestation Among Pregnant Individuals with Psychiatric Disease
Authors: Mary Kimmel, Tracy Manuck
Objective: The effects of prenatal stress and resilience on maternal and offspring health may vary by the gestational age of exposure and the presence of psychiatric comorbidity. We investigated whether perceived stress and resilience varied by gestational age, among those with and without psychiatric disease.
Methods: Analysis of 2 prospective cohorts, 2019-2022. Pregnant persons were recruited <28 weeks’. Consenting participants completed the Perceived Stress Scale (PSS, range 0-40; ‘high’ stress = score ≥ 21) and the Brief Resilience Scale (BRS, range 1-5; ‘low’ resilience = score <3) surveys. Linear regression was used to evaluate whether PSS and BRS scores varied by gestational age among those with and without current or previous psych disease, including anxiety, depression, prior postpartum depression, PTSD, and bipolar disorder.
Results: The study included 1,036 participants, with 49.1% having psychiatric disease. Cohort characteristics are shown in Table 1. Those with psychiatric disease had higher PSS scores and were more likely to have scores ≥21; BRS scores were lower and more likely to be <3 among those with psychiatric disease. Stress decreased with gestational age, while resilience increased for both groups (Figure 1). In regression models adjusting for confounders, psych disease, but not gestational age, remained associated with PSS (β=3.7, 95% CI 2.9,4.5, p<0.001) and BRS (β=-0.34, 95% CI 0.43-0.26, p<0.001) scores.
Conclusions: Though trends suggesting lower stress and higher resilience occur over the course of gestation, those pregnant individuals with past or current psych disease have higher stress and lower resilience throughout pregnancy and may be particularly vulnerable to stressors.

Click here for large version
Body Composition Methods Across The Menstrual Cycle
Alex Ladan, BS
Contact: aladan2@unc.edu
 Alex Ladan is a 1st year Master’s student in Exercise Physiology at The University of North Carolina at Chapel Hill under the direction of Dr. Abbie Smith-Ryan in the Applied Physiology Lab. Alex’s research interests include female physiology, body composition and exercise performance specifically as they relate to women’s health and athletics. Her upcoming project will focus on the impact of the menstrual cycle on fatigue and recovery from acute high-intensity interval training. Alex graduated from the University of Illinois with a BS in Kinesiology where she previously studied exercise and the gut microbiome.
Alex Ladan is a 1st year Master’s student in Exercise Physiology at The University of North Carolina at Chapel Hill under the direction of Dr. Abbie Smith-Ryan in the Applied Physiology Lab. Alex’s research interests include female physiology, body composition and exercise performance specifically as they relate to women’s health and athletics. Her upcoming project will focus on the impact of the menstrual cycle on fatigue and recovery from acute high-intensity interval training. Alex graduated from the University of Illinois with a BS in Kinesiology where she previously studied exercise and the gut microbiome.
BODY COMPOSITION METHODS ACROSS THE MENSTRUAL CYCLE
Alex N. Ladan1, Hannah E. Cabre1,2, Sam R. Moore1,2, Kelly E. Joniak1, Abbie E. Smith-Ryan1,2
1. Applied Physiology Laboratory, Department of Exercise Sport and Science, University of North Carolina at Chapel Hill, Chapel Hill, NC; 2. Human Movement Science Curriculum, University of North Carolina, Chapel Hill, NC
Exercise and nutrition recommendations are often provided to females based upon body composition and training goals. Evaluating the sensitivity of body composition technology may inform female specific recommendations. The purpose of this study was to examine the impact of menstrual cycle (MC) phase and hormonal contraception on body composition measurements of lean mass (LM) and fat mass (FM). 60 healthy women (mean±standard deviation [SD]; Age: 26.5±7.0 yrs, BMI: 22.5±3.7 kg/m2) that had a regular, naturally occurring MC or were using a non-hormonal intrauterine device (EUM; n=19), who were monophasic oral contraceptive (OC) users (n=21) or had a hormonal-intrauterine device (H-IUD; n=20) were measured using dual-energy x-ray absorptiometry (DXA), BodPod, multi-frequency bioelectrical impedance spectroscopy (BIS), and a four compartment criterion (4C) method after a 12 hour fast. Participants were measured during the follicular phase/placebo pills (FP) or luteal phase/active pills (LP). MC had no significant impact on body composition outcomes (p>0.04); there were no differences between the FP and LP for DXA FM (Mean difference: 0.05±2.0 kg) or LM (MD: 0.02±0.8 kg; p>0.05), for BIS FM (MD: 0.01±0.9 kg) or LM (MD: 0.05±1.1 kg), or 4C FM (MD: 0.03±2.0 kg) or LM (MD: 0.00±2.2 kg). BodPod resulted in significantly greater LM in the FP vs LP (MD: 0.77±3.1 kg; p=0.032) with no change in FM. Results did not vary across contraception type. Changing hormonal landscapes of MC phase and hormonal contraceptives appear to have little effect on the accuracy of body composition measurements.
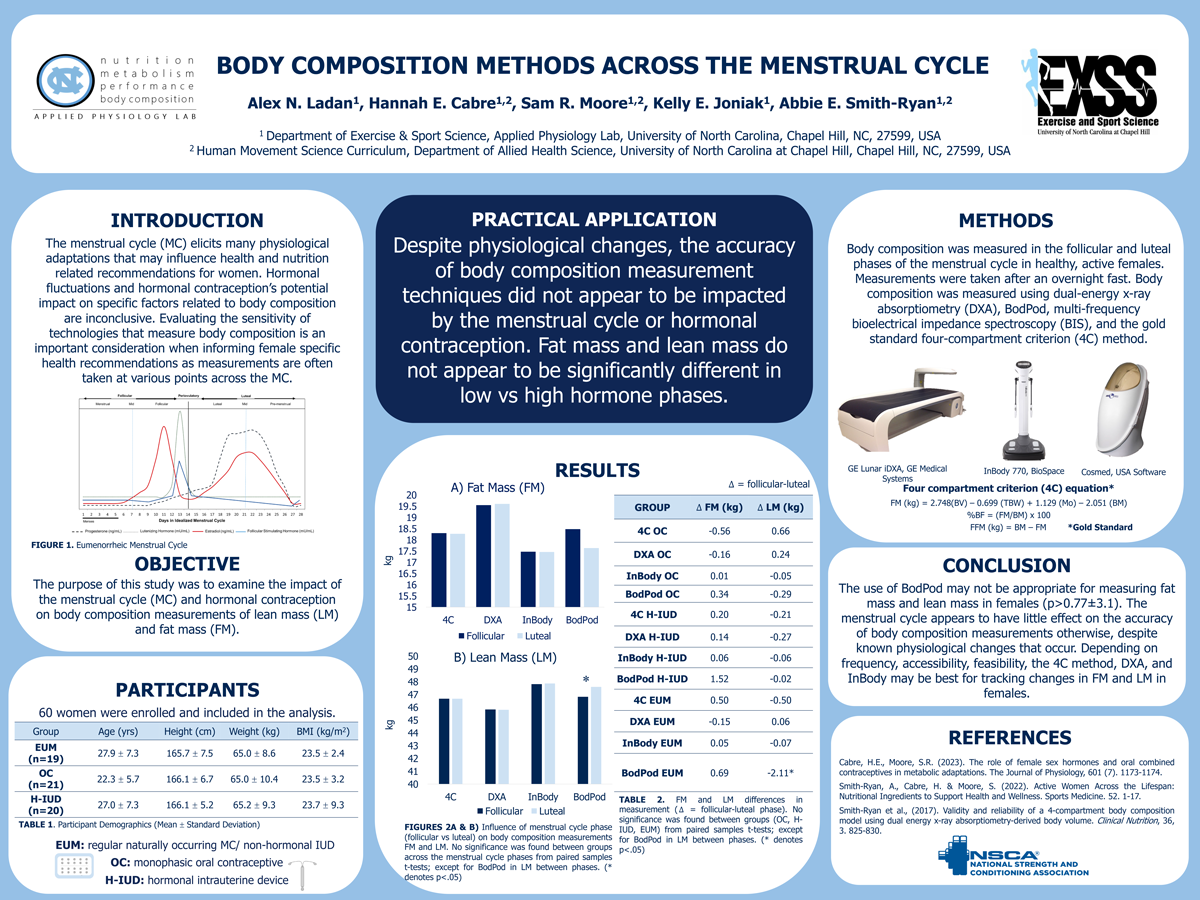
Click here for large version
Gestational exposure to phthalates and phthalate replacements and preeclampsia diagnosis: a longitudinal study
Erin McNell, BSc
Contact: eemcnell@email.unc.edu
 Erin McNell is a Ph.D. Candidate in the Curriculum in Toxicology and Environmental Medicine at the University of North Carolina at Chapel Hill. She is completing her dissertation research at the National Institute of Environmental Health Sciences under the joint mentorship of Dr. Kelly Ferguson and Dr. Suzanne Fenton, studying the relationship between prenatal chemical exposures and complicated pregnancies. Her work is a unique mix of epidemiology and traditional toxicology. Erin is originally from Buffalo, New York, and received a B.S. in Biochemistry from St. Bonaventure University in 2020. She is passionate about advocating for the improvement of maternal and women’s health and is currently a member of the Women’s Health Multidisciplinary Consortium Inaugural Trainee Cohort. Outside of her studies, Erin enjoys spending time outdoors, reading, and taking her dog to the park.
Erin McNell is a Ph.D. Candidate in the Curriculum in Toxicology and Environmental Medicine at the University of North Carolina at Chapel Hill. She is completing her dissertation research at the National Institute of Environmental Health Sciences under the joint mentorship of Dr. Kelly Ferguson and Dr. Suzanne Fenton, studying the relationship between prenatal chemical exposures and complicated pregnancies. Her work is a unique mix of epidemiology and traditional toxicology. Erin is originally from Buffalo, New York, and received a B.S. in Biochemistry from St. Bonaventure University in 2020. She is passionate about advocating for the improvement of maternal and women’s health and is currently a member of the Women’s Health Multidisciplinary Consortium Inaugural Trainee Cohort. Outside of her studies, Erin enjoys spending time outdoors, reading, and taking her dog to the park.
