

Vibhor Krishna, MD
Vice Chair, Inpatient Operations
Service Line Leader
Associate Professor
With decades of experience in the field, our Deep Brain Stimulation Therapy (DBS) Program aims to provide personalized treatment options for patients whose symptoms have not been effectively treated through traditional approaches such as medications, occupational therapy, or physical therapy. UNC Health performed its first DBS surgery in 2004. Since then, our team has performed over 1,000 DBS surgeries.
Our program offers DBS for the following conditions:
Parkinson’s disease
Tremor
Dystonia*
Epilepsy
Obsessive Compulsive Disorder*
*DBS for dystonia and obsessive compulsive disorder are offered based on an approval from the Food and Drug Administration’s (FDA) Humanitarian Device Exemption.
Our neuromodulation team is among the most comprehensive and collaborative in the nation, offering a patient centered experience starting with you and your existing care team. DBS candidacy is and should be a personalized process for every patient, and this mission is clearly shared by our team of movement disorder specialists, functional neurosurgeons, neuropsychologists, nurse coordinators, and multiple other care partners. DBS patients at UNC Health have two dedicated nurse navigators, Kelsey Wertman and Wes Crutchfield, to guide them through their care.
In DBS surgery, electrodes (made of insulated wires) are implanted into a specific, deep target location within the brain. The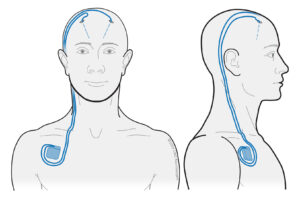 target location is personalized to treat patient-specific symptoms. These wires are connected to an extension cable that runs behind the ear, down over the collarbone, with a pacemaker installed below the collarbone. The entire system lies under the skin, with the pacemaker delivering a constant, fast-frequency stimulation to the brain . This stimulation modulates specific brain circuits involved with different neurological conditions.
target location is personalized to treat patient-specific symptoms. These wires are connected to an extension cable that runs behind the ear, down over the collarbone, with a pacemaker installed below the collarbone. The entire system lies under the skin, with the pacemaker delivering a constant, fast-frequency stimulation to the brain . This stimulation modulates specific brain circuits involved with different neurological conditions.
After the DBS system is installed, a neurologist programs the electrical stimulation settings using a special communication device, allowing them to personalize settings aimed at improving specific symptoms. An overwhelming majority of patients who qualify for and undergo DBS surgery experience a remarkable improvement in symptoms as well as in their quality of life.
In order to provide highly-specialized and successful care through the UNC DBS program, we rely on the close-knit partnership and multidisciplinary care offerings of several medical specialties; including but not limited to neurology, neurosurgery, neuropsychology, radiology, and anesthesiology. We discuss and treat every patient individually prior to offering surgery in order to meet our patients’ specific needs and to maximize their clinical improvement.
We recommend that all patients first be evaluated by one of the neurologists from the Movement Disorders Center at UNC Health. During the evaluation, the movement disorders specialist will confirm the disease or condition causing involuntary movement and if the patient may be a candidate for deep brain stimulation surgery at UNC Health.
Once DBS is being considered, our interdisciplinary team of specialists discuss the patient’s history, examination, expected benefits, and unique risks for undergoing surgery. Considerable time and effort is placed to ensure that the team’s recommendations are personalized to the patient’s case and needs. We then communicate this information back to the patient.
If a qualifying patient then decides to proceed with surgery, the following steps are taken:
Patients are first seen during a consultation visit with a neurologist on our team. To schedule a consultation visit at the Movement Disorders Center at UNC Health in Chapel Hill, please call (984) 974-4401.
Care providers can fax referrals to 984-974-2287.


