Tremor Interdisciplinary Clinic
The mission of the Tremor Interdisciplinary Clinic is to provide an educational, consultative set of assessments and recommendations to participants and their local, referring care teams who seek to better understand the nature of and management options for their tremor syndromes.

Essential tremor (ET) and Parkinson disease (PD) remain the most common movement disorders and also the top 2 causes of involuntary tremor. Telling the difference between these tremor types — let alone other causes of tremor — can prove difficult even for movement disorder specialists who attempt to discern and classify them. Tremor in ET and PD are often rendered medically-refractory within as little as 1 year of initiating available medications on the market. Patients suffering from tremor are only occasionally referred to allied health professionals like occupational therapists for adaptive training: a lost opportunity considering a growing number of adaptive and wearable devices on the market. Deep brain stimulation (DBS) and focused ultrasound ablation (FUSA) surgeries are approved for tremor reduction in both ET and PD, but require dedicated teams of neurologists, neurosurgeons, and other healthcare professionals to effectively communicate expectations to patients and the referring community at large, let alone coordinate the procedures effectively. Lastly, in order to investigate future insights into diagnosing and treating tremors, this requires a team-based approach with basic science researchers to engage in translational research opportunities within clinical settings, using a number of tools available for tremor analysis.
At UNC Neurology, we recognize the excellent work performed by so many of these professionals independently studying and treating tremor; yet through the innovative Tremor Interdisciplinary Clinic we aim to integrate their work through a single interdisciplinary care approach. Through this effort, we strive to provide the same benefits offered by the individual team member, truly enhanced through effective team communication during a single evaluation by all members of the clinic. The Tremor Interdisciplinary Clinic provides a unique set of consultative visits with recommendations for patients and their ongoing care providers to offer guidance towards both the highest level of available care while reviewing options to engage in cutting edge opportunities for tremor treatment.

What would my visit to the Tremor Interdisciplinary Clinic look like?
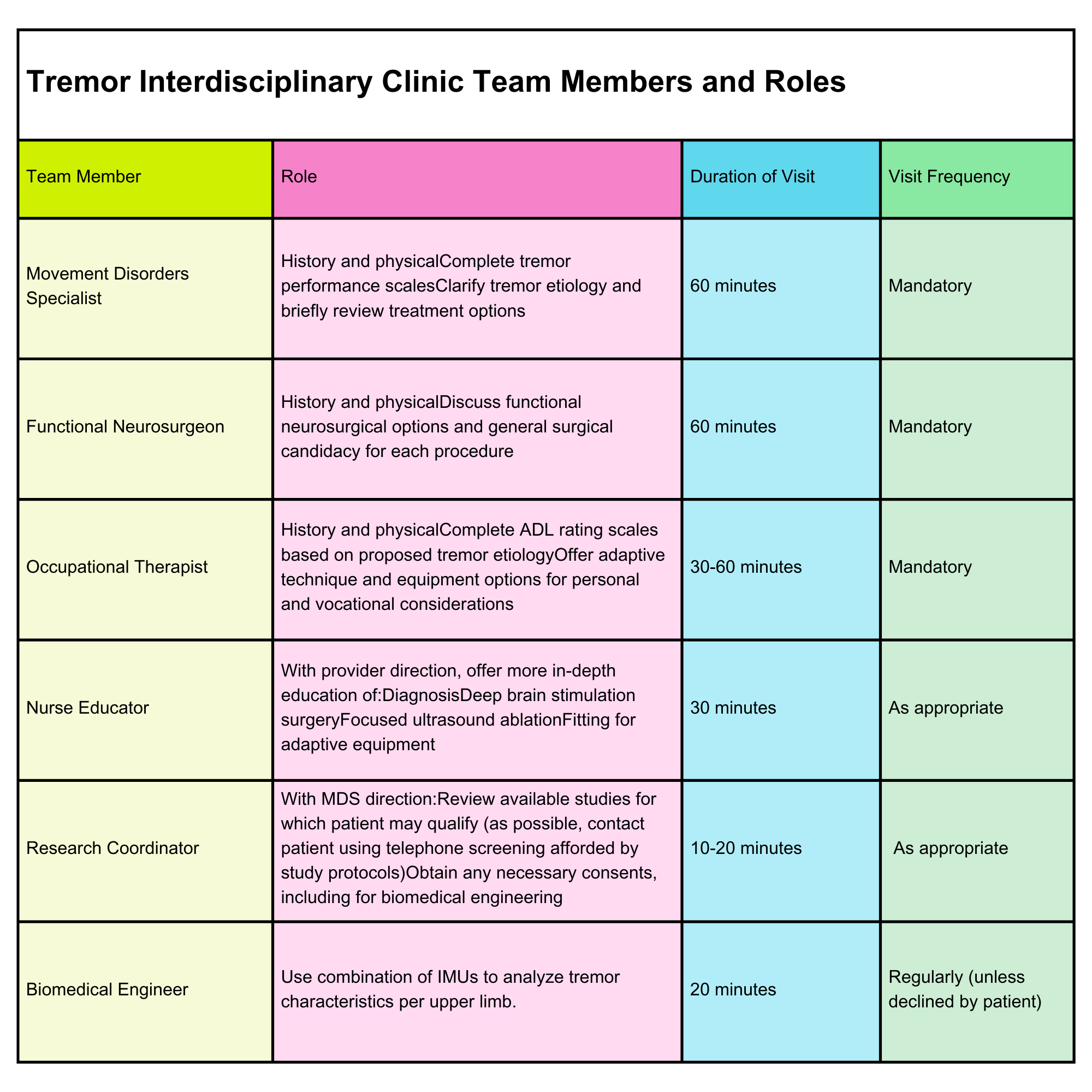
Patients are scheduled for a 4-hour session with multiple evaluations. Each participant is seen by at least 3 team members: our neurologist, our neurosurgeon, and our occupational therapist. The last hour of evaluation for each participant is flexible and designed to cater to the needs and interests of the person; such that they may be offered opportunities to participate in available research and be provided with additional education regarding their individual diagnosis and/or treatment options available to them. We also hope to measure all tremors with the assistance of tools available to our biomedical engineering colleagues, though this is will only be completed with each patient’s permission in advance.
Interdisciplinary, guidance, recommendations, and take home points
Once all in-person evaluations have occurred, time is spent by all team members discussing individual evaluations per participating patient. Subjective reports, objective findings, clinical opinions, and treatment considerations are reviewed through collaborative discussion. Clinical and ethical questions and concerns are raised as appropriate, resulting in a series of recommendations which are then drafted into a comprehensive clinic document for the use of patients and referring providers.
It is largely the intent of this clinic to be consultative in nature and as such patients are encouraged to return to their previously-treating healthcare professionals. Given the fact that our center does offer more advanced therapeutic options (including deep brain stimulation surgery, focused ultrasound ablation surgery, professional connections to adaptive equipment manufacturers, and research opportunities), ongoing professional relationships with Tremor Interdisciplinary Clinic participants are certainly possible but not the primary goal of the evaluations. This helps us ensure adequate access to our clinic for prospective, future participants.