Gestational exposure to phthalates and phthalate replacements and preeclampsia diagnosis: a longitudinal study
Phthalates and their replacements are found in numerous consumer products. Gestational phthalate exposure may disrupt hormonal balance, contributing to pregnancy complications such as preeclampsia, a hypertensive disorder that affects 5-10% of pregnancies. Most studies assessing phthalate exposure and preeclampsia utilize exposure biomarkers from a single timepoint, which could miss the critical period of susceptibility or result in exposure misclassification. This study aims to investigate the prospective association between gestational exposure to phthalates and their replacements throughout pregnancy and diagnosis of preeclampsia. The study included 291 pregnant persons recruited between 2017-2020 within the Human Placenta and Phthalates Study. Urine samples were obtained at up to 8 visits throughout gestation, from which metabolites of phthalates and replacements were quantified. The geometric mean for each metabolite was calculated from repeated measures in early- (12-15 weeks), middle- (16-25 weeks), late- (26-38 weeks), and overall-gestation. Logistic regression models of preeclampsia were adjusted for maternal age, body mass index, race and ethnicity, education, smoking, and study site. Participants identified predominantly as non-Hispanic Black (43%) and were widely exposed to phthalates and replacements. Incidence of preeclampsia was 8.6%. The adjusted odds ratios (OR) of preeclampsia were above the null but not statistically significant for several phthalate and replacement metabolites. For mono-ethyl phthalate (MEP), the OR increased from early (OR=0.87, 95% confidence interval [CI]=0.57, 1.32), to middle (OR=1.31, 95% CI=0.83, 2.06), to late (OR=1.39, 95% CI=0.91, 2.14) pregnancy. This racially diverse, U.S.-based prospective cohort provides insight into the temporality of associations between gestational phthalate exposure and preeclampsia.

Click here for large version
Body Composition, Activity, & Nutrition In Menopause
Sam Moore, MS, CSCS, USAW
Contact: smoore@unc.edu
 Sam R. Moore, MS, CSCS, USAW is an applied sport scientist and Human Movement Science Curriculum doctoral student at the UNC-Chapel Hill’s School of Medicine, working under the direction of Dr. Abbie Smith-Ryan. Her research interests center around metabolic and performance effects of female sex hormones for women specific interventions to improve health and performance across the lifespan. Sam’s scholarly record demonstrates a strong commitment to both research and translation, having successfully published 6 peer-reviewed articles, in addition to 24 peer-reviewed abstract presentations at regional and national conferences. Sam has also been featured on 14 various podcasts and given 28 guest lectures, conference presentations, and invited talks on topics ranging from facilitating gender equity in sport through strength and conditioning to integrated strategic periodization models for team sports. Prior to Carolina, Sam was with the NC State Wolfpack from 2019-2021 as the Director of Sport Science and Assistant Strength & Conditioning Coach; the first woman to serve in this role in the NCAA. At NCSU, Sam’s primary responsibilities were designing and implementing a revolutionary and evidence informed framework of women’s specific training design based on the hormonal landscape of the Wolfpack female athletes.
Sam R. Moore, MS, CSCS, USAW is an applied sport scientist and Human Movement Science Curriculum doctoral student at the UNC-Chapel Hill’s School of Medicine, working under the direction of Dr. Abbie Smith-Ryan. Her research interests center around metabolic and performance effects of female sex hormones for women specific interventions to improve health and performance across the lifespan. Sam’s scholarly record demonstrates a strong commitment to both research and translation, having successfully published 6 peer-reviewed articles, in addition to 24 peer-reviewed abstract presentations at regional and national conferences. Sam has also been featured on 14 various podcasts and given 28 guest lectures, conference presentations, and invited talks on topics ranging from facilitating gender equity in sport through strength and conditioning to integrated strategic periodization models for team sports. Prior to Carolina, Sam was with the NC State Wolfpack from 2019-2021 as the Director of Sport Science and Assistant Strength & Conditioning Coach; the first woman to serve in this role in the NCAA. At NCSU, Sam’s primary responsibilities were designing and implementing a revolutionary and evidence informed framework of women’s specific training design based on the hormonal landscape of the Wolfpack female athletes.
BODY COMPOSITION, ACTIVITY, & NUTRITION IN MENOPAUSE
Sam R. Moore1,2, Hannah E. Cabre1,2, Kelly E. Joniak1, Alex N. Ladan1, Abbie E. Smith-Ryan1,2
1. Applied Physiology Laboratory, Department of Exercise and Sport Science, University of North Carolina at Chapel Hill, Chapel Hill, NC 27599; 2. Human Movement Science Curriculum, Department of Health Sciences, University of North Carolina, Chapel Hill, NC
This study aimed to characterize relationships between body composition (percent body fat [%BF]; lean mass [LM]), activity (light [LOW]; moderate [MOD]; vigorous [VIG] active mins/day), nutrition (carbohydrate to protein ratio [C:P]) and menopausal symptoms (TMS) in 72 females categorized as: pre- (PRE: eumenorrheic), peri- (PERI: irregular periods or amenorrheic for <12 months and ³38 years old), or post-menopausal (POST: amenorrheic for ³12 months). TMS and C:P were determined using The North American Menopause Society and Diet History III Validated Questionnaires, respectively. Body composition was evaluated using a whole-body dual energy x-ray absorptiometry scan. Activity minutes were collected from wearable fitness trackers. Bivariate correlations were used to analyze relationships, with stepwise linear regressions applied to evaluate independent effects of significant correlations. Significant associations were observed between %BF and VIG with TMS (r=0.464; p<0.001 and r=-0.245; p=0.038 respectively), %BF and VIG (r=-0.239; p=0.043), and C:P and LM (r=-0.267; p=0.023). C:P demonstrated relationships with LM (r=-0.425; p=0.038) within PERI, and %BF (r=-0.600; p=0.002) within POST. %BF and VIG were significant predictors for TMS across groups (R2=0.215 and R2=0.060, respectively), but only maintained within group significance for PERI (R2=0.442; p<0.001 and R2=0.163; p=0.05, respectively). C:P was a significant predictor for PERI LM (R2=0.181), and POST %BF (R2=0.360). There is a sizeable impact of body fat accumulation and intense physical activity, while C:P appears to influence body composition differently across the menopause transition. Exercise and nutrition interventions to alleviate body composition changes and TMS should be stage specific.
Funding Acknowledgement: This study was supported by the UNC Center for Women’s Health Research.
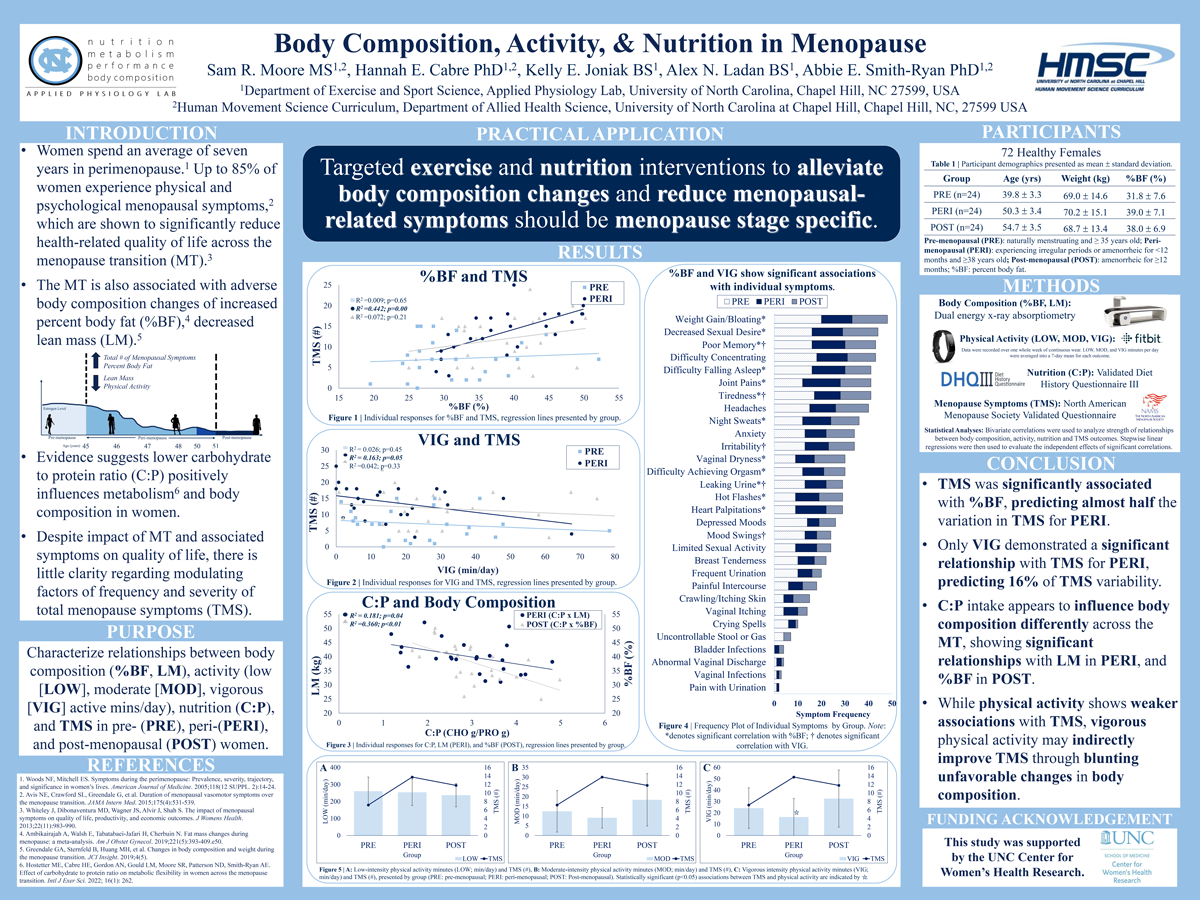
Click here for large version
Reactions of Spanish-speaking birthing parents and companions after communication from inpatient postpartum health care team members
Marisue Peralta
Contact: marisue@ad.unc.edu
 Marisue Peralta is an undergraduate student at the University of North Carolina at Chapel Hill, studying Medical Anthropology with a minor in Chemistry. Marisue plans to go to medical school, but for now, she wants to get involved in the social sciences, humanities, and biological sciences to help those deemed most vulnerable in our own healthcare system.