Vice Chair, Inpatient Operations
Service Line Leader
Associate Professor
Director, UNC Movement Disorders Neuromodulation Program
Associate Professor, Movement Disorders
Vice Chair, Ambulatory Affairs
Vice Chair of Faculty Affairs
Residency Program Director
Section Chief of Functional Neurosurgery
Professor


Assistant Professor, Neuropsychology
Joseph & Hannah Baggett Distinguished Professor, Movement Disorders


Functional Neurosurgery Nurse Coordinator
Assistant Professor, Movement Disorders
DBS is most effective for two sets of symptoms in Parkinson’s disease patients:
DBS can be easily adjusted from the physician programmer and does not require another surgery if the patient’s condition changes. This remarkable technology allows our neurologists the lifelong ability to adjust stimulation and provides the opportunity to constantly improve patient’s Parkinson’s disease symptoms.
The majority of Parkinson’s disease patients will still need to take medication after DBS surgery, but some may be able to lessen the number of medications taken. Medications will often be useful to improve other symptoms not address by DBS surgery.
DBS is available to improve Essential Tremor symptoms; the most common cause of tremor in the world. For most patients, the degree of tremor improvement is well above the benefits of available medications on the market.
DBS can be easily adjusted from the physician programmer and does not require another surgery if the patient’s condition changes. This remarkable technology allows our neurologists the lifelong ability to adjust stimulation and provides the opportunity to constantly improve patient’s tremors.
It is common for many DBS programs to offer Essential Tremor patients a “staged” procedure. This means that one side of the brain receives the DBS implant first, with stimulation capable of affecting one hand. Months to years later, it is then decided whether to implant the opposite side of the brain to impact tremor on the other hand. This can require implantation of 2 pacemakers, one for each side of the brain.
UNC is proud to offer DBS surgery with implants to both side of the brain at the same time (for qualifying patients). Through the efforts of our dedicated group of subspecialists in tremor management, we have found that this method highly reliable tremor improvement to both hands with only one brain surgery and only the need for one pacemaker to provide stimulation.
While DBS is not a cure for essential tremor, it can improve a patient’s ability to improve daily activities, including but not limited to dressing, bathing, driving, use of technological devices, handwriting, eating, and drinking among other fine motor skills.
Dystonia is a movement disorder that causes muscle contractions that then cause repetitive or twisting movements and postures. Dystonia can affect one or more parts of the body; focal dystonia affects only a specific part of the body, while generalized dystonia affects most or all parts of the body.
Dystonia can become disabling due to impairment of motor skills and/or significant pain from contractions. There are multiple medications along with botulinum toxin that can effectively treat focal dystonias. However, when medications or other non-surgical therapies are not successful or insufficient to provide meaningful relief of muscle contractions, DBS may be an effective treatment option; FDA-approved for both generalized and focal dystonia.
The FDA has provided a humanitarian-device exemption to approve DBS for dystonia on a limited basis. Specialized centers like UNC are required to keep track of specific symptoms and other factors while offering DBS for dystonia; this information is kept by the FDA to help them decide on how and whether to continue to support the approval for surgery.
Dr. Robert McClure in the Department of Psychiatry works with the DBS team to determine if a patient with obsessive compulsive disorder (OCD) may be a candidate for DBS. UNC Health was one of the first centers in the United States to perform DBS for OCD.
Potential candidates for DBS surgery are patients with OCD that are severely resistant to multiple medications and behavioral therapies. Research has shown that DBS may be a promising therapy for these patients.
The FDA has provided a humanitarian-device exemption to approve DBS for OCD on a limited basis. Specialized centers like UNC are required to keep track of specific symptoms and other factors while offering DBS for OCD; this information is kept by the FDA to help them decide on how and whether to continue to support the approval for surgery.
Members of the UNC Movement Disorders Center participate in ongoing deep brain stimulation research and movement disorders research to improve patient care and treatment options available to patients. Each member of the DBS team at UNC Health has published extensively, summarizing their promising research.
Learn about ongoing research on each provider’s individual lab website:
Krishna Lab
Publications by Dr. John Younce
Publications by Dr. Daniel Roque
Publications by Dr. Robert McClure
Publications by Dr. Vibhor Krishna