“I want individuals of color to realize that an endocrinologist can help with some of these issues.”
Joyce runs a nonprofit, Bridging the Gap CDC, in North Carolina that aims to connect resources with individuals who are in need. She’s also a wife, mother, and grandmother that loves to garden and help out on her family’s farm. But over the past five years, Joyce has experienced a gradual increase in symptoms that almost forced her to give up her nonprofit work and hobbies.
Five years ago, Joyce noticed that she was always cold, even in the summer. “I could never get warm,” recalled Joyce. Joyce also shared that she struggled with weight gain and was diagnosed with type 2 diabetes in 2017. “It’s always been a hard situation,” said Joyce. “Gaining weight and losing weight. I’ve done that quite a bit.”
Two years ago, Joyce noticed a significant decrease in her energy level and began to struggle with daily fatigue. It became difficult for Joyce to sleep through the night. She discussed her concerns with her primary care physician who then prescribed medications for sleep and anxiety. The medications provided some relief, but did not make her insomnia and anxiety go away completely.
Joyce also noticed that her limbs were so stiff that she could no longer enjoy her hobbies, including gardening. “I’ve had replacement of a knee,” said Joyce. “Most people recover, but my knee surgery recovery was two years. The muscle felt like it was burning.”
Joyce’s symptoms peaked in the summer of 2023 with extreme fatigue, depression, blurry vision, and brain fog. She had a fear of falling after 2-3 rough falls, which resulted in Joyce limiting her movement as much as possible. “It was a gradual progression for years,” said Joyce. “I was stumbling. I was ready to give up the nonprofit.”
“I am a biology major and I know the function of the pituitary gland. I know it controls so many organs in my body, and mine wasn’t doing anything.”
Joyce also experienced severe allergic reactions to everything, including mosquito bites. Finally, Joyce went to the emergency room where a CT scan and MRI showed a 3 cm pituitary adenoma with optic chiasmal compression. When she was discharged, she was referred to UNC Health endocrinologist, Dr. Atil Kargi.
Joyce admits that she was cautious going into her first consultation with Dr. Kargi. At this point, she had been struggling with debilitating symptoms for years and was desperate for answers. After imaging and bloodwork, Dr. Kargi confirmed the presence of a tumor on her pituitary gland. “It was a huge relief,” said Joyce. “I am a biology major and I know the function of the pituitary gland. I know it controls so many organs in my body, and mine wasn’t doing anything.”
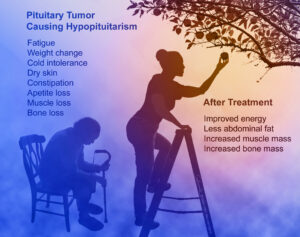
Dr. Atil Kargi and pituitary tumor surgeon Dr. Nelson Oyesiku discussed Joyce’s tumor and determined that it would be best to treat the tumor and hormone abnormalities with medication rather than surgery. “She has responded to treatment in amazing fashion,” said Dr. Kargi. “She was suffering from symptoms for many years until the elusive diagnosis of prolactinoma and hypopituitarism were arrived at and addressed.”
Dr. Kargi is a neuroendocrinologist at UNC Health and frequently sees patients that go undiagnosed for years before receiving a proper diagnosis and referral. “It would be easy to miss the prolactinoma and hypopituitarism during checkups or evaluations for her symptoms by general doctors,” said Dr. Kargi. “But after menopause, these symptoms should not happen. In younger women the high prolactin would have likely been noticed, but since older women do not get symptoms from high prolactin after menopause, it would not be checked or thought of.”
Joyce’s hormone deficiencies were low cortisol and low thyroid. Cortisol is not part of a routine lab panel and is rarely checked. Thyroid levels are often checked at routine physicals and were checked by Joyce’s primary care provider before the tumor was discovered. However, the thyroid test used to diagnose thyroid disease is different than the thyroid test used to diagnose low thyroid levels caused by pituitary disease, so hypothyroidism due to hypopituitarism often gets missed during screening tests. “Since thyroid disease is much more common than pituitary disease, the medical community is generally ‘okay’ with the common thyroid screening test called TSH, but to diagnose hypopituitarism a free T4 needs to be measured along with the TSH level,” said Dr. Kargi.
Dr. Kargi also explained that it is common in older patients to consider the symptoms of hypopituitarism as signs of normal aging. “If not assessed with the correct lab tests, the diagnosis is very often delayed or missed,” said Dr. Kargi. “Many of our patients only get diagnosed with the hormone deficiencies after a surreptitious finding of tumor or MRO leads us to check the hormones.”
“It’s like someone turned the clock back on my life 10-15 years. I’m not always cold. I’m not crying all the time.”
After a couple months of medication, imaging now shows that the tumor is shrinking. Joyce has noticed a drastic improvement in the symptoms that made day-to-day life feel impossible. “Dr. Kargi has been working with me and it’s like a new life for me,” said Joyce. “It’s like someone turned the clock back on my life 10-15 years. I’m not always cold. I’m not crying all the time.”
Joyce also noticed significant improvement in her balance and memory. She has lost over 25 pounds without having to work as hard as she has in the past to lose weight. She no longer needs to take anxiety medication. “I’m a black female, and I think that lots of times, because blacks are not involved in a lot of case studies, often they just don’t trust doctors as much as they should,” said Joyce. “I want individuals of color to realize that an endocrinologist can help with some of these issues.”
The medication has also allowed Joyce to continue her nonprofit work, and she has plans to expand the organization’s work. She’s returned to gardening and works on her family’s farm. “My primary care physician is great, but he did not dig deep enough,” said Joyce. “You say you hurt or you’re forgetful and people say you’re just getting older. They need to look deeper into the problem instead of just saying it’s aging.”
Joyce hopes that by sharing her story, she can help other patients come to the right diagnosis sooner, rather than having to wait years for answers and treatment. “The endocrine system is not a widely recognized system within the lay population,” said Joyce. “The symptoms of deficiency in that system can be overlooked.”
Joyce plans to continue working on her overall health by increasing her flexibility, dancing, and playing with her grandchildren. “I want to get my body back to physical shape,” said Joyce. “I want to get back to the things that I used to do that were fun.”