Marisue Peralta is an undergraduate student at the University of North Carolina at Chapel Hill, studying Medical Anthropology with a minor in Chemistry. Marisue plans to go to medical school, but for now, she wants to get involved in the social sciences, humanities, and biological sciences to help those deemed most vulnerable in our own healthcare system.
Neha Saggi is an undergraduate student at the University of North Carolina at Chapel Hill, studying Health Policy and Management and Biology, with a Chemistry minor. She is an aspiring physician with a strong interest in the intersection of women’s health, health policy, and social justice.
Kathia Pena is an engineer working as a Research Assistant for the Perinatal team of the UNC OB/GYN dept. She has over 16 years of experience recruiting and doing follow-up for a wide variety of studies from Maternal Fetal Medicine and Industrial trials. Her last completed study was the Chronic Hypertension during Pregnancy Study (CHAP) done at nationwide level and where UNC was the second highest recruiter and currently ready to start the follow up as a second phase. Her experience involves the prenatal care in clinic, labor and delivery and postpartum unit, working with mothers and babies through the study participation, their follow up and postpartum transition.
Dr. Kristin Tully is a medical anthropologist and Research Assistant Professor in the Department of Obstetrics and Gynecology at the University of North Carolina at Chapel Hill. Her expertise is engaging birthing individuals, family members, clinicians, and community members through mixed methods research to understand health priorities and co-generate solutions to meet their needs. Broadly, her program of work advances reproductive justice by addressing what people need to know, feel, and have happen to be safe and well.
Reactions of Spanish-speaking birthing parents and companions after communication from inpatient postpartum health care team members
Marisue Peralta, Neha Simran Saggi, Kathia Pena, Kristin P. Tully
Effective communication among patients, companions, and their health care team members is critical for safe, respectful care. During inpatient postpartum care, topics of communication span maternal and infant health, warning signs, and care planning. The extent to which information is clear, relevant, and culturally aligned has received little attention, and patients-companions with Limited English Proficiency navigate the intersecting challenge of access to language concordant services.
The Postnatal Patient Safety Learning Laboratory is a multidisciplinary research study to evaluate the delivery of health care that contributes to perinatal mortality and morbidity. Following UNC IRB approval (#19-1900), filming occurred on the postnatal unit of NC Women’s Hospital between August-December 2020. This analysis addresses the reactions of Spanish-speaking families following health care team member communication with them in the 12 hours leading to discharge.
Over 66 hours were coded, applying definitions of positive, confusing, and negative verbalizations within the 10-minutes after health care team member exited rooms. Birthing parents and companions discussed 20 health topics over 50 exchanges, with 4 positive reactions, 24 instances of confusion, and 14 negative reactions.
Findings suggest that interpretations services should be more readily accessible and, broadly, there is opportunity for more connection and meaningful communication for equitable health services.
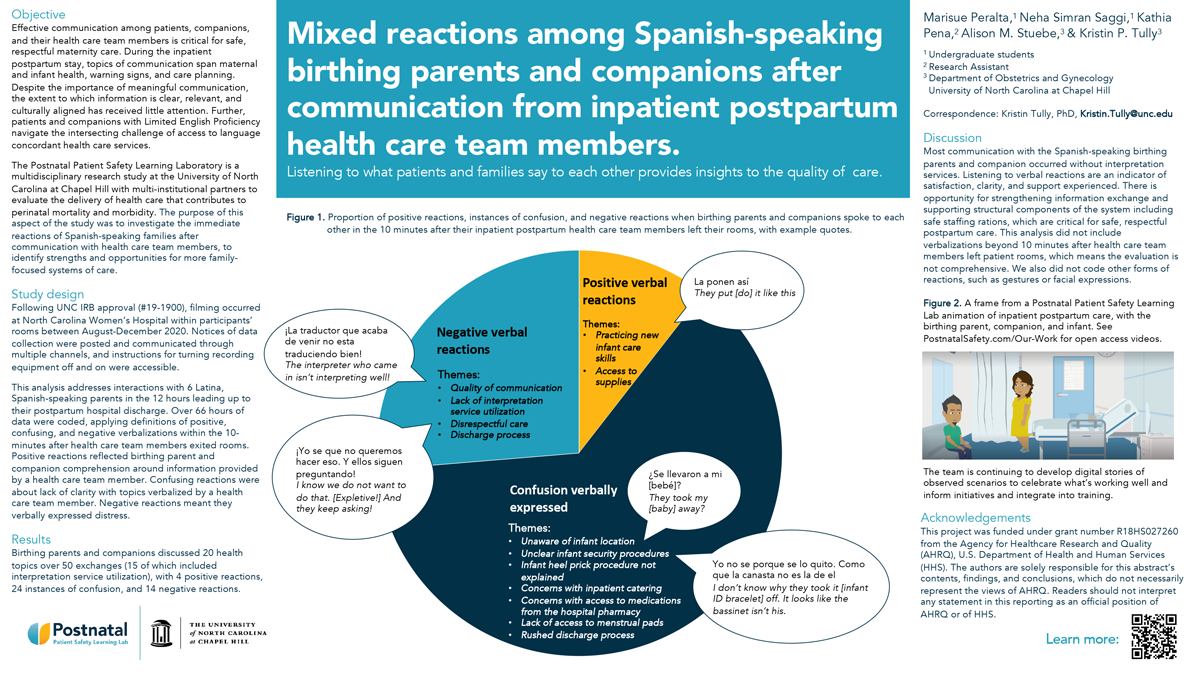
Click here for large version
Body mass index mediates the association between disordered eating and cardiometabolic risks: evidence from the China Health and Nutrition Survey
Baiyu Qi, MPH
Contact: baiyuqi@email.unc.edu
Baiyu Qi is a third year PhD student in the Department of Epidemiology at University of North Carolina at Chapel Hill. She is interested in both genetic and environmental risk factors of eating disorders and comorbid diseases, particularly among underrepresented populations. Before attending UNC, she received a BS in Chemistry from Hong Kong Polytechnic University and an MPH from Boston University.
Body mass index mediates the association between disordered eating and cardiometabolic risks: evidence from the China Health and Nutrition Survey
Baiyu Qi1, MPH, Gabrielle E. Cooper2, BS, Laura M. Thornton2, PhD, Ruyue Zhang3, PhD, Shuyang Yao3, PhD, Annie Green Howard4,5, PhD, Penny Gordon-Larsen5,6, PhD, Shufa Du5,6, PhD, Huijun Wang7, PhD, Bing Zhang7, PhD, Cynthia M. Bulik2,3,6, PhD, Kari E. North1, PhD, Melissa A. Munn-Chernoff2, PhD
1. Department of Epidemiology, Gillings School of Global Public Health, University of North Carolina at Chapel Hill, Chapel Hill, NC, USA; 2. Department of Psychiatry, University of North Carolina at Chapel Hill, NC, USA; 3. Department of Medical Epidemiology and Biostatistics, Karolinska Institutet, Stockholm, Sweden; 4. Department of Biostatistics, Gillings School of Global Public Health, University of North Carolina at Chapel Hill, Chapel Hill, NC, USA; 5. Carolina Population Center, University of North Carolina at Chapel Hill, Chapel Hill, NC, USA; 6. Department of Nutrition, Gillings School of Global Public Health, University of North Carolina at Chapel Hill, Chapel Hill, NC, USA; 7. National Institute for Nutrition and Health, Chinese Center for Diseases Control and Prevention, Beijing, PR China
We examined the association between disordered eating (DE) and cardiometabolic risks (CMR) and the mediating role of body mass index (BMI) in 2,005 Chinese women (aged 18-50 years) from the 2015 China Health and Nutrition Survey exam. Loss of control eating, restraint, shape concern, and weight concern were assessed using self-report questionnaires. Eight CMRs were measured by trained staff. Generalized linear models examined associations between DE traits with CMRs. We tested whether BMI mediated significant associations using structural equation modeling. Shape concern was associated with systolic [β (95% confidence interval): 0.06 (0.02, 0.10)] and diastolic blood pressure [0.07 (0.03, 0.11)], and high-density lipoprotein cholesterol [HDL-C; -0.08 (-0.12, -0.04)]. Weight concern was associated with diastolic blood pressure [0.06 (0.02, 0.10)], triglycerides [0.06 (0.02, 0.10)], and HDL-C [-0.11 (-0.14, -0.07)]. BMI at least partially mediated these associations: greater DE was associated with higher BMI, and higher BMI was associated with lower HDL-C and higher other CMRs. Shape and weight concerns captured concerns related to high weight in our sample, rather than concerns among individuals with normal/low weight with eating disorder pathology. Findings could assist screening individuals at risk and identifying modifiable targets of prevention and intervention for CMR.

Click here for large version
Perfluoroalkyl Substances (PFAS) Induce Platinum Resistance in Ovarian Cancer by Improving Mitochondrial Membrane Potential and Increasing Mitochondrial DNA Copy Number
Brittany Rickard
Contact: brickard@live.unc.edu
 I am currently a fourth-year graduate student in the Curriculum in Toxicology and Environmental Medicine. I first learned about, and became passionate for, toxicology when I participated in the Toxicology, Health, and Environmental Disease High School Program at Rutgers University in 2014. This program taught me about environmental exposures and how they shape health outcomes, and ultimately led me to pursue my undergraduate degree in Pharmacology & Toxicology at the Philadelphia College of Pharmacy. Although I entered graduate school with a background in toxicology, I’ve dreamt of studying ovarian cancer for over a decade. In February of 1997, six months before I was born, my grandmother was diagnosed with stage IV ovarian cancer and given less than six months to live. This diagnosis meant that she would likely not live long enough to meet me, her twelfth and final grandchild. Luckily, soon after her diagnosis, my grandmother became part of a clinical trial investigating a combination of platinum and taxane-based chemotherapy, and this clinical trial enabled my grandmother to live with advanced-stage ovarian cancer for seven years. Although I was too young to realize it then, a clinical trial enabled me to meet and remember my grandmother, and I couldn’t be more thankful to the bench researchers and clinicians involved. My grandmother’s story has motivated me to pursue a career in ovarian cancer research, and I am extremely thankful to have found mentors who share similar passions and support my career goal of improving outcomes for ovarian cancer patients.
I am currently a fourth-year graduate student in the Curriculum in Toxicology and Environmental Medicine. I first learned about, and became passionate for, toxicology when I participated in the Toxicology, Health, and Environmental Disease High School Program at Rutgers University in 2014. This program taught me about environmental exposures and how they shape health outcomes, and ultimately led me to pursue my undergraduate degree in Pharmacology & Toxicology at the Philadelphia College of Pharmacy. Although I entered graduate school with a background in toxicology, I’ve dreamt of studying ovarian cancer for over a decade. In February of 1997, six months before I was born, my grandmother was diagnosed with stage IV ovarian cancer and given less than six months to live. This diagnosis meant that she would likely not live long enough to meet me, her twelfth and final grandchild. Luckily, soon after her diagnosis, my grandmother became part of a clinical trial investigating a combination of platinum and taxane-based chemotherapy, and this clinical trial enabled my grandmother to live with advanced-stage ovarian cancer for seven years. Although I was too young to realize it then, a clinical trial enabled me to meet and remember my grandmother, and I couldn’t be more thankful to the bench researchers and clinicians involved. My grandmother’s story has motivated me to pursue a career in ovarian cancer research, and I am extremely thankful to have found mentors who share similar passions and support my career goal of improving outcomes for ovarian cancer patients.
Perfluoroalkyl Substances (PFAS) Induce Platinum Resistance in Ovarian Cancer by Improving Mitochondrial Membrane Potential and Increasing Mitochondrial DNA Copy Number
Brittany P. Rickard1, Suzanne E. Fenton1,2, Imran Rizvi1,3,4,5
1. Curriculum in Toxicology & Environmental Medicine, University of North Carolina at Chapel Hill, Chapel Hill, NC; 2. Mechanistic Toxicology Branch, National Institute of Environmental Health Sciences, Research Triangle Park, NC; 3. Joint Department of Biomedical Engineering, University of North Carolina at Chapel Hill, Chapel Hill, NC 27599, USA; North Carolina State University, Raleigh, NC 27606, USA; 4. Lineberger Comprehensive Cancer Center, University of North Carolina School of Medicine, Chapel Hill, NC 27599, USA; 5. Center for Environmental Health and Susceptibility, University of North Carolina at Chapel Hill, Chapel Hill, NC 27599, USA
Perfluoroalkyl substances (PFAS) are widespread, persistent environmental contaminants that frequently pollute drinking water supplies worldwide. While these chemicals have been linked to a plethora of adverse outcomes, studies have shown that PFAS exposure can increase risk of infertility and ovarian cancer. Ovarian cancer is the most lethal gynecologic malignancy with a ~65% mortality rate. One contributing factor to its high lethality is resistance to platinum-based chemotherapy, the standard of care for ovarian cancer treatment. Importantly, our recently published study showed, for the first time, that select PFAS induce platinum resistance in two ovarian cancer cell lines. Since platinum-resistant ovarian tumor populations often display increased mitochondrial networks and enhanced bioenergetic capacities, we hypothesized that PFAS induce alterations to mitochondrial biology. To determine the effect of PFAS on mitochondrial health, we evaluated changes in mitochondrial membrane potential (DYm) and mitochondrial DNA (mtDNA) copy number. After PFAS exposure alone and in combination with carboplatin, a platinum-based chemotherapeutic, DYm increased compared to controls by up to 46%, whereas carboplatin alone decreased DYm by ~50%. Increased DYm after PFAS exposure alone and in combination with carboplatin can signify improved mitochondrial functioning. As an additional mitochondrial parameter, mtDNA copy number was evaluated and found to be elevated by up to 41% in exposure groups where PFAS-induced platinum resistance was observed. Increased mtDNA copy number in cancer cells may enhance bioenergetic capabilities, promoting cancer progression. Together, these findings implicate alterations to mitochondrial functioning as a mechanism underlying PFAS-induced chemotherapy resistance.
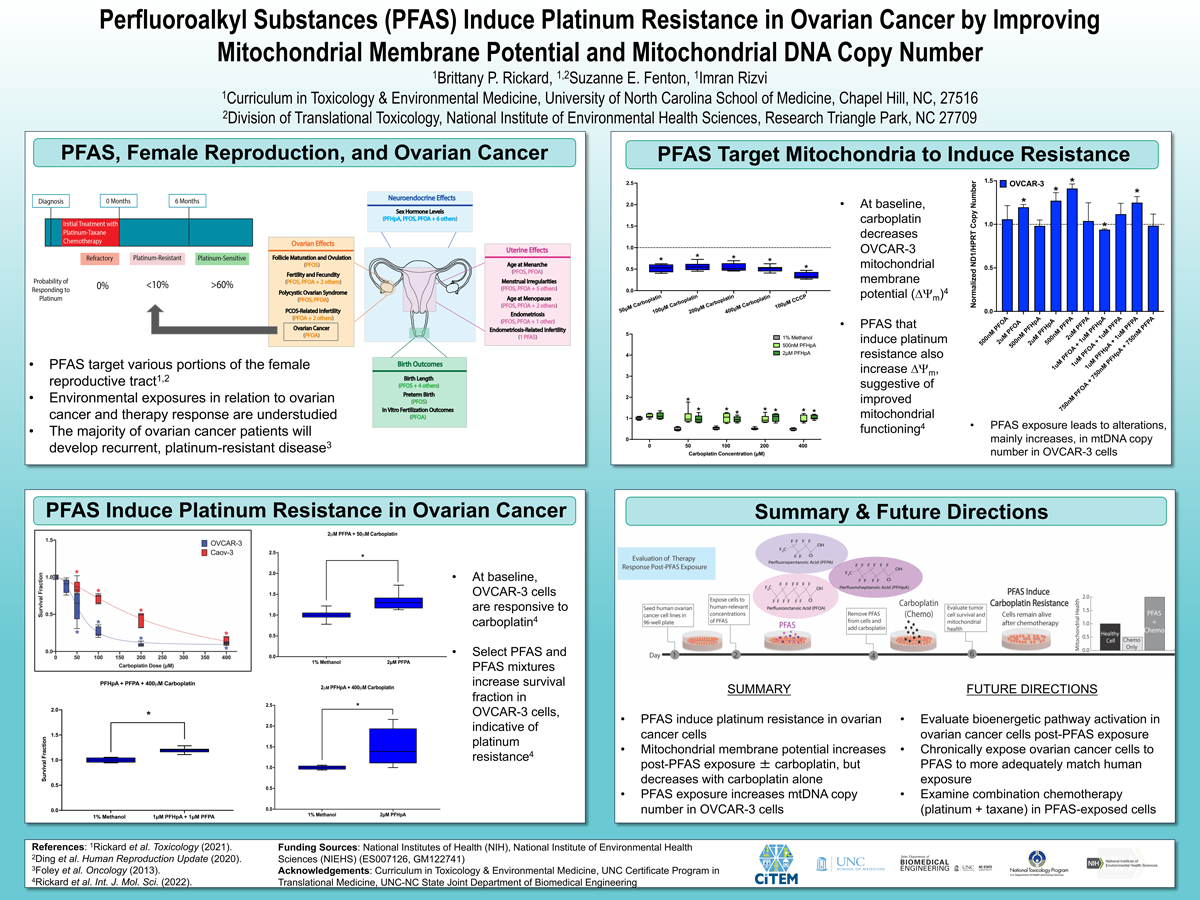
Click here for large version
Coordinating postpartum cardiac care for patients with preterm preeclampsia: maternal healthcare provider perspectives / Provision of high-quality care for patients who experience preterm preeclampsia: maternal healthcare providers’ perceptions
Stanthia Ryan, MD
Contact: stanthia.ryan@unchealth.unc.edu
 Stanthia Ryan is a second year resident in the Department of Obstetrics and Gynecology at the University of North Carolina Hospitals. She grew up in Boston, Massachusetts and completed medical school at Georgetown University School of Medicine in Washington, DC. She is passionate about healthcare disparities and reducing maternal mortality. She is planning to pursue a career in Maternal Fetal Medicine.
Stanthia Ryan is a second year resident in the Department of Obstetrics and Gynecology at the University of North Carolina Hospitals. She grew up in Boston, Massachusetts and completed medical school at Georgetown University School of Medicine in Washington, DC. She is passionate about healthcare disparities and reducing maternal mortality. She is planning to pursue a career in Maternal Fetal Medicine.
Coordinating postpartum cardiac care for patients with preterm preeclampsia: maternal healthcare provider perspectives
Alexandria C. Kraus, MD, Johanna Quist-Nelson, MD, Alison M. Stuebe, MD, MSc, Omar M Young, MD, Elizabeth Volz, MD, Kristin P. Tully, PhD
Objective: To document maternal healthcare providers’ perspectives on coordinating care for birthing people who experienced preterm preeclampsia with severe features and were referred to an innovative postpartum clinic for cardiac risk stratification.
Study design: Maternal healthcare providers completed a semi-structured interview between March 2022 to May 2022. Providers were approached for participation based on their involvement in delivering care for birthing people with preeclampsia. The interviews were audio-recorded, professionally transcribed, and checked for accuracy. Responses were iteratively coded for inductive narrative analysis.
Results: Ten maternal healthcare providers participated. Their roles were obstetricians (n=4), nurses (n=2), advanced practice provider (n=1), family medicine physician (n=1), certified nurse midwife (n=1), and pregnancy care coordinator (n=1). Nine participants self-identified as non-Hispanic white, and one participant did not respond with a preferred race/ethnicity. The patient populations served were diverse in payer status, acuity, rurality, and primary language. Support for referrals, sensitivity to patient priorities, and clarification of clinical workflow all emerged as themes (Table 1). Collectively, providers deemed the patient experience of utmost priority when coordinating postpartum cardiac care (Figure 1).
Conclusions: Maternal healthcare providers view support for referrals, sensitivity to patient priorities, and clarification of clinical workflow as integral in coordination of postpartum cardiac care for birthing people. Documentation of birthing persons’ experiences with postpartum cardiac care will be a crucial next step in aligning perspectives important to both maternal care providers and birthing people.
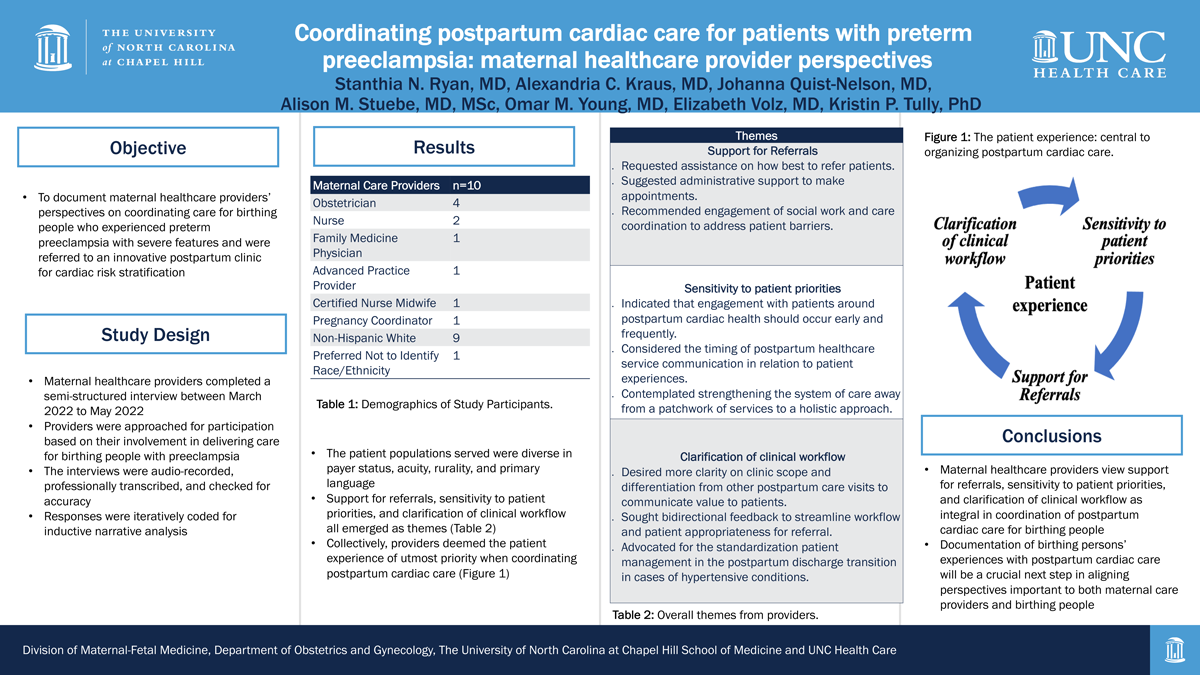
Click here for large version
Provision of high-quality care for patients who experience preterm preeclampsia: maternal healthcare providers’ perceptions
Alexandria C. Kraus, MD, Johanna Quist-Nelson, MD, Alison M. Stuebe, MD, MSc, Omar M Young, MD, Elizabeth Volz, MD, Kristin P. Tully, PhD
Objective: To document maternal healthcare providers’ perceptions on how high-quality care might be best structured to equitably serve birthing people who experienced preterm preeclampsia with severe features and consequently are at high risk of cardiovascular disease following childbirth.
Study design: Maternal healthcare providers completed a semi-structured interview between March 2022 to May 2022. Providers were approached for participation based on their involvement in delivering care for birthing people with preeclampsia. The interviews were audio-recorded, professionally transcribed, and checked for accuracy. Responses were iteratively coded for inductive narrative analysis.
Results: Ten maternal healthcare providers participated. Their roles were obstetricians (n=4), nurses (n=2), advanced practice provider (n=1), family medicine physician (n=1), certified nurse midwife (n=1), and pregnancy care coordinator (n=1). Nine participants self-identified as non-Hispanic white, and one did not respond with a preferred race/ethnicity. The patient populations served were diverse in payer status, acuity, rurality, and primary language. Providers offered several examples of successes and areas for improvement in the provision of high-quality care (Table 1). They considered the use of personalized communication with birthing people a standard for excellent patient care. Nonetheless, providers also felt strongly that more attention should be conferred on identifying and eliminating biased healthcare practices; many proposed an interrelated approach for accomplishing this objective (Figure 1).
Conclusions: Maternal healthcare providers supplied several examples of how services are already optimally structured to provide equitable care, while also offering several suggestions for improvement. Detailing birthing persons’ thoughts on what constitutes high-quality, unbiased, and respectful clinical care is an essential next step.

Click here for large version
Effects of Sex Steroid Manipulation on Anhedonia in Women With a History of Postpartum Depression
Danielle Swales, PhD
Contact: danielle_swales@med.unc.edu
 Dr. Danielle Swales is a postdoctoral research fellow in the Reproductive Mood Disorders T32 program in the Department of Psychiatry at UNC. She received her Ph.D. in Clinical Child Psychology from the University of Denver and completed her internship at Children’s Hospital Colorado. Her program of research broadly investigates the biological and psychosocial determinants of mental health during pregnancy and the postpartum period, as well as the impact of perinatal distress on child development. The long-term goal of her research is to continue uncovering the pathophysiology of perinatal mood disorders and identify novel targets for intervention that can confer two generation benefits.
Dr. Danielle Swales is a postdoctoral research fellow in the Reproductive Mood Disorders T32 program in the Department of Psychiatry at UNC. She received her Ph.D. in Clinical Child Psychology from the University of Denver and completed her internship at Children’s Hospital Colorado. Her program of research broadly investigates the biological and psychosocial determinants of mental health during pregnancy and the postpartum period, as well as the impact of perinatal distress on child development. The long-term goal of her research is to continue uncovering the pathophysiology of perinatal mood disorders and identify novel targets for intervention that can confer two generation benefits.
EFFECTS OF SEX STEROID MANIPULATION ON ANHEDONIA IN WOMEN WITH A HISTORY OF POSTPARTUM DEPRESSION
Danielle A. Swales1, Lauren Schiff2, David Rubinow1, and Crystal E. Schiller1
1. Department of Psychiatry, University of North Carolina at Chapel Hill, Chapel Hill, NC, United States; 2. Department of Obstetrics and Gynecology, University of North Carolina at Chapel Hill, Chapel Hill, NC, United States.
The hormonal changes of pregnancy can trigger depression in vulnerable women. Less work has explored whether sex steroid changes trigger anhedonia. In the current study we investigated the effects of experimentally controlled reproductive steroid exposure on anhedonia in women with and without a history of postpartum depression (PPD). The hormone states of pregnancy and parturition were simulated in non-pregnant, euthymic women with a history of PPD (n = 11) and healthy controls (n = 12) by inducing hypogonadism (via administration of gonadotropin-releasing hormone [GnRH] agonist, leuprolide acetate [Lupron]), adding back supraphysiologic doses of estradiol (E2) and progesterone (P4) for 2 weeks (“addback”), and then withdrawing both steroids (“withdrawal”). Symptoms of depression were assessed at each study visit using the Inventory of Depression and Anxiety Symptoms (IDAS-II). Anhedonia was assessed using the reverse-coded wellbeing scale of the IDAS-II and the Behavioral Inhibition System and Behavioral Activation System (BIS/BAS) scales. Women with a history of PPD reported an increase in anhedonia from baseline to hormone addback on the IDAS reverse-coded wellbeing scale (t = -2.8, p = .011) and the BAS Drive scale (t = 2.4, p = .026). Depression and anhedonia levels did not change from baseline to addback for control participants with no PPD history (all p’s > .250). Findings support the role of sex steroids in perinatal-onset depression and suggest that sex-steroid changes can trigger anhedonia in at-risk women.
Acknowledgements: NIMH R21 MH119615-01, NIMH T32 MH093315
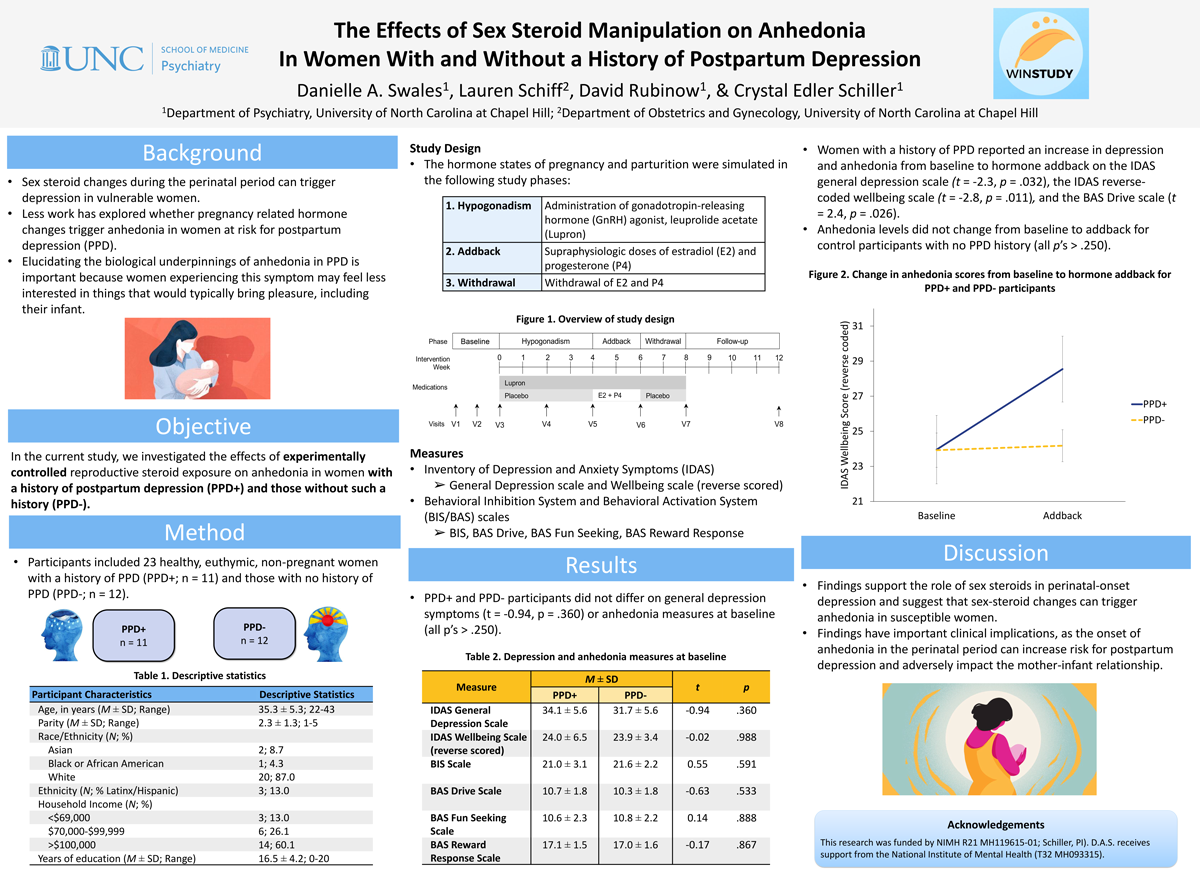
Click here for large version
Single center experience using single-gene-NIPT to evaluate fetal risk assessment of autosomal recessive conditions
Asha Talati, MD
Contact: asha_talati@med.unc.edu
 Asha Talati MD, MSCR is a Clinical instructor in Maternal Fetal Medicine and fellow in Medical Genetics and Genomics at University of North Carolina, Chapel Hill. She will begin her faculty appointment as Assistant Professor of Maternal Fetal Medicine & Medical Genetics & Genomics July 2023. Dr. Talati completed medical school and residency at Case Western Reserve University in Cleveland, Ohio, where she was a part of the Alpha Omega Alpha Honor Society. She served as chief resident at University Hospitals Case Medical Center in Obstetrics & Gynecology 2016-2017. From 2017-2019, Dr. Talati completed the Women’s Health Research fellowship and earned her Masters of Science in Clinical Research at UNC while an active member of the division of General Obstetrics & Gynecology. Following this, she completed her Maternal Fetal Medicine and Medical Genetics & Genomics fellowship in 2023. She currently runs a Maternal Fetal Medicine, Medical Genetics clinic at University of North Carolina at Chapel Hill, focusing on reproductive counseling for parents with rare disease or pregnancies at increased risk of genetic conditions. Her research focuses on equity in access to prenatal genetic diagnosis and ethical implementation of advanced sequencing strategies in the prenatal period.
Asha Talati MD, MSCR is a Clinical instructor in Maternal Fetal Medicine and fellow in Medical Genetics and Genomics at University of North Carolina, Chapel Hill. She will begin her faculty appointment as Assistant Professor of Maternal Fetal Medicine & Medical Genetics & Genomics July 2023. Dr. Talati completed medical school and residency at Case Western Reserve University in Cleveland, Ohio, where she was a part of the Alpha Omega Alpha Honor Society. She served as chief resident at University Hospitals Case Medical Center in Obstetrics & Gynecology 2016-2017. From 2017-2019, Dr. Talati completed the Women’s Health Research fellowship and earned her Masters of Science in Clinical Research at UNC while an active member of the division of General Obstetrics & Gynecology. Following this, she completed her Maternal Fetal Medicine and Medical Genetics & Genomics fellowship in 2023. She currently runs a Maternal Fetal Medicine, Medical Genetics clinic at University of North Carolina at Chapel Hill, focusing on reproductive counseling for parents with rare disease or pregnancies at increased risk of genetic conditions. Her research focuses on equity in access to prenatal genetic diagnosis and ethical implementation of advanced sequencing strategies in the prenatal period.
Single center experience using single-gene-NIPT to evaluate fetal risk assessment of autosomal recessive conditions
Asha N. Talati, MD MS Emily E. Hardisty MS CGC, Kelly L. Gilmore MS CGC, Rachel Veazey MS CGC, Ginger Hocutt MS CGC, Smriti Singh MS CGC, Madeline Dyke MS CGC, Neeta L. Vora MD
University of North Carolina at Chapel Hill Division of Maternal Fetal Medicine, Reproductive Genetics
Objective: To evaluate partner screening and diagnostic testing after reflex single gene NIPT (sgNIPT) is used to determine fetal risk of an autosomal recessive (AR) condition is performed after maternal carrier status is detected.
Study Design: Retrospective cohort of patients undergoing carrier screening with the Billion to One Unity Screen in a tertiary care center from 3/20 – 7/22. This test screens for maternal carrier status for five AR conditions: spinal muscular atrophy (SMA), cystic fibrosis (CF), alpha thalassemia (AT), beta thalassemia (BT), and sickle cell disease (SCD). If maternal carrier status is detected, test reflexes to sgNIPT from cell free placental DNA to estimate low or high risk fetal status for the AR condition. Data was abstracted including maternal characteristics, results of testing, and follow up of results such as amniocentesis or partner carrier screening. Analysis utilized descriptive statistics.
Results: 229 patients with singleton pregnancies had the Unity Screen during the study period. Median gestational age at time of screening was 90 days (IQR 79, 106). Sixty-two (27%) of individuals were identified as carriers for at least one of the tested conditions; 9 were carriers of more than one condition. Reflex to sgNIPT was sent on 71 genes; of those, 94% provided a fetal risk assessment. Distribution of low risk and high risk results per gene is shown in Figure 1. All individuals with carrier status were offered partner testing as appropriate and/or fetal diagnosis with amniocentesis. Among the 56 people with low risk fetal results, 3 (5%) had partner carrier testing and 0 had diagnostic testing. Among the 6 individuals with high-risk fetal results, 2 had partner testing and 1 had diagnostic testing.
Conclusions: Few patients who utilized sgNIPT accepted follow up paternal screening or fetal diagnostic testing, even if high fetal risk was suspected. Additional work to assess patient understanding of results and how this may impact uptake of diagnostic testing and partner screening is a future direction to improve use of this testing method.
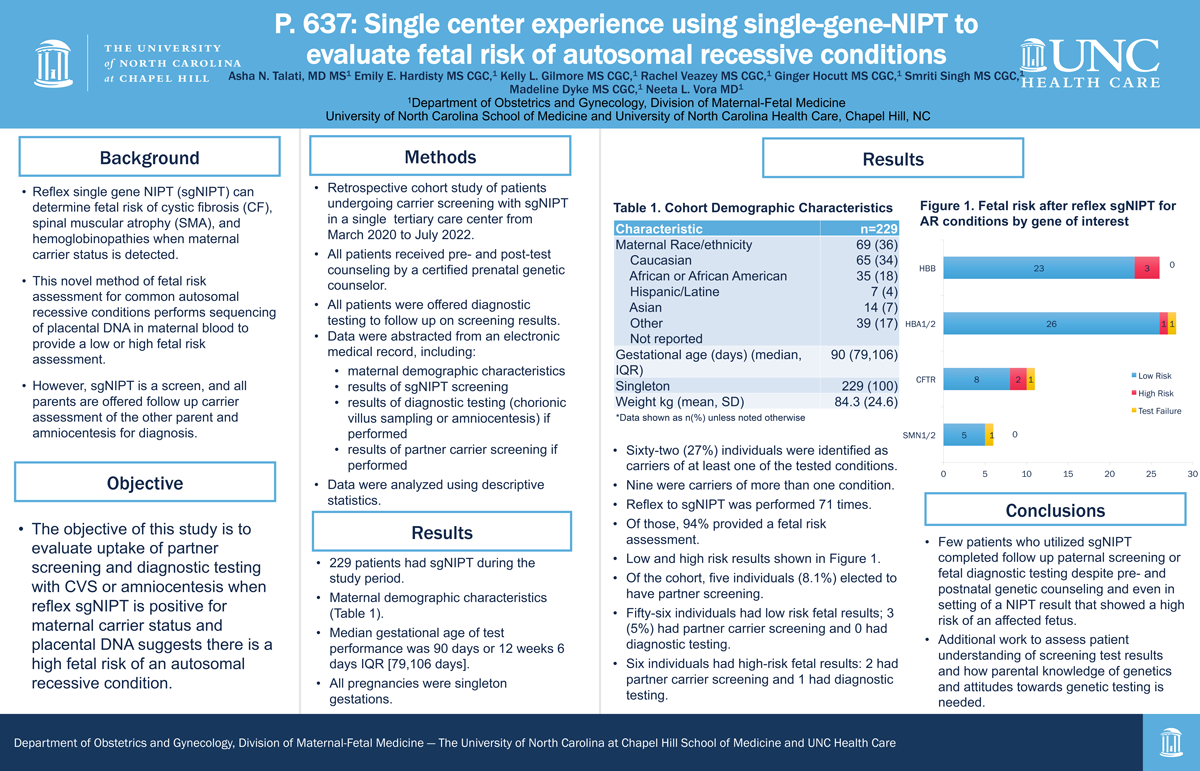
Click here for large version
Implementation of a Patient Safety Bundle for Pregnancy-Related Severe Hypertension in the Outpatient Setting / Using Training and Simulation to Improve Respectful Maternity Care
E. Nicole Teal, MD, MPH
Contact: nicole.teal@unchealth.unc.edu
 Nicole Teal is a third year Maternal-Fetal Medicine Fellow at the University of North Carolina at Chapel Hill. A native Floridian, she received her undergraduate degree from the University of Florida in Family, Youth and Community Sciences with minors in Leadership and Education. She earned her medical degree and her Masters in Public Health from the University of South Florida. She then completed residency in Obstetrics and Gynecology at the University of California at San Francisco. During fellowship, Dr. Teal’s has focused her research on using implementation science as a strategy to improve health equity.
Nicole Teal is a third year Maternal-Fetal Medicine Fellow at the University of North Carolina at Chapel Hill. A native Floridian, she received her undergraduate degree from the University of Florida in Family, Youth and Community Sciences with minors in Leadership and Education. She earned her medical degree and her Masters in Public Health from the University of South Florida. She then completed residency in Obstetrics and Gynecology at the University of California at San Francisco. During fellowship, Dr. Teal’s has focused her research on using implementation science as a strategy to improve health equity.
Implementation of a Patient Safety Bundle for Pregnancy-Related Severe Hypertension in the Outpatient Setting
Teal EN, Farahi N, Rogers PL, Westgard CM, Harper KD, Moretto R, Oluyadi FO, Lin FC, Menard MK, and rest of ACHIEVE Team
This was a pilot study aiming to define effective strategies for implementation of a community-informed patient safety bundle for severe hypertension (HTN) during pregnancy in the outpatient setting.
The AIM Inpatient Severe HTN in Pregnancy Patient Safety Bundle was adapted for use in 3 Federally Qualified Health Centers (FQHCs) using a community-engaged approach. It was piloted from 9/2021 to 6/2022 with using training, coaching and simulation.
Pre-intervention, clinical teams consisting of a medical assistant, nurse, provider (midwife or physician), and pharmacy staff at each FHQC participated in a simulation to establish a baseline. The simulation involved a patient actor who was found to have severe HTN during a prenatal visit. Teams were observed and evaluated on key behaviors demonstrating recognition of and response to severe HTN in pregnancy. Teams then received training on the adapted outpatient severe HTN management algorithm. Post-training, simulation was repeated, and teams were again evaluated. The primary outcome was team recognition of and response to severe HTN pre/post-intervention. Mean pre/post-intervention scores were compared.
Twenty teams from 3 FHQCs received the intervention. In the pre-intervention simulation, teams scored a mean of 78% overall on recognition of and response to severe HTN. Post-training, they improved to a mean of 95% (p=0.006). Statistically significant gains were made on these key behaviors: identification of need to treat HTN, provision of timely treatment, and escalation to higher level of care.
Training, coaching, and simulation were effective for improving outpatient recognition of and response to severe HTN during pregnancy in this pilot study. These strategies hold promise for the implementation of an outpatient severe HTN patient safety bundle.

Click here for large version
Using Training and Simulation to Improve Respectful Maternity Care
Teal EN, Harper KD, Farahi N, Lightfoot AF, Menard MK, and rest of ACHIEVE Team
The WHO defines respectful maternity care (RMC) as care provided to birthing people that “maintains their dignity, privacy and confidentiality, ensures freedom from harm and mistreatment, and enables informed choice.” We sought to train clinical teams on patients’ perception of RMC and evaluate the teams’ implementation of RMC in simulated patient encounters. First, we used themes from patient focus groups to build a Respectful Care Reflection Tool (RCR). We then conducted a baseline simulation of an episode of severe hypertension in a pregnant patient actor with 20 clinical teams at three federally qualified health clinics. After the simulation, each team member, the patient actor, and an observer from the research team completed an RCRT Next, we provided training to the teams on management of severe hypertension as well as patients’ perception of RMC. We then repeated the simulation. We compared RCR scores pre/post-simulation. Clinical team members scored themselves an average of 30% on respectful care pre-training and 46% post (p=0.002). The patient actor scored the teams an average of 62% pre-training and 89% post (p-0.004). The observer scored the teams an average of 40% pre-training and 66% post (p=0.003). By self-reflection, patient perception, and observer evaluation, teams scored significantly better post-training than pre-training. The limitations of this study include that everyone completing the RCR knew whether it was for pre- or post-training and the patient actor was not from a diverse background. Nevertheless, this is the first study we are aware of to specifically train clinical teams on RMC and evaluate the impact of the training on simulated patient encounters. This represents a promising strategy for improving provision of RMC.
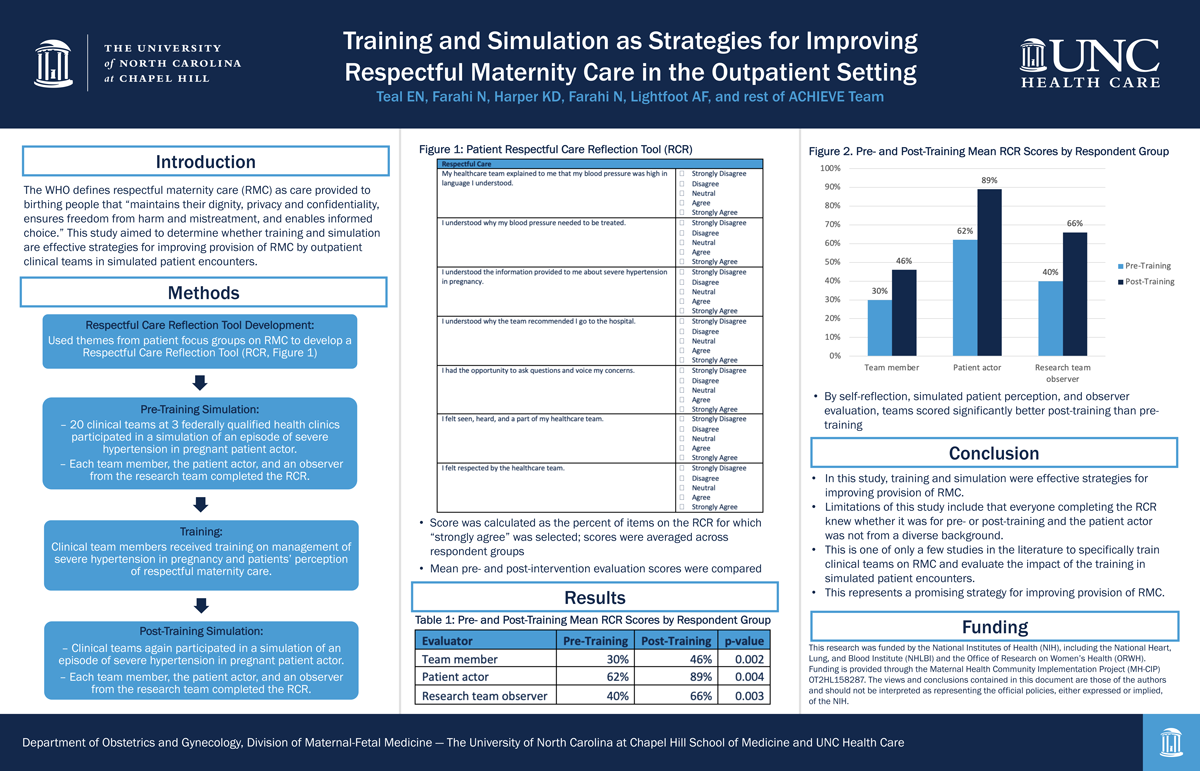
Click here for large version
Exclusion of Women from Phase I Trials: Perspectives from Investigators and Research Oversight Officials
Margaret Waltz, PhD
Contact: margaret_waltz@med.unc.edu
Margaret Waltz is a Research Scientist in the Department of Social Medicine and Center for Bioethics at UNC Chapel Hill. She received her PhD in Sociology from Case Western Reserve University. She then received a Postdoctoral Research Fellowship from the UNC Center for Genomics and Society. Waltz has been involved in a wide array of mixed methods empirical research projects at UNC. The primary focus of her research investigates the ethical, social, and policy issues that emerge as a result of developments in genomic technologies, population and clinical genomic screening, and patient receipt of genetic test results. She has also studied the experiences of providers/patients and researchers/participants in situations of uncertainty or ethical dilemmas. Additionally, she has interviewed and surveyed numerous scientists from around the world on their perceptions of professional norms around emerging technologies or scientific policy changes. Finally, Waltz has a keen interest in how gender inequalities are perpetuated within and by medical and scientific institutions.
Exclusion of Women from Phase I Trials: Perspectives from Investigators and Research Oversight Officials
Over the past 30 years, progress has been made to increase women’s representation in clinical research. However, women continue to be underrepresented in Phase I clinical trials—those trials that test the safety and tolerability of investigational drugs, often on healthy individuals. As sex-based differences in adverse drug reactions are often linked to drug dose, pivotal safety information in Phase I trials is often insufficiently—and inequitably—captured for females. Yet, there has been little attention to how clinical investigators and those charged with overseeing the ethical conduct of these trials perceive the barriers to women’s inclusion in Phase I trials. To address this gap, we report on 22 interviews with US Phase I investigators and institutional review board (IRB) members. Our findings indicate that although they acknowledged the importance of including women in clinical trials, investigators and IRB members justified women’s exclusion from Phase I trials by citing the need to manage women’s reproductive potential. In particular, we identified four key themes that informants used to warrant women’s exclusion from Phase I trials: (1) the structure of the drug development system itself, (2) fears about risks to potential fetuses, (3) distrust of women to prevent pregnancy, and (4) concerns about risks and burdens to institutions from resulting pregnancies. We argue that these rationales reflect structural and cultural barriers to women’s inclusion in clinical research that ultimately fail to respect female research participants as persons, highlighting the need for broad-based solutions.
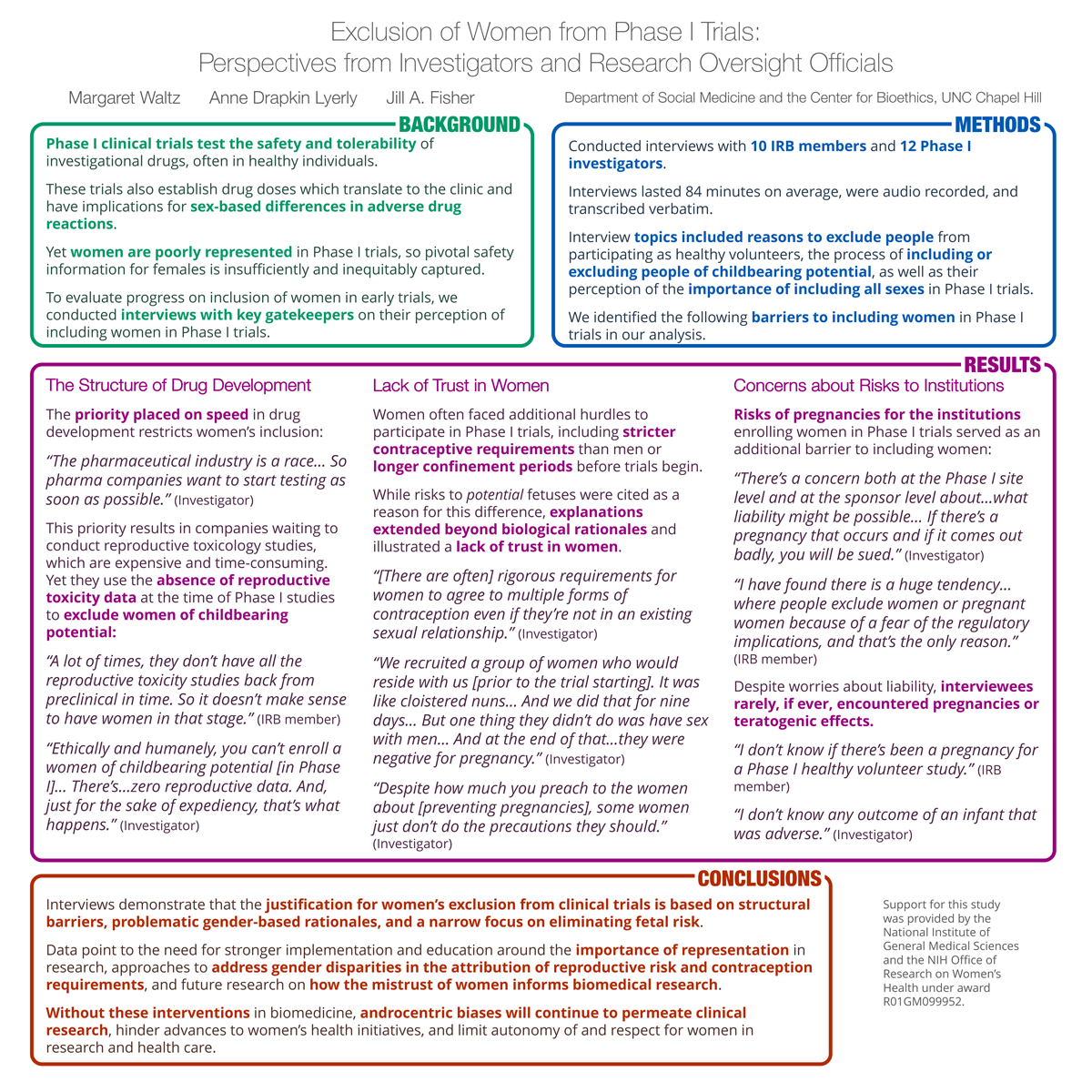
Click here for large version
Pre-diagnosis Symptoms Reported Among Endometrial Cancer Survivors / Gynecologic care for people experiencing incarceration: a systematic review
Meredith Wise, MD
Contact: meredith_wise@med.unc.edu
 Meredith Wise is a general obstetrics and gynecology clinical instructor and reproductive health research fellow and will complete her Master of Science in Clinical Research through UNC’s Gillings School of Global Public Health this spring. Her research interests include gynecologic cancer prevention and early detection, substance use and carceral health, and early pregnancy complications.
Meredith Wise is a general obstetrics and gynecology clinical instructor and reproductive health research fellow and will complete her Master of Science in Clinical Research through UNC’s Gillings School of Global Public Health this spring. Her research interests include gynecologic cancer prevention and early detection, substance use and carceral health, and early pregnancy complications.
Pre-diagnosis Symptoms Reported Among Endometrial Cancer Survivors
Meredith K Wise, Theo Wu, Victoria Bae-Jump, Andy F Olshan, Hazel B Nichols
Introduction: Incidence and mortality of endometrial cancer (EC) are increasing, with significant outcome disparities between Black and White patients. Postmenopausal bleeding is generally accepted as the most common symptom of EC. However, symptom experience may vary according to the presence of comorbid conditions which that more common among Black women. The aim of this study is to describe the distribution of pre-diagnosis symptoms and reporting by endometrial cancer (EC) survivors by race.
Methods: We used baseline survey data to describe the distribution of 6 menstrual and 7 non-menstrual prediagnosis symptoms among Black and White participants. We assessed survivors’ pre-diagnosis knowledge about postmenopausal bleeding. We calculated prevalence ratios (PR) and 95% confidence intervals (CI) with Poisson regression for the association between race and symptom experience.
Results: Among a total of 355 participants, 120 self-identified as Black or African American and 213 as White. After adjusting for age, Black women were 8% less likely to report experiencing any menstrual symptoms compared to White (PR=0.92; 95% CI 0.84-0.99). Non-menstrual symptoms were reported by 69% of Black women and 78% of White women (age-adjusted PR=0.90; 0.79, 1.04). Only 38 (21%) of participants reported knowing that EC can cause bleeding after menopause prior to their diagnosis.
Discussion: Pre-diagnosis symptoms were similar by race. The low rate of knowledge pertaining to postmenopausal bleeding as a symptom of endometrial cancer suggests opportunity for improved patient education. Further study is needed to assess how pre-diagnosis experiences contribute to Black-White EC outcome disparities.
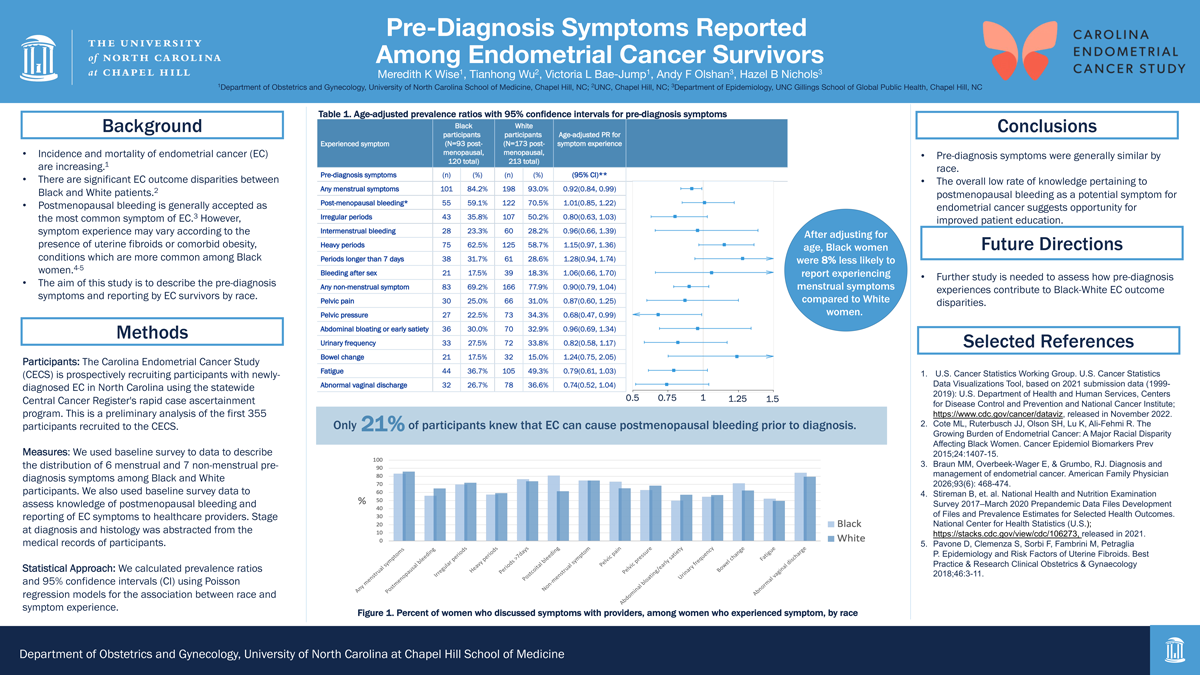
Click here for large version
Gynecologic care for people experiencing incarceration: a systematic review
Authors: Meredith K. Wise, MD, Elana Jaffe, Sreya Upputuri, Andrea K. Knittel, MD, PhD
Background: Gynecologic care is a vital component of medical care for people experiencing incarceration. A review of gynecologic conditions and management in carceral settings may identify best practices and areas where improvement and further research is needed. Research questions: We sought to answer questions of prevalence, special considerations for management, access, and experiences of benign and malignant gynecologic conditions. Methods: We searched six databases with a detailed search strategy using a systematic review method.
Results: Full text review is ongoing. At this point, 101 studies have met criteria for inclusion in the review. Conditions addressed include cervical cancer, abnormal uterine bleeding, dysmenorrhea, normal menstruation, menopause, vaginitis, and urogynecology conditions.
Conclusions: While the review includes a large number of studies, they are heterogenous with few studies focused on each individual condition. Moreover, the gynecologic conditions in question for this review were often not the primary purpose of the included studies, but rather a small component of a broader study. When completed, this review will give an overview of the current state of the literature pertaining to common benign and malignant conditions and identify gaps in the literature where further research is needed to care for this unique